High rates of suicide have been documented in India, Reference Joseph, Abraham, Muliyil, George, Prasad and Minz1–Reference Abraham, Abraham and Jacob4 and pose a major public health challenge. Reference Jacob5 These studies used the ‘verbal autopsy’ method (see below) in a population under surveillance as part of a comprehensive community health programme. The relative contributions of psychosocial stress and psychiatric morbidity to suicide are subject to debate. Whereas psychiatrists employing medical models and using Western data argue for psychiatric illness – especially depressive disorders – as causal for suicide, Reference Cavanagh, Carson, Sharpe and Lawrie6 work from low- and middle-income countries suggests social, economic and cultural factors as significant contributors. Reference Gururaj, Isaac, Subbakrishna and Ranjani7–Reference Cheng, Chen, Chen and Jenkins10 Epidemiological studies simultaneously investigating the combined effects of psychiatric and psychosocial risk factors for suicide are sparse. Available case–control psychological autopsy studies often recruit cases of suicide only from police or legal registers, employ non-probabilistic sampling, seldom use structured diagnostic interviews to categorise psychiatric morbidity and do not systematically study psychosocial stress or exclude confounders. Reference Khan, Mahmud, Karim, Zaman and Prince11–Reference Vijayakumar and Rajkumar13 We aimed to evaluate simultaneously the psychosocial and psychiatric risk factors for suicide, using structured interviews, in a rural Indian population under the surveillance of a comprehensive community health programme.
Method
We used a matched-pair case–control study to investigate the psychosocial and psychiatric risk factors for suicide.
Study setting
Kaniyambadi Block, Vellore District, is in the southern Indian state of Tamil Nadu. It is spread over 127 km2 and has 85 villages housing a total population of about 110 000. The majority of the population follow the Hindu religion and are from the lower socioeconomic strata. Agriculture and animal husbandry are the major occupations. The Department of Community Health at the Christian Medical College, Vellore, has been operating a community health programme in this block for the past five decades.
Surveillance system
The surveillance system, described elsewhere in detail, Reference Joseph, Joseph and Kamaraj14 consists of a four-tier monitoring system. The block is divided into regions with specific personnel in charge of the health of the different regions. The system involves a health team comprising a community health worker, health aide, community nurse and doctor. Every week the community health worker reports to the health aide about pregnancies, deliveries, births, deaths, morbidity, marriages, immunisation and couples eligible for contraception in the village. The health team in charge of the region verify and confirm the information. Data obtained by the surveillance system are computerised. Each person living in the block has an individual identification number. The data for the whole block are collated and reviewed monthly by all members of the department.
All deaths in the block are investigated using a verbal autopsy, a procedure used since 1985 to obtain mortality statistics. Reference Joseph, Abraham, Muliyil, George, Prasad and Minz1–Reference Abraham, Abraham and Jacob4 It is based on the assumption that most causes of death have distinct symptom complexes, and that these can be recognised, remembered and reported by respondents. It also assumes that it is possible to classify deaths, based on the reported information, into useful categories of causes of death. The community health worker who lives in the village and the health aide provide mortality data. The health worker, being part of the community, has access to detailed and reliable information on the circumstances of death, and will be aware of situations in which death by suicide is officially reported as accident or illness. The community health worker, health aide, community nurse and the doctor in charge of the village evaluate the details and circumstances of the death. Information is obtained from relatives of the dead person, the neighbours, traditional healers and village leaders. Information from the person's health records is also examined. The community health team arrives at a consensus on the nature of death. The system employed is an ‘open’ approach to classify all deaths in the region. Reference Chandramohan, Maude, Rodrigues and Hayes15 The data are computerised and reviewed every month by the whole health and development team. Independent interviewers have validated the procedure to assess the accuracy of the surveillance data.
Recruitment of participants
We recruited family members of all people who died by suicide during the study period (July 2006 to February 2008). The controls were pair-matched to the suicide cases by age (2 years), gender and neighbourhood (those living on the same street).
Assessment
The investigators established working relationships with the village leaders, local physicians and the community health workers. One investigator (S.D.M.) and the local community health worker visited the first-degree relatives of the dead person 2 months after the suicide. All interviews were conducted in the households of the participants. If the house was locked, we visited it on at least three occasions before excluding it. Each interview lasted about 2 h. A second interview was scheduled if the participant reported tiredness or difficulty in concentration. We interviewed more than one informant to minimise recall bias.
The psychological autopsy interview was a semi-structured schedule similar to earlier psychological autopsy studies. Reference Barraclough, Bunch, Nelson and Sainsbury16,Reference Foster, Gillespie and McClelland17 It was modified to suit the local cultural and social needs. The interview included the details of death, family history, childhood, adolescence, education, relationships, social support and isolation, housing, legal problems, employment, physical health, previous psychiatric history, exposure to suicidal behaviours, religious commitment, life events, contact with clinical services and relatives' response to death. We ascertained the psychiatric morbidity by means of the Structured Clinical Interview for DSM–III–R (SCID), Reference Williams, Gibbon, First, Spitzer, Davies and Borus18 and employed its algorithms for diagnosis. We also recorded the sociodemographic characteristics on a structured form. We defined ‘chronic pain’ as one or more pain symptoms lasting for more than 12 months and ‘ongoing stress’ as one or more stressful life events persisting for more than 12 months. All psychological autopsies were discussed with a consultant psychiatrist (P.T.). The first-degree relatives of control group participants (those residing with the participant) were interviewed using similar procedures and the same instruments. A pilot study was done to establish the feasibility of the method.
The instruments were translated into Tamil, the local language, and back-translated to English by bilingual health professionals. Consensus versions were employed for the study. The process of translation and back-translation employed standard procedures and focused on content, conceptual, semantic and technical equivalence.
Ethical considerations
The institutional review board of the Christian Medical College, Vellore, approved the study. We explained the details of the study to all participants and ensured that they provided written informed consent. We provided supportive counselling and appropriate referral services for the relatives where necessary.
Statistical analysis
We initially analysed the sociodemographic data, psychosocial profiles and psychiatric morbidity using descriptive statistics. We converted the continuous variables to categorical measures by splitting them into two categories using their median values. Reference Ragin19 The dependent variable was suicide or control status and the independent variables were the hypothetical psychosocial and psychiatric risk factors. We calculated the odds ratios with 95% confidence intervals for various risk factors. We employed Fisher's exact test to assess the statistical significance in situations where the variable was absent from either the case or the control group, as odds ratios could not be calculated. We performed multivariate analysis using backward conditional logistic regression with determinants that were significant on bivariate analysis. We analysed our data using the statistical software package SPSS version 16.0 for Windows.
Available systematic review of psychological autopsy studies of suicide has established the proportion of psychiatric morbidity among the control group as 27%. Reference Cavanagh, Carson, Sharpe and Lawrie6 We estimated the required sample size with an anticipated odds ratio of 2.5, 80% power and 5% alpha error as 82 matched case–control pairs for a two-sided test. A large population-based study has reported that half of the control group experienced more than one life event. Reference Phillips, Yang, Zhang, Wang, Ji and Zhou12 We again estimated the required sample size with an anticipated odds ratio of 2.5, 80% power and 5% alpha error as 81 matched case–control pairs for a two-sided test. Hence, we decided to include 100 suicide cases and 100 matched controls in our study.
Results
Sociodemographic characteristics
Figure 1 documents the details of recruitment of informants. Among the 122 suicides (73 male, 49 female; male to female ratio 1:0.67) occurring during the study period, we were able to trace the first-degree relatives in 100 cases (82%). All invited informants regarding the people who had died and the neighbourhood controls consented to participate. Table 1 records the sociodemographic and psychiatric profiles of the case and control groups. The majority were married, literate, from the lower socioeconomic class and owned their homes. The male to female ratio for suicide was 1:0.69.
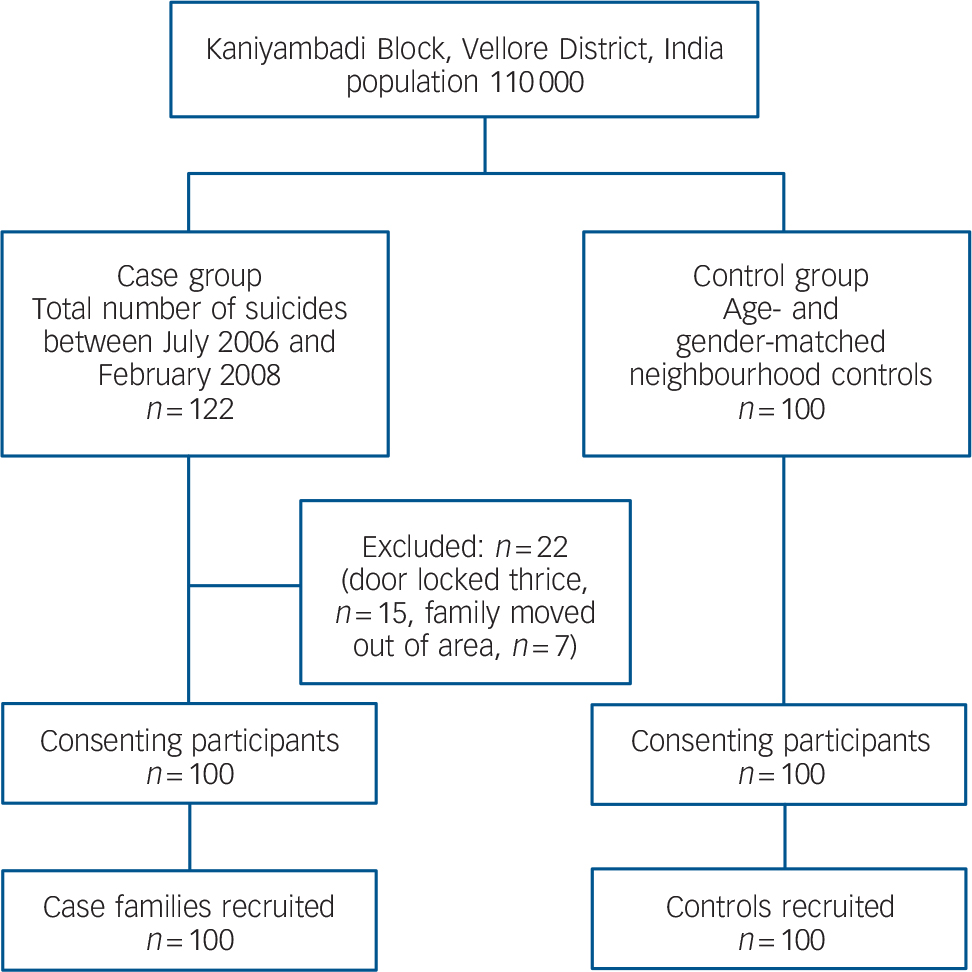
Fig. 1 Study profile.
Table 1 Sociodemographic and psychiatric profiles of the suicide group and matched living controls
| Case group n = 100 | Control group n = 100 | |
|---|---|---|
| Gender, n (%) | ||
| Male | 59 (59) | 59 (59) |
| Female | 41 (41) | 41 (41) |
| Marital status, n (%) | ||
| Single | 27 (27) | 25 (25) |
| Married | 55 (55) | 68 (68) |
| Widowed/separated | 18 (18) | 7 (7) |
| Most recent occupation, n (%) | ||
| Unemployed | 4 (4) | 5 (5) |
| Labourer | 52 (52) | 58 (58) |
| Skilled | 6 (6) | 4 (4) |
| Professional | 1 (1) | 0 (0) |
| Homemaker | 27 (27) | 25 (25) |
| Student | 10 (10) | 8 (8) |
| Accommodation, n (%) | ||
| Own | 90 (90) | 94 (94) |
| Rented | 10 (10) | 6 (6) |
| Living alone | 13 (13) | 0 (0) |
| Psychiatric morbidity, n (%)a | ||
| Present | 37 (37) | 16 (16) |
| Absent | 63 (63) | 84 (84) |
| DSM—III—R diagnostic categories, n (%) | ||
| Adjustment disorder | 15 (15) | 5 (5) |
| Alcohol dependence syndrome | 16 (16) | 7 (7) |
| Dysthymia | 2 (2) | 4 (4) |
| Major depressive disorder | 2 (2) | 0 (0) |
| Paranoid schizophrenia | 2 (2) | 0 (0) |
| Age, years: mean (s.d.) | 42.24 (20.69) | 42.65 (20.76) |
| Years of education: mean (s.d.) | 5.37 (4.14) | 4.57 (3.99) |
| Monthly income of family, INR: mean (s.d.) | 3966 (3795) | 3325 (2305) |
Psychiatric morbidity and psychosocial stress
More than a third (37%, 95% CI 27.5–46.5) of the suicide group and 16% (95% CI 8.8–23.2) of the control group had at least one Axis I psychiatric diagnosis. Among the suicide group, alcohol dependence syndrome was the most common diagnosis (16%, 95% CI 8.8–23.2), followed by adjustment disorders (15%, 95% CI 8.0–22.0). Prevalence rates for dysthymia, major depressive episode and schizophrenia were 2% each (95% CI 0–4.7).
Risk factors for suicide
The results of the bivariate analysis of psychosocial and psychiatric risk factors for suicide are shown in Table 2. The exposure variables such as living alone (Fisher's exact test, P<0.001) and break in a steady relationship within the past year (Fisher's exact test, P<0.001) were significantly associated with suicide and were not present in the control group. Twice as many people in the case group had ongoing stress and lacked confidants compared with the control group, and a significantly higher number of the case group were widowed or separated and had chronic pain. Psychiatric morbidity was also higher among this group. Variables significantly associated with suicide on bivariate analysis and which were present among both cases and controls were included in the multivariate analysis. We built two models using backward conditional logistic regression. Model 1 included variables that were significant on bivariate analysis and all psychiatric morbidity as a single exposure variable. Model 2 included all variables significant on bivariate analysis, and adjustment disorders and other psychiatric morbidity as two separate exposure variables. Ongoing stress and chronic pain were the only two significant variables in both models (Table 3).
Table 2 Bivariate analysis: risk factors associated with suicide among the case group (n = 100) and the control group (n = 100)
| Characteristic | Cases n (%) | Controls n (%) | Odds ratio (95% CI) | P |
|---|---|---|---|---|
| Male gender | 59 (59) | 59 (59) | 1.0 (0.6-1.8) | 1.00 |
| Widowhood or separated | 18 (18) | 7 (7) | 2.9 (1.1-7.7) | <0.05* |
| Illiteracy | 23 (23) | 29 (29) | 0.7 (0.4-1.4) | 0.33 |
| Monthly family income <INR2400 | 52 (52) | 51 (51) | 1.0 (0.6-1.8) | 0.89 |
| Living alone | 13 (13) | 0 (0) | <0.001a*** | |
| Lack of confidants | 44 (44) | 18 (18) | 3.6 (1.9-6.8) | <0.01** |
| Lack of religious faith | 27 (27) | 14 (14) | 2.3 (1.1-4.7) | <0.05* |
| Ongoing stress | 63 (63) | 24 (24) | 5.4 (2.9-10.0) | <0.01** |
| Bereavement | 24 (24) | 28 (28) | 0.8 (0.4-1.5) | 0.52 |
| Break in steady relationship | 34 (34) | 0 (0) | 0.001a*** | |
| Unemployment | 2 (2) | 0 (0) | 0.49a | |
| Recent major financial crisis | 11 (11) | 5 (5) | 2.4 (0.8-7.0) | 0.13 |
| Chronic pain | 15 (15) | 1 (1) | 17.5 (2.3-135.0) | <0.01** |
| Family history of suicide | 9 (9) | 10 (10) | 0.9 (0.4-2.3) | 0.81 |
| Previous suicidal attempts | 13 (13) | 8 (8) | 1.7 (0.7-4.4) | 0.25 |
| Family history of psychiatric illness | 8 (8) | 6 (6) | 1.4 (0.5-4.1) | 0.58 |
| Any psychiatric diagnosis | 37 (37) | 16 (16) | 3.1 (1.6-6.3) | <0.05* |
| Adjustment disorder | 15 (15) | 5 (5) | 3.4 (1.2-9.6) | <0.05* |
| Major depressive disorder | 2 (2) | 0 (0) | 0.49a | |
| Alcohol dependence | 16 (16) | 7 (7) | 2.8 (1.0-6.9) | <0.05* |
| Psychiatric diagnoses without adjustment disorders | 22 (22) | 11(11) | 2.3 (1.0-5.0) | <0.05* |
Table 3 Multivariate analysis: risk factors associated with suicide among cases (n = 100) and controls (n = 100)
| Multivariate analysisa OR (95% CI) | |
|---|---|
| Model 1b | |
| Ongoing stress | 98.2 (27.9-345.8) |
| Chronic pain | 40.0 (3.0-537.8) |
| Any psychiatric diagnosis | 2.8 (0.95-8.2) |
| Model 2c | |
| Ongoing stress | 97.7 (27.8-343.2) |
| Chronic pain | 66.1 (5.0-873.5) |
Discussion
Our findings suggest that psychosocial stress has a major role in suicide in a rural south Indian community. Psychiatric morbidity was not significantly related to suicide on multivariate analysis. Although the association with psychosocial stress has been reported previously from India, Reference Prasad, Abraham, Minz, Abraham, Joseph and Muliyil2,Reference Gururaj, Isaac, Subbakrishna and Ranjani7,Reference Cheng, Chen, Chen and Jenkins10,Reference Vijayakumar and Rajkumar13 this is the first study to use a community surveillance programme and structured psychological autopsies. The study also validated the verbal autopsy procedure. We believe that the high rates of suicide reported from Vellore (95 per 100 000) reflect accurate reporting due to the ongoing surveillance of the comprehensive community health programme. The official rate of suicide in India is about 10 per 100 000. 22 Inefficient civil registration systems, poor reporting of deaths, variable standards in certifying death and the legal as well as social consequences of suicide explain the low rates. Reference Joseph, Abraham, Muliyil, George, Prasad and Minz1–Reference Abraham, Abraham and Jacob4 Much higher rates of 62 per 100 000 have been reported from other parts of the state where verbal autopsies have been systematically employed as part of a research project. Reference Gajalakshmi and Peto23 The higher rates from Vellore, we believe, are due to the fact that the programme has been functioning in the area for over 50 years, and the health workers are residents of the villages, giving them access to local information usually not available to outsiders.
Other studies that have moved beyond the symptom checklist approach to diagnosing depression and have examined the context have also established that at least half of the depressive disorders in people who die by suicide are secondary to physical disease and psychosocial stress. Reference Zonda24 Studies diagnosing depressive disorders without structured diagnostic interviews often employ lower thresholds, and such assessments sacrifice specificity and may yield inflated estimates of psychiatric diagnoses because of high false-positive rates.
Strengths and limitations
The strengths of this study are the inclusion of suicides from a community programme with effective surveillance, a very good response rate, the use of structured diagnostic interviews, adequate sample size and the use of a standard protocol for psychological autopsies. Its limitations were the possibility of recall bias and the absence of masking of case status during the interviews. Although the use of SCID in informants may be problematic, it was employed in order to provide a structured interview for diagnosis, and has been used in similar studies. Reference Foster, Gillespie and McClelland17,Reference Schneider, Wetterling, Sargk, Schneider, Schnabel and Maurer20,Reference Chen, Chan, Wong, Chan, Chan and Law21 The SCID for DSM–III–R was used because of the availability of a Tamil version, the familiarity of the investigators with the interview schedule and the absence of major differences from DSM–IV. Although the likelihood of underreporting of mental illness was present, the use of a structured interview and diagnostic algorithms for DSM–III–R minimised recall and interviewer bias respectively. We also attempted to minimise the recall bias by interviewing more than one informant and collaborating with local community health workers. Although we did not formally validate the instruments, we believe that they have face, content and construct validity and that the study adds to existing knowledge. However, it would be prudent to exercise caution in generalising the finding of our study to other parts of the country and to other populations.
Comparing Indian and Western data
The suicide rates in the Western world are low compared with the rates reported from low- and middle-income countries. Reference Joseph, Abraham, Muliyil, George, Prasad and Minz1–Reference Abraham, Abraham and Jacob4,Reference Gajalakshmi and Peto23,25 Western data also argue for a high prevalence of mental illness in those who complete suicide. Reference Hawton and Heeringen26 The Indian experience suggests that many suicides are impulsive and related to stress. Recent studies using verbal autopsy data have shown that suicide is often related to socioeconomic circumstances and to interpersonal, social and cultural conflicts. Reference Prasad, Abraham, Minz, Abraham, Joseph and Muliyil2 Other studies using psychological autopsies have supported the conclusion that suicide is related to interpersonal conflicts, marital discord, alcoholism, financial problems and unemployment. Reference Gururaj, Isaac, Subbakrishna and Ranjani7 Suicide has also been associated with adverse economic circumstances among farmers in India. Reference Sainath27 A previous case–control study on risk factors for suicide in India, although documenting the association between suicide and psychopathology, highlighted its association with adverse life events. Reference Vijayakumar and Rajkumar13 Qualitative data suggest that many in the general population view suicide as an option when faced with apparently insoluble personal difficulties and misfortune. Reference Manoranjitham, Charles, Saravanan, Jayakaran, Abraham and Jacob9 Studies from China too have reported low rates of mental illness among those who kill themselves and highlighted the role of interpersonal conflict and impulsive suicide. Reference Yang, Phillips, Zhou, Wang, Zhang and Xu28
Although people with mental illness do die by suicide in India, the contribution of such suicides to the high rate is small when compared with the number of suicides secondary to stress and conflict. The relationship between stress, impulsivity and suicide is widely acknowledged by mental health professionals in low- and middle-income countries. Although one can relabel distress secondary to life events and social circumstances as depression using the medical model, it does not reflect severe mental illness. Studies of risk factors for suicide that employed police records (to identify cases of suicide) tend to overestimate the risk of the relationship between mental illness and its contribution to suicide. Reference Gururaj, Isaac, Subbakrishna and Ranjani7,Reference Khan, Mahmud, Karim, Zaman and Prince11–Reference Vijayakumar and Rajkumar13 Police records, which form the basis of official statistics, grossly underestimate the actual rate of suicide in populations. Reference Joseph, Abraham, Muliyil, George, Prasad and Minz1–Reference Abraham, Abraham and Jacob4 This is particularly true among those without a history of severe mental illness. Social stigma, local beliefs and legal consequences result in many suicides being declared natural or accidental deaths. In addition, the absence of systematic sampling of police data in societies with high social stigma will oversample people with severe mental illness, suggests selection bias and probably invalidates the results. Reference Khan, Mahmud, Karim, Zaman and Prince11
The differences between Indian and Western data are probably a reflection of the many differences in the populations (such as the social security net, the national health service systems, rapidity of social and economic change, growth and development) and cultures. Severe mental illness seems to be related to suicide when the rates are low (i.e. 10 per 100 000 population) but does not seem to contribute significantly when the suicide rates are high, as in India, where social, economic and cultural factors play a much greater part. Similar findings are reported from the Baltic states, which have high rates of suicide attributed to social and economic transitions. Reference Varnik, Kolves and Wasserman29
Disease or distress?
Separating human distress from depression is difficult. Reference Heath30 The depression seen in the community is often viewed as a result of personal and social stress, lifestyle choices or habitual maladaptive patterns of behaviour. Consequently, the general population and general physicians often hold psychological and social models for depression and for suicide. Psychiatrists, with their biomedical frameworks, on the other hand, argue for disease models for these conditions. Reference Kessler, Lloyd, Lewis and Gray31 They transfer the disease halo reserved for melancholia and severe mental illness to all psychiatric diagnoses. Epidemiological studies in general and on suicide in particular use diagnostic instruments that do not evaluate stress-related conditions, Reference Lewis, Pelosi, Araya and Dunn32,Reference Robins, Wing, Wittchens, Helzer, Babor and Burke33 and fail to address adjustment disorders. Reference Portzky, Audenaert and van Heeringen34,Reference Casey, Dowrick and Wilkinson35 Our study supports the view that the majority of people in India who kill themselves do not have a severe mental disorder. Qualitative investigations from the region have documented a widespread belief in the population that suicide is an option when faced with severe personal distress. Reference Manoranjitham, Charles, Saravanan, Jayakaran, Abraham and Jacob9
The use of symptom counts for the diagnosis of depression, the focus on cross-sectional presentations and the refusal to factor the context (coping, stress, supports) are limitations of the current diagnostic criteria for depression. Reference Jacob36 The diagnosis of major depression straddles all three traditional typologies of melancholia (usually not associated with stress, and often in people with family history of bipolar disorder or melancholia), dysthymia (depression in people with poor coping strategies associated with chronic and fluctuating stress) and adjustment disorders (depression in people good at coping but currently facing acute and severe stress). The high rates of spontaneous remission and of placebo response seen in major depression argue for heterogeneity and against its disease status. The subordinate status of dysthymia and adjustment disorders to major depressive disorder, and the mechanistic application of the diagnostic hierarchy, allow major depression and the medical model to argue for disease in all people with depressive symptoms rather than recognising human distress. Reference Jacob36 Medical assessments and interventions mandate the use of medical labels.
Suicide prevention
Suicide prevention in India and other low- and middle-income countries requires public health interventions. Reference Jacob5 Although curative psychiatric services and counselling for individuals will relieve distress and prevent suicide, they will not reduce population suicide rates. There is a need to reduce the medicalisation of personal and social distress and focus on other underlying causes of human suffering, including poverty, economic inequality and lack of social justice. Reference Jacob5 Macroeconomic policies that protect vulnerable sections of the population from the sudden opening up of markets, the provision of basic needs (water, sanitation, housing, nutrition, education, health, employment), an essential pesticide list that bans the manufacture and sale of pesticides lethal to humans, and legislation to prevent gender and other discrimination are suggested as solutions. Broad population-based strategies cutting across narrow disciplinary perspectives will be needed to reduce population suicide rates.
Funding
The study was funded by a grant from the Christian Medical College, Vellore.
Acknowledgements
The authors thank the participating families and the health workers for their cooperation.







eLetters
No eLetters have been published for this article.