Depression is a disabling disease Reference Sobocki, Jönsson, Angst and Rehnberg1 causing problems such as a reduction in quality of life and loss of general functioning. Reference Lönnqvist2 In Finland, depression has become a common reason for inability to work Reference Lönnqvist2 and is prevalent in 5–6.5% of the population. Reference Tuulari, Aromaa, Herberts and Wahlbeck3 Medication together with psychiatric counselling is the most common combination in the treatment of depression. Psychotherapy has also been found to be effective, Reference Isometsä, Jousilahti, Lindfors, Luutonen, Marttunen and Pirkola4 but verbal psychotherapy processing may be difficult or insufficient for some individuals. Therefore, therapies that allow non-verbal processing – such as music therapy – may offer a workable alternative. Music can then be seen as an alternative expressive modality and a way to get in touch with emotions and develop relationships. Reference De Backer5,Reference Gold, Heldal, Dahle and Wigram6 Free improvisation, a specific music therapy technique, has also been described as a means of ‘self-projection and free association’ Reference Hadley and Hadley7 enabling one to connect with emotional memories and images. Reference Erkkilä8–Reference Erkkilä, Ala-Ruona, Punkanen, Fachner, Hargreaves, Miell and MacDonald10 In recent years, some randomised controlled trials (RCTs), a Cochrane systematic review Reference Maratos, Gold, Wang and Crawford11 and a meta-analysis Reference Gold, Solli, Krüger and Lie12 focusing on dose–response relationships in music therapy for people with serious mental disorders (including depression) have found music therapy to be an effective treatment for depression, for example, improving mood and being easily accepted by individuals. Reference Erkkilä, Gold, Fachner, Ala-Ruona, Punkanen and Vanhala13 However, better methodological quality with more focus on clinical theories and working modes of music therapy has been demanded. Only one study Reference Radulovic14 focused on people of working age. The present study focused on a single clinical method with a clear clinical theory (improvisational, psychodynamic music therapy), a combination that is relevant in music therapy practice. Reference De Backer5,Reference Erkkilä9,Reference Erkkilä, Ala-Ruona, Punkanen, Fachner, Hargreaves, Miell and MacDonald10,Reference Eschen15–Reference Priestley17 We limited our study to working-age people because of the huge socioeconomic importance of this large population, Reference Lönnqvist2,Reference Honkonen, Aro, Isometsä, Virtanen and Katila18 and because of the dearth of research in this area. Reference Maratos, Gold, Wang and Crawford11
Method
Participants
The sample consisted of 79 adults with unipolar depression, ranging from 18 to 50 years of age. Inclusion criteria required that their primary diagnosis was depression, F32 or F33, according to ICD–10 classification. 19 The Structured Clinical Interview for DSM–III–R (Mini-SCID) Reference Spitzer, Williams, Gibbon and First20 was used in health centres and polyclinics for diagnosing depression. In addition, a masked clinical expert (I.P.) with specific training in diagnosing depression assessed all the participants before randomisation. Anxiety was included because of the frequent comorbidity of depression and anxiety. Reference Aina and Susman21,Reference Cassidy, Lauderdale and Sheikh22 Clients were included irrespective of medication status and were allowed to continue medication during the study. Musical skills or any given musical background were not required, although these did not exclude clients from participation. Clients were excluded if: they had a history of repeated suicidal behaviour or psychosis; they had acute and severe substance misuse; the severity of depression prevented them from participating in the measurements or engaging in verbal conversation; or they had insufficient knowledge of the Finnish language.
The study was conducted at the Music Therapy Clinic for Research and Training, University of Jyväskylä, Finland. Trial registration: ISRCTN84185937.
Recruitment began in February 2008 and continued until April 2009. Participants were recruited primarily from the Central Finland Health Care District’s psychiatric health centres and the psychiatric polyclinics of Jyväskylä city. Clinicians at these centres identified potential participants among their patients and gave them information about the study. When these patients contacted us, a clinical expert (I.P.) evaluated them based on the inclusion and exclusion criteria. Newspaper advertisements were launched to boost recruitment. Further details of the flow of participants are provided in Fig. 1. The ethical board of the Central Finland Health Care District gave their approval for the study on 24 October 2007. In addition, all participants gave signed informed consent to the study.
Randomisation
Participants were randomised using simple randomisation with a 10:7 ratio of standard care to music therapy (details in Fig. 1). This unequal ratio was chosen to maximise feasibility and power within the given budget and time constraints. An independent person at Uni Health, Bergen, Norway, generated the randomisation list using a spreadsheet software program and kept each participant’s allocation concealed from the investigators until a decision about inclusion was made. Once all baseline data had been collected and informed consent obtained, the investigators used email to receive the allocation for the respective participant. After randomisation the participants were considered part of the study regardless of whether they decided to leave the study prematurely (intention-to-treat principle).
Assessment procedure
Psychiatric assessments were conducted at baseline and at 3- and 6-month follow-up, where 3-month follow-up took place immediately after the intervention in the music therapy group, and the 6-month follow-up 3 months after the treatment had been completed.
One masked clinical expert (I.P.), with training in psychiatric nursing and long experience in psychiatry, conducted all the psychiatric assessments. The expert had in addition specific
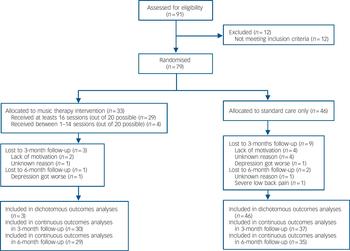
Fig. 1 Flow chart of study participants.
training in the treatment and assessment of depression based on collaborative care for depression (psychiatric nurses working at healthcare centres with special training in depression treatment), Reference Bower, Gilbody, Richards, Fletcher and Sutton23 which is applied in some healthcare districts in Finland, including Jyväskylä. The assessor was masked to the participants’ group assignment, and the evaluations were conducted in another physical setting outside the clinic in order to avoid accidental meetings with the members of the music therapy group. The assessor was excluded from meetings at which the masking could have been endangered. Any instances of broken masking were reported.
Outcome measures
Primary outcome
The primary outcome measure of the study was the Montgomery–Åsberg Depression Rating Scale (MADRS). Reference Montgomery and Åsberg24 It consists of 10 items and the total score can vary from 0 to 60. The MADRS has high joint reliability, its sensitivity to change has been shown in several studies and its predictive validity for major depressive disorder has been demonstrated. Reference Rush, First and Blacker25
Secondary outcomes
The secondary outcome measures administered were the anxiety part of the Hospital Anxiety and Depression Scale (HADS–A), Reference Zigmond and Snaith26 Global Assessment of Functioning (GAF), Reference Hall27,Reference Jones, Thornicroft, Coffey and Dunn28 the health-related quality of life survey RAND–36 Reference Aalto, Aro and Teperi29 for measuring quality of life, and Toronto Alexithymia Scale (TAS–20) Reference Taylor, Ryan and Bagby30 for evaluating alexithymia. The measures of general functioning and quality of life were chosen on the basis of their wide use in studies of psychological interventions for people with mental health problems. Alexithymia was considered in this study because it typically occurs with depression. Reference Honkalampi, Hintikka, Laukkanen, Lehtonen and Viinamäki31 Treatment response was calculated as a 50% or greater decrease in MADRS score.
Electroencephalographic biomarkers were included as additional outcomes to research the impact of music therapy on brain processing of (negative) emotions, especially in frontal areas, but these will be reported separately.
Intervention
All participants (in both the music therapy and the control group) continued to receive treatment as usual while participating in the study.
Control group: treatment as usual
In the Central Finland Health Care District, standard care included a short-term psychotherapy intervention (5–6 individual sessions) conducted by nurses specially trained in depression, medication (antidepressants) and psychiatric counselling (appointments for advice, follow-up and support when needed). The use of medication was reported.
Music therapy group: individual music therapy plus treatment as usual
Music therapy is a form of therapy that uses music experiences and client–therapist relationships for the purpose of therapeutic change. Reference Gold, Solli, Krüger and Lie12 The music experiences used in music therapy may be varied and can range from listening to music to playing or singing songs to free improvisation; the degree of verbal reflection used in therapy sessions and the degree of structure provided by the therapist may also vary. In this study, active (i.e. clients are asked to play) music therapy was offered in an individual setting (therapist–client) according to the clinical model Reference Erkkilä32,Reference Erkkilä33 developed at the Music Therapy Clinic for Research and Training, University of Jyväskylä. This model is based on an interaction between free musical improvisation and discussion, and is theoretically anchored in a psychodynamic music therapy tradition. Reference De Backer5,Reference Erkkilä8,Reference Erkkilä, Ala-Ruona, Punkanen, Fachner, Hargreaves, Miell and MacDonald10,Reference Eschen15–Reference Priestley17,Reference Bruscia34 The basic principle of the intervention is to encourage and engage clients in expressive musical interaction. The role of the therapist is to actively facilitate and support the client’s therapeutic process by using musical elements (i.e. rhythm, harmony, melody, dynamics, timbre) and interventions combined with reflective discussion. The therapeutic process is based on the mutual construction of meaning of emerging thoughts, images, emotional content and expressive qualities that often originate from the musical experience and are then conceptualised and further processed in the verbal domain. That psychodynamic theory is common in active music therapy may have arisen from conceptual commonalities between them – for example, some of the typical concepts of psychodynamics, such as emotion, metaphor, association and image, are also core elements of musical experiences. Reference Erkkilä, Ala-Ruona, Punkanen, Fachner, Hargreaves, Miell and MacDonald10,Reference Wigram, Nygaard Pedersen and Bonde35
A total of 20 bi-weekly music therapy sessions were offered, each session lasting 60 min (conducted between May 2008 and July 2009). Musical expression in the sessions was based on a restricted selection of music instruments, including a mallet instrument (a digital mallet midi-controller), a percussion instrument (a digital midi-percussion), and an acoustic djembe drum. The therapist and the client both had identical instrumentation. All the improvisations created in the sessions were recorded either as MIDI-data or as digital audio. This made it possible to play back the improvisations for further processing and discussion. Moreover, all the sessions were video recorded for research and supervision purposes.
Ten music therapists took part in the study (three female, seven male). They all had professional training in music therapy following the highest Finnish music therapy training standards. During the study the clinicians received frequent supervision (group based, 2 monthly sessions throughout the study, presence was consistent across the clinicians) by an experienced and trained supervisor with qualifications in music therapy and psychotherapy. In case of specific questions a psychiatrist was available for consultation.
For treatment fidelity, the therapists participated in extensive training Reference Erkkilä33 before the study, lasting for 15 months. The aim of the training was to achieve a common understanding about the theoretical and clinical fundamentals behind the clinical model, and to further develop the therapeutic expertise needed in the study. Lectures, real-time peer observation of the rehearsing sessions and reflective group work were used as a primary training method. During the study, video recordings of the clinical sessions were used frequently in supervision both for monitoring adherence to the method and competence in its application.
Statistical analysis
Sample size was determined using the results of a previous systematic review of dose–effect relationships in music therapy with mental disorders, from which the expected standardised mean difference of 15 sessions of music therapy for depression was predicted as 0.75. Reference Gold, Solli, Krüger and Lie12 We assumed that clients would attend at least 15 sessions on average, and that no more than 10% of participants would leave the study early. We arrived at 88% power for the primary outcome, with a sample size of n = 85 (control group, 50 and music therapy group, 35; details in the study protocol). Reference Erkkilä, Gold, Fachner, Ala-Ruona, Punkanen and Vanhala13
Data from patient notes and interviews were entered into spreadsheet files and checked independently by another person. Analyses were conducted using R (version 2.7.2 for Mac). All analyses were intention-to-treat. For dichotomous outcomes, this meant that we assumed the negative outcome when the information was missing. For continuous outcomes, intention-to-treat meant that we retained data from all participants for whom the information was available. Full intention-to-treat including all randomised participants is not possible for continuous outcomes. Multiple imputations is not recommended when data are missing on dependent but not on independent variables, as it would only serve to increase standard errors. As a sensitivity analysis for the primary outcome, we assumed no change for those where the outcome was unobserved. Distributions of scores and change scores were examined graphically, and if unusual outliers were found they were excluded in a sensitivity analysis.
We calculated Fisher’s exact test and odds ratios with 95% confidence intervals for dichotomous outcomes, and Welch’s t-test with 95% confidence intervals for changes in continuous outcomes. All tests were two-tailed. After obtaining these results, we also calculated the number needed to treat (NNT) and standardised mean difference (Cohen’s d) to facilitate interpretation of clinical significance. Exploratory regression analyses were conducted to examine the possible influence of severity of depression (three levels), anxiety (yes/no), age (continuous), antidepressant medication status (yes/no), and being self-described as a musician (yes/no) or singer (yes/no). Predictors were each entered separately. The dependent variables were change in MADRS scores (linear model) and response rate (logistic model). The interaction between the treatment condition and each predictor was examined to identify whether any of these predictors had an influence on the treatment effect. Similarly, the therapist was examined as a predictor within the music therapy group.
Results
During the study period, 91 people were screened, of whom 79 (87%) were eligible to participate in the study. No eligible patients refused to participate in the study and therefore 79 people (100% of eligible patients) were randomised (Fig. 1). In total, 62 (78%) were female; ages ranged from 18 to 50 years (mean 35.65). Of the participants, 33 were randomised to music therapy. Baseline characteristics in each arm of the trial, including medication status, are shown in Table 1. No significant difference was found on any of these characteristics.
A total of 12 participants dropped out before the 3-month follow-up and another 3 before the 6-month follow-up. The drop-out rate was higher in the control group (Fig. 1). The reasons for dropping out were lack of motivation (n = 6), health issues (n = 3) or unknown reasons (n = 6), i.e. the participants did not respond to the contact attempts. Among those who were followed up at 3 months, medication status was mostly unchanged.
The assessor became aware of group allocation unintentionally for two participants (the participants reported their allocation to the assessor), and for one participant intentionally (because of an adverse event).
On average, the participants assigned to the music therapy group received 18 music therapy sessions (s.d. = 4.7, range 1–20). A total of 29 (88%) received at least 15 sessions. None of those in the control group received any music therapy. Therapy was provided by one of ten music therapists (three female) in a one-to-one setting.
During the therapy process, participants created on average 21.8 (s.d. = 12.9, range 1–59) improvisations. The majority of the improvisations (mean 18.6, s.d. = 11.7, range 1–53) were therapist–client duets, but there were also solo improvisations by the clients (mean 3.2, s.d. = 3.2, range 0–9). In total, 721
Table 1 Baseline characteristics of 79 patients randomised to music therapy or standard care
| Characteristic | Music therapy group (n = 33) | Control group (n = 46) | Mean difference (95% CI) | Odds ratio (95% CI) | P a |
|---|---|---|---|---|---|
| Age: years, mean (s.d.) | 35.8 (9.0) | 35.5 (10.5) | 0.21 (–4.60 to 4.17) | 0.92 | |
| Female, n (%) | 25 (75.8) | 37 (80.4) | 1.31 (0.38 to 4.43) | 0.78 | |
| Diagnosis, b n (%) | 0.77 | ||||
| F32.0 Mild depressive episode | 8 (24.2) | 15 (32.6) | |||
| F32.1 Moderate depressive episode | 17 (51.5) | 21 (45.7) | |||
| F32.2 Severe depressive episode without psychotic symptoms | 8 (24.2) | 10 (21.7) | |||
| Anxiety (cut-off score 8 in Hospital Anxiety and Depression Scale – Anxiety) | 28 (84.8) | 35 (76.1) | 0.40 | ||
| Musical background (self-reported), n (%) | |||||
| Sings | 11 (33.3) | 12 (26.1) | 1.41 (0.47 to 4.21) | 0.62 | |
| Plays an instrument | 14 (42.4) | 13 (28.3) | 1.86 (0.66 to 5.33) | 0.23 | |
| Has musical training | 7 (21.2) | 6 (13.0) | 1.78 (0.46 to 7.21) | 0.37 | |
| Self-described as a musician/singer | 9 (27.3) | 8 (17.4) | 1.77 (0.52 to 6.08) | 0.41 | |
| Current medication (self-reported), n (%) | |||||
| Any antidepressant medication | 22 (66.7) | 35 (76.1) | 0.63 (0.21 to 1.91) | 0.45 | |
| Selective serotonin reuptake inhibitors | 16 (48.5) | 20 (43.5) | 1.22 (0.45 to 3.30) | 0.82 | |
| Serotonin and noradrenaline reuptake inhibitors | 5 (15.2) | 9 (20.0) | 0.72 (0.17 to 2.71) | 0.77 | |
| Psychiatric test scores, mean (s.d.) | |||||
| Montgomery–Åsberg Depression Rating Scale score | 24.6 (6.4) | 23.0 (7.6) | 1.61 (–4.74 to 1.53) | 0.31 | |
| Hospital Anxiety and Depression Scale – Anxiety score | 11.2 (3.5) | 10.3 (3.9) | 0.98 (–2.66 to 0.70) | 0.25 | |
| Global Assessment of Functioning score | 58.5 (6.4) | 59.5 (8.0) | 0.96 (–2.27 to 4.19) | 0.55 | |
| Toronto Alexithymia Scale score | 52.5 (12.4) | 51.2 (11.3) | 1.27 (–6.73 to 4.20) | 0.64 | |
| Health-related quality of life survey RAND–36 score | 50.5 (15.3) | 52.6 (13.9) | 2.05 (–4.66 to 8.76) | 0.54 | |
a Welch's t-test for continuous outcomes, Fisher's exact test for dichotomous outcomes.
b Based on Montgomery–Åsberg Depression Rating Scale cut-off scores (up to 19, mild; 20–29, moderate; 30 or greater, severe).
improvisations (615 duets, 106 solo improvisations) were recorded over 596 sessions and are available for further analysis.
Tables 2 and 3 compare outcomes in each arm of the trial. Changes in MADRS, HADS–A, and GAF scores were significantly greater in the music therapy group than in the control arm of the trial. Modest differences in secondary outcomes as well as in 6- month follow-up assessments did not reach statistical significance. However, graphical analysis suggested that differences between the groups tended to persist at 6 months for all five psychiatric measures (Fig. 2). The chances of response at 3 months were significantly greater with music therapy than with standard care (odds ratio (OR) = 2.96; Table 3). This difference was not significant anymore at 6 months. Drop-out rates tended to favour the music therapy arm but did not reach significance. We transformed the identified effects into effect sizes (standardised mean differences) and calculated NNT to facilitate clinical interpretation (Table 4). These effect sizes are based on the intention-to-treat analysis as defined earlier. We conducted two sensitivity analyses. The first, conducted for MADRS change scores, assumed no change for those participants where the outcome was unobserved at 3 months, in order to provide a conservative estimate based on all participants initially randomised. The effect was still significant (P<0.05). Second, a per-protocol analysis with one outlier excluded was conducted for all outcomes. This analysis tended to show larger effect sizes than the intention-to-treat analysis, but statistical significance levels were unchanged (not shown).
We conducted pre-planned exploratory regression analyses of change in MADRS scores and logistic regression analyses of response rates to identify potential predictors of change. Severity of depression, presence of anxiety, age, being on antidepressant medication and being self-described as a musician or a singer, were each entered separately. None of these potential predictors showed a significant interaction with the assigned group. Within the music therapy group we examined whether the therapist was a significant predictor; no such influence was identified.
Table 2 Changes in primary and secondary outcomes in the music therapy group and control group from baseline to 3 and 6 months (intention-to-treat): continuous outcomes
| 3-month follow-up, (n = 67) a | 6-month follow-up, (n = 64) b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Mean (s.d.) | Change from baseline Mean | Mean difference (95% CI) | t-test | P | Mean (s.d.) | Change from baseline Mean | Mean difference (95% CI) | t-test | P |
| Montgomery–Åsberg Depression Rating Scale | ||||||||||
| Control group | 16.43 (9.33) | –6.05 | 4.65 (0.59 to 8.70) | 2.29 | 0.03 * | 14.74 (10.65) | –6.97 | 3.44 (–1.05 to 7.94) | 1.53 | 0.13 |
| Music therapy group | 14.10 (8.77) | –10.70 | 14.48 (9.60) | –10.41 | ||||||
| Hospital Anxiety and Depression Scale – Anxiety | ||||||||||
| Control group | 8.00 (4.11) | –1.95 | 1.82 (0.09 to 3.55) | 2.11 | 0.04 * | 7.29 (4.75) | –2.46 | 1.65 (–0.38 to 3.67) | 1.63 | 0.11 |
| Music therapy group | 7.37 (3.99) | –3.77 | 7.21 (4.15) | –4.10 | ||||||
| Global Assessment of Functioning | ||||||||||
| Control group | 66.78 (9.61) | 6.92 | –4.58 (–8.93 to –0.24) | –2.11 | 0.04 * | 70.74 (12.64) | 10.06 | –4.56 (–10.48 to 1.35) | –1.54 | 0.13 |
| Music therapy group | 70.00 (9.37) | 11.50 | 72.90 (13.89) | 14.62 | ||||||
| Toronto Alexithymia Scale – 20 | ||||||||||
| Control group | 47.43 (11.99) | –4.05 | 2.05 (–2.35 to 6.44) | 0.93 | 0.36 | 45.77 (12.80) | –5.37 | 3.53 (–1.36 to 8.41) | 1.45 | 0.15 |
| Music therapy group | 45.83 (13.51) | –6.10 | 42.66 (12.20) | –8.90 | ||||||
| Health-related quality of life survey RAND–36 | ||||||||||
| Control group | 62.59 (18.20) | 9.86 | –4.50 (–11.40 to 2.40) | –1.30 | 0.20 | 64.60 (18.74) | 10.80 | –4.13 (–11.83 to 3.57) | –1.07 | 0.29 |
| Music therapy group | 66.70 (20.10) | 14.37 | 67.93 (18.51) | 14.93 | ||||||
a Control group n = 37; music therapy group n = 30.
b Control group n = 35; music therapy group n = 29.
* P < 0.05.
Table 3 Changes in primary and secondary outcomes in the music therapy group and control group from baseline to 3 and 6 months (intention-to-treat): dichotomous outcomesa
| 3-month follow-up | 6-month follow-up | |||||
|---|---|---|---|---|---|---|
| Outcome | n/N (%) | Odds ratio (95% CI) | P | n/N (%) | Odds ratio (95% CI) | P |
| Leaving the study early | ||||||
| Control group | 9/46 (20) | 0.42 (0.07–1.86) | 0.34 | 11/46 (24) | 0.44 (0.09–1.70) | 0.25 |
| Music therapy group | 3/33 (9) | 4/33 (12) | ||||
| Response b | ||||||
| Control group | 10/46 (22) | 2.96 (1.01–9.02) | 0.03 * | 16/46 (35) | 1.38 (0.49–3.82) | 0.64 |
| Music therapy group | 15/33 (45) | 14/33 (42) | ||||
a Missing information was treated as no response (intention-to-treat analysis).
b Response was defined as a 50% or greater reduction in Montgomery–Åsberg Depression Rating Scale symptom scores.
* P < 0.05.
Table 4 Clinical relevance of the effects of individual music therapy: effect sizes and number needed to treata
| Effect size, d | Risk difference, % | Number needed to treat | |
|---|---|---|---|
| Montgomery–Åsberg Depression Rating Scale | 0.65 | ||
| Hospital Anxiety and Depression Scale – Anxiety | 0.49 | ||
| Global Assessment of Functioning | 0.62 | ||
| Response | 24 | 4 | |
a All analyses intention-to-treat. Effect sizes were calculated as the difference in change at 3 months divided by the pooled standard deviation at baseline (Table 1), with signs reversed where applicable so that a positive effect size indicates a difference in favour of music therapy. Risk difference and number needed to treat are based on the numbers with no response at 3 months (Table 3).
Adverse events were noted for a few participants. Two participants (one in each arm of the trial) experienced a significant worsening of their depression, leading them to quit the study early; one participant in the control group developed severe low back pain (Fig. 1).
Discussion
This trial has shown that music therapy added to standard care helps people with mild, moderate or severe depressive episodes to improve their levels of depression as well as anxiety and functioning. The response rate was significantly greater in music therapy, compared with those who only received standard care. Effects were clinically relevant, with effect sizes in the medium-to-large range (ranging from 0.65 for depression to 0.49 for anxiety). The NNT was four, indicating that one person will change from no response to response for every four people to whom music therapy is offered. These estimates are based on an intention-to-treat analysis, which means that they are likely to underestimate the effects of treatment for those who received it. Another interesting finding is the high attendance rate. Average attendance of 18 sessions out of 20 shows a high level of engagement and sustained involvement.

Fig. 2 Changes in psychiatric tests. (a) Montgomery–Åsberg Depression Rating Scale; (b) Hospital Anxiety and Depression Scale – Anxiety; (c) Global Assessment of Functioning; (d) Toronto Alexithymia Scale – 20; (e) Health-related quality of life scale RAND–36.
* P<0.05.
Matching research and clinical methods
The main limitations of previous RCTs on music therapy for depression were that the clinical method was not clearly defined or was diverse; also, a typical working-age population were rarely included, and the methodological quality was generally poor. Reference Maratos, Gold, Wang and Crawford11 In particular, earlier music therapy research has suffered from an imbalance between research methods and clinical methods. Reference Erkkilä, Ala-Ruona, Punkanen, Fachner, Hargreaves, Miell and MacDonald10,Reference Gold, Solli, Krüger and Lie12,Reference Rolvsjord, Gold and Stige36 Flexible and process-oriented clinical methods that are prevalent in clinical practice have most commonly been investigated using qualitative process research. Conversely, quantitative research methods have been applied more commonly to highly structured clinical methods that music therapists do not commonly apply. Similar tendencies exist in psychotherapy research in general, where the effects of more structured approaches (e.g. cognitive–behavioural models) have also been more rigorously investigated than more process-oriented ones (e.g. psychodynamic psychotherapy). Reference Leichsenring and Rabung37 Yet the imbalance might have been even more extreme in music therapy, with the result that RCTs of music therapy methods that are commonly applied are rare and evidence for them is sparse. Reference Gold, Heldal, Dahle and Wigram6,Reference Maratos, Gold, Wang and Crawford11,Reference Gold, Solli, Krüger and Lie12,Reference Gold, Wigram and Elefant38 As the first RCT on improvisational music therapy for depression, the present study fills an important gap in knowledge and may also contribute to innovating the research culture in music therapy towards greater clinical applicability and relevance of outcome research.
Translation into clinical practice
The present study supports and further clarifies earlier clinical findings that suggested that music therapy has specific qualities that enable meaningful non-verbal expression and interaction even in those situations where the client cannot verbally describe their inner experiences. Reference De Backer5,Reference Erkkilä9 Clinical improvisation is said to be able to operate on a protosymbolic level Reference De Backer5 by triggering unconscious processes beyond the pathology and, in a way, to prepare the client for fully symbolic expression and eventually for verbalising. In this way musical interaction in music therapy can be seen as a preverbal Reference Rolvsjord39 or early Reference Erkkilä9 mode of communication, which may serve to extend and complement verbal expression and communication. For many clients in the music therapy group, experiences during the non-verbal act of musical expression led them to insights of certain aspects of their psychopathology as the experiences were further processed in the verbal domain. For example, it can happen in clinical improvisation that emotional memories about the domestic atmosphere in early childhood are triggered by musical interaction with the therapist. In general, the additional value of improvisational music therapy with these clients seemed to be that it enabled working with and experiencing emotions associated with depression on a symbolic, non-verbal level. Musical, improvisational interplay between the client and the therapist also offers an open stage for transferences and creative imagery.
Classical psychoanalytic thinking explains depression through traumatic events in one’s biography, often associated with dramatic losses and lack or deficit of love. Reference Freud40,Reference Rado41 Our study supports this viewpoint. Participants in music therapy often found reasons for their condition in past events and relationships based on their own initiative, even though clinicians were instructed not to manipulate clients in this direction.
That music therapy includes active doing – i.e. playing music instruments – was important to many clients. Inner pressure and feelings were often expressed by drumming or by the tones produced with a mallet instrument. Clients sometimes described their playing experience as cathartic, and this may have led to corrective emotional experiences in further processing. A rather unique property of music therapy is the fact that it includes the opportunity to be active and this seems to be a meaningful dimension for dealing with issues associated with depression.
We assume that the bi-weekly scheduling of sessions increased the intensity of the therapy and thereby contributed to positive outcomes. For research purposes, the clinical setting (instruments and clinical techniques available) was more restricted than in everyday music therapy practice. In our experience, however, this did not have a negative influence on the results.
Although not significant, the trend towards a reduction in alexithymia that was seen both at 3 and 6 months is interesting. Music therapy’s putative mechanisms of change, involving emotion recognition and expression, are directly related to the concept of alexithymia. Further research is needed to find out whether music therapy has an effect in reducing alexithymia in people with depression.
Limitations
The present trial was larger and more rigorous than previous studies, but might still be regarded as an exploratory trial in a statistical sense. The sample size was sufficient to detect an effect in the primary outcome at the end of therapy, but not at 6 months, even though graphical analyses suggested that the effect tended to persist. Second, the present trial used a simple two-arm design of music therapy with standard care versus standard care alone. It was designed to address the most policy-relevant question of interest, that is whether music therapy is superior to the usual treatment offered to that population, not to address the mechanism of change or the specific ingredients of music therapy. However, we examined whether the effect of music therapy varied significantly across therapists – a common criticism from common factors research in psychotherapy – and found no such indication. This lack of significant variation of effects between therapists might be an indication that the effect was based on the music therapy method utilised. Finally, an analysis of cost-effectiveness (or other health economic analysis) was not included in the present study, but would be useful and relevant for future studies. The achievement of the present study is to have demonstrated music therapy’s effectiveness over and above an already quite highly developed standard of care for people with depression.
Funding
The NEST (New and Emerging Science and Technology) programme of the European Commission (project BrainTuning ), and the programme for Centres of Excellence (CoEs) in research, Academy of Finland.
Acknowledgements
The authors would like to thank Tony Wigram for advice on the design of the study, Timo Männikkö for clinical supervision and collaboration, Petri Toiviainen for advice on the project management, Thomas Wosch for advice on alexithymia, Markku Pöyhönen for practical arrangements of the study, and Lasse Pulli for clinical supervision of the therapists. Geoff Luck and Fiona Kirkwood Brown have helped with language corrections.









eLetters
No eLetters have been published for this article.