Bipolar disorder is a complex mood disorder that can be viewed as a spectrum condition. Reference Angst1,Reference Goodwin and Geddes2 A growing body of research suggests that it is underrecognised in clinical practice and often misdiagnosed as recurrent major depressive disorder. Reference Ghaemi, Ko and Goodwin3–Reference Smith and Ghaemi8 Estimates of the mean delay between first onset of mood symptoms and receiving a correct bipolar diagnosis are in the region of 10 years. Reference Lish, Dime-Meenan, Whybrow, Price and Hirschfeld9–Reference Berk, Dodd, Callaly, Berk, Fitzgerald and de Castella11 Certain subgroups of individuals with depression, such as those with early-onset depression Reference Geller, Zimerman, Williams, Bolhofner and Craney12,Reference Smith, Harrison, Muir and Blackwood13 and those with severe or treatment-refractory depression, Reference Sharma, Khan and Smith14 appear to have the highest rates of unrecognised bipolar disorder. However, many of the studies that have identified underdiagnosis of bipolar disorder have been carried out in secondary or tertiary care settings and there have as yet been no studies in the UK assessing the likely prevalence of unrecognised bipolar disorder in primary care patients who have a working diagnosis of unipolar depression.
This study had three main aims. First, to estimate the proportion of primary care patients with a working diagnosis of unipolar depression who satisfy DSM–IV 15 diagnostic criteria for bipolar disorder (either bipolar I disorder, bipolar II disorder or bipolar disorder not otherwise specified). Second, to test the potential usefulness of two screening instruments for bipolar disorder – the Hypomania Checklist (HCL–32) Reference Angst, Adolfsson, Benazzi, Gamma, Hantouche and Meyer16 and Bipolar Spectrum Diagnostic Scale (BSDS) Reference Ghaemi, Miller, Berv, Klugman, Rosenquist and Pies17 – within a primary care sample. Third, to assess whether those participants with major depressive disorder who screen false positive for bipolar disorder on the HCL–32 or BSDS questionnaires (that is, participants with major depressive disorder and with a history of subdiagnostic manic symptoms) differ from participants with major depressive disorder but with no or only minimal history of manic symptoms in terms of their clinical course, psychosocial functioning and quality of life.
Method
Recruitment
This study was approved by the South East Wales Research Ethics Committee, Cardiff and Vale University Health Board, and Cardiff, Merthyr Tydfil and Newport Local Health Boards (primary care local health boards). Our aim was to collect detailed diagnostic, clinical, psychosocial functioning and quality of life data on a representative sample of individuals from primary care who had a current working diagnosis of unipolar depression. In order to sample people from a range of socioeconomic backgrounds, we invited 45 general practices in three local health boards in South Wales to take part in this study (27 practices from Cardiff Local Health Board, 9 from Merthyr Tydfil Local Health Board and 9 from Newport Local Health Board). Eleven practices agreed to take part (seven from Cardiff, three from Merthyr and one from Newport). From their patient databases, practice managers generated lists of individuals who had at least one of eight possible codes for depression recorded by their general practitioner (GP) within the past 5 years. These codes were: ‘recurrent depressive disorder’; ‘depressive episode’; ‘depressive disorder NEC (not elsewhere specified)’; ‘recurrent major depressive episode’; ‘single major depressive episode’; ‘neurotic (reactive) depression’; ‘depressed’; and ‘depression NOS (not otherwise specified)’.
When large numbers of potentially eligible participants were identified within a single practice, a maximum of 400 were selected using computer-generated random number lists. In total, 3117 patients were identified as potentially eligible from the 11 practices and all were invited to take part in this study. The invitation sheet about the study was sent to individuals by practice managers on behalf of the research team and included the HCL–32 and BSDS questionnaires. Invited participants were asked to return the completed questionnaires if they were interested in taking part in the study. A reminder invitation pack was sent by practice managers to those who had not replied after 8 weeks.
The recruitment process is outlined inFig. 1. In total, 576 individuals (18.5% of those invited) volunteered to take part and returned completed HCL–32 and BSDS questionnaires. In order to compare volunteers and non-volunteers, each practice manager used computer-generated random number lists to select a small sample of 55 volunteers and 55 non-volunteers (5 volunteers and 5 non-volunteers from each practice) and performed a case-file review of age, gender, time since first diagnosis of depression, whether currently taking antidepressant medication, whether taking other medication, and whether diagnosed with a comorbid medical disorder (Table 1).
The 576 participants who returned HCL–32 and BSDS questionnaires were divided into two groups: a group of ‘high scorers’ (defined as scoring either 14 or more on the HCL–32 or 13 or more on the BSDS; n = 411) and a group of ‘low scorers’ (defined as scoring less than 14 on the HCL–32 and less than 13 on the BSDS; n = 165) (Fig. 1). This approach is outlined in the recruitment flow chart (Fig. 1). The choice of these thresholds was informed by several previous studies that suggested that 14 or more on the HCL–32 and 13 or more on the BSDS represented reasonable cut-offs on each questionnaire for reliably distinguishing between bipolar disorder and major depressive disorder. Reference Angst, Adolfsson, Benazzi, Gamma, Hantouche and Meyer16–Reference Vieta, Sanchez-Moreno, Bulbena, Chamorro, Ramos and Artal20
From the 576 volunteers, all of the ‘low scorers’ group (n = 165) and 50% of the ‘high scorers’ group (selected using computer-generated random number lists; n = 205) were invited to take part in a comprehensive diagnostic and clinical assessment. In total, 154 (41.6%) of these 370 eligible participants were assessed at interview. To test the representativeness of this sample, the 154 participants who were interviewed were compared with the 216 participants who declined to be interviewed (Table 2).
Table 1 Characteristics of a random subsample of volunteers v. non-volunteers

| Volunteers (n = 55) | Non-volunteers (n = 55) | P | |
|---|---|---|---|
| Age, years: mean (s.d.) | 42.8 (13.0) | 44.4 (11.1) | 0.49a |
| Gender ratio, male:female | 17:38 | 18:37 | 0.84b |
| Time since first diagnosis, months: median (range) | 60 (4–492) | 48 (3–540) | 0.51c |
| Currently taking antidepressants, n (%) | 32 (58.2) | 18 (32.7) | 0.01b |
| Currently taking other medications, n (%) | 35 (63.6) | 27 (49.1) | 0.12b |
| At least 1 comorbid medical disorder, n (%) | 28 (50.9) | 22 (40.0) | 0.29b |
a Independent t-test.
b χ2-test.
c Mann-Whitney U-test.
Table 2 Comparison of interviewees v. those who were not interviewed

| Interviewed (n = 154) | Not interviewed (n = 216) | P | |
|---|---|---|---|
| Age, years: mean (s.d.) | 44.0 (12.5) | 40.9 (13.7) | 0.03a |
| Male, n (%) | 53 (34.4) | 58 (26.9) | 0.12b |
| Ethnicity, White: n (%) | 118 (76.6) | 155 (71.8) | 0.17b |
| Hypomania Checklist-32 score, mean (s.d.) | 12.83 (7.14) | 14.09 (7.46) | 0.10a |
| Bipolar Spectrum Diagnostic Scale score, mean (s.d.) | 11.77 (6.14) | 12.66 (6.45) | 0.19a |
a Independent t-test.
b χ2-test.

Fig. 1 Recruitment flow chart.
‘High scorers’ were defined as having either a score of 14 or more on the Hypomania Checklist–32 (HCL–32) or 13 or more on the Bipolar Spectrum Diagnostic Scale (BSDS). ‘Low scorers’ were defined as having a score of less than 14 on the HCL–32 and less than 13 on the BSDS. NOS, not otherwise specified.
Assessments
The comprehensive diagnostic and clinical assessment was carried out by a research psychologist and included: the Mini International Neuropsychiatric Interview (MINI) to obtain DSM–IV diagnoses; Reference Sheehan, Lecrubier, Harnett-Sheehan, Amorim, Janavas and Weiller21 a structured assessment of socio-demographics, medical history, current medication and family history of psychiatric disorder; the Montgomery–Åsberg Depression Rating Scale (MADRS) Reference Snaith, Harrop, Newby and Teale22 and the Young Mania Rating Scale (YMRS) Reference Young, Biggs, Ziegler and Meyer23 to assess levels of current depressive and manic symptoms respectively; the Massachusetts General Hospital (MGH) assessment of treatment resistance to antidepressants; Reference Fava24 the Global Assessment of Functioning (GAF) scale; Reference Spitzer, Gibbon, Williams, Sederer and Dickey25 the Functional Assessment Screening Tool (FAST); Reference Rosa, Sanchez-Moreno, Martinez-Aran, Salamero, Torrent and Reinares26 and the World Health Organization Quality of Life Instrument (WHOQOL–Bref). 27
Two-phase sampling analysis
The prevalence of undiagnosed bipolar disorder observed in the data was estimated using Dunn’s two-phase sampling strategy (Fig.1). Reference Dunn, Pickles, Tansella and Vazque-Barquero28 This approach applies to survey designs where the population of interest is screened and then split into multiple arms based on screening scores. Differential proportions are invited to further testing/interview to ensure broadly equal numbers of participants in each arm. Point estimates of the prevalence along with 95% confidence intervals were calculated using weighted logistic regression.
Three increasingly conservative sets of assumptions were made about participants who did not respond either to the initial questionnaire invitation or subsequently to the invitation to interview in order to provide robust estimates of the proportion of undiagnosed bipolar in this population. First, least conservatively, we made the assumption that all of those who were not interviewed and all of those who did not return their questionnaires would have responded similarly to those who were interviewed (Fig. 1). Here we assume that the 92 high scorers who were interviewed represent all of the 411 high scorers (a sampling weight of 4.4) and that the 62 low scorers who were interviewed represent all 165 low scorers (a sampling weight of 2.7). This provides the least conservative estimate of the prevalence of undiagnosed bipolar disorder in this sample. Second, more conservatively, we assumed that all of those who were not interviewed did not have bipolar disorder and that the 576 participants who returned their questionnaires were representative of the 3117 individuals with unipolar depression initially approached. This means that the 205 high scorers who were invited to interview (comprising 113 high-scoring participants not interviewed who are assumed not to have bipolar disorder and 92 who were interviewed) represent the 411 high scorers. This calculation, with a weighting of 2 for the 205 high scorers and 1 for the 165 low scorers, gives an intermediate estimate of undiagnosed bipolar disorder. Finally, the most conservative estimate makes the assumption that all of those who dropped out at either stage (either through failing to return the initial screening questionnaire or not having been interviewed when invited) did not have bipolar disorder. The 205 high scorers invited to interview represent the 411 high scorers and the 165 low scorers represent everyone else (the weighting for the 205 high scorers is 2.0 and the weights for the 165 low scorers is 16.4).
Receiver Operating Characteristic curve analyses
To assess the potential usefulness of the HCL–32 and BSDS questionnaires in this sample, we conducted receiver operating characteristic (ROC) curve analyses between participants with DSM–IV-defined bipolar disorder and major depressive disorder. Optimal thresholds were based on maximising the sum of the sensitivity and specificity.
Comparing participants with major depressive disorder with and without a history of manic symptoms
To assess whether participants with major depressive disorder with a history of subdiagnostic manic symptoms differed from those participants with no or minimal history of manic symptoms, we divided participants with major depressive disorder into two groups: one group of ‘false positives’ who scored above the optimal calculated threshold for bipolar disorder on either the HCL–32 or the BSDS (the major depressive disorder (MDD)–manic symptoms group) and another group who were ‘true negatives’ in that they scored below the threshold for bipolar disorder on both screening instruments (called the MDD group). For each questionnaire, these groups were then compared with each other on a range of demographic, clinical, psychosocial functioning and quality of life measures. We used SPSS for Windows, version 11.5), to conduct chi-squared tests for dichotomous variables, the Mann–Whitney U-test for non-parametric data and independent t-tests for parametric data. Given the relatively large number of comparisons between groups, statistical significance was set at 0.01.
Results
Sample representativeness
Volunteers for the study who returned their questionnaires and those who did not return their questionnaires were generally well matched apart from whether they were currently taking antidepressants (58.2% of volunteers v. 32.7% of non-volunteers;Table 1). There were no differences between participants who were and were not subsequently interviewed in terms of gender ratio, ethnicity and mean HCL–32 and BSDS scores, although the interviewed group were younger (mean age 44.0 years v. 40.9 years, P = 0.03) (Table 2).
Estimates of previously unrecognised bipolar disorder
From the 154 participants interviewed, 9 (5.8%) had not previously experienced an episode of major depression as defined by DSM–IV. In total, 116 (75.3%) had a history of DSM–IV major depressive disorder and 29 (18.8%) satisfied DSM–IV criteria for bipolar disorder (including bipolar I disorder, n = 2; bipolar II disorder, n = 15; and bipolar disorder not otherwise specified, n = 12) (Fig. 1).
Following the two-phase sampling methodology proposed by Dunn et al, Reference Dunn, Pickles, Tansella and Vazque-Barquero28 three increasingly conservative estimates of previously unrecognised bipolar disorder in this sample were possible. The least conservative estimate, which makes the assumption that all of those who were not interviewed and all of those who did not return their questionnaires would have responded similarly to those who were interviewed, is 21.6% (95% CI 18.4–25.1). A more conservative estimate assumes that all of those who were not interviewed did not have bipolar disorder and that the 576 participants who returned their questionnaires were representative of the 3117 individuals with unipolar depression initially approached, and gives an estimate of previously undiagnosed bipolar disorder of 9.6% (95% CI 7.4–12.3). Finally, the most conservative estimate makes the assumption that all of those who dropped out at either stage (either through failing to return the initial screening questionnaire or not having been interviewed when invited) did not have bipolar disorder. This gives an estimate of 3.3% (95% CI 2.7–3.9).
HCL–32 and BSDS screening questionnaires in primary care
In this sample, both the HCL–32 and BSDS could distinguish between bipolar disorder and major depressive disorder with reasonable precision (the area under the curve was 0.81 for the HCL–32 and 0.71 for the BSDS) (Figs2 and3). However, even though the optimum thresholds of 18 or more for the HCL–32
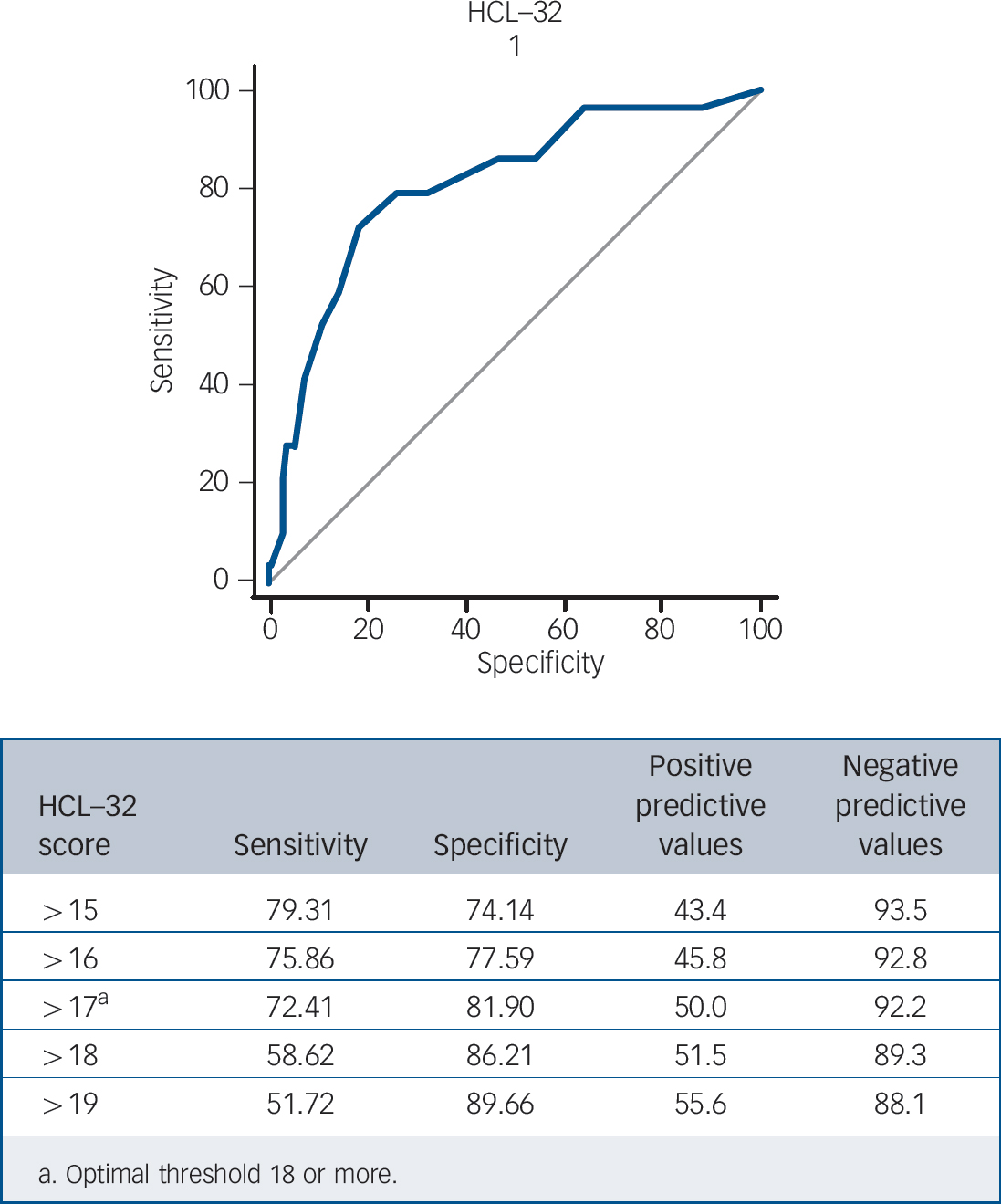
Fig. 2 Receiver operating characteristic curve analysis for the Hypomania Checklist–32 (HCL–32): bipolar disorder (n=29) v. major depressive disorder (n=116).
and 12 or more for the BSDS had reasonable sensitivities and specificities, the positive predictive values for both questionnaires were quite low (50.0% for the HCL–32 and 32.1% for the BSDS).
Subthreshold manic symptoms in major depressive disorder
The sample of 116 participants with major depressive disorder were divided into two groups according to their scores on each of the questionnaires: a MDD–manic symptoms group (n = 60) and an MDD group (n = 56). These groups were compared with each other on a range of clinical, psychosocial functioning and quality of life measures (Table 3; see online Table DS1 for a more detailed version of this table.). For both the HCL–32 threshold definition of major depressive disorder with manic symptoms (a score of 18 or more) and the BSDS definition (a score of 12 or more) there were no significant differences between the two groups on several demographic (gender, ethnicity, employment status, premorbid IQ assessed with the National Adult Reading Test) Reference Nelson and Willison29 and clinical variables (whether ever admitted to hospital for depression, antidepressant treatment resistance, whether currently taking psychotropic medication and family history of depression and bipolar disorder) (Table 3). However, for the HCL–32 definition, the MDD–manic symptoms group were significantly younger, had an earlier age at onset of depression, reported more current depressive symptoms, had more frequent episodes of depression and were more likely to have a comorbid history of alcohol misuse and alcohol dependence. This group also had significantly poorer functioning rated by the GAF, more difficulties with relationships according to the FAST questionnaire and lower scores on the overall score for the WHOQOL–Bref

Fig. 3 Receiver operating characteristic curve analysis for the Bipolar Spectrum Diagnostic Scale (BSDS): bipolar disorder (n=29) v. major depressive disorder (n=116).
quality of life measure (including lower scores within the ‘psychological’ and ‘environment’ subsections).
Similarly, the MDD–manic symptoms group defined by the BSDS threshold were significantly younger, had more current depressive symptoms, were more likely to have a history of chronic depression, had more lifetime comorbid panic, alcohol misuse and alcohol dependence disorders and had worse current functioning measured by the GAF. They were significantly more impaired in all of the FAST psychosocial functioning sections (including ‘autonomy’, ‘occupational’, ‘cognitive’, ‘finances’, ‘relationships’ and ‘leisure time’) and all of the WHOQOl–Bref quality of life sections (‘physical health’, ‘psychological’, social relationships’ and ‘environment’) (Table 3 and online Table DS1).
Overall, these findings suggest that the MDD–manic symptoms group (whether defined by the HCL–32 or the BSDS) had a pattern of depressive illness that was more severe and that was associated with both poorer psychosocial functioning and worse quality of life than participants with major depressive disorder with no or little history of subthreshold manic symptoms.
Discussion
There are three key findings from this study. First, unrecognised DSM–IV bipolar disorder may be relatively common in primary care patients with a working diagnosis of unipolar depression. Our most conservative estimate was 3.3% and our least conservative estimate was 21.6%. Second, the HCL–32 and BSDS screening questionnaires (when used in primary care settings) may have limited utility in terms of detecting DSM–IV-defined bipolar
Table 3 Demographic, clinical, psychosocial functioning and quality of life characteristics according to threshold score on the Hypomania Checklist-32 and Bipolar Spectrum Diagnostic Scale: major depressive disorder with manic symptoms group (MDD-manic symptoms group) v. MDD group (see online Table DS1 for a more detailed version of this table)

| Hypomania Checklist-32 | Bipolar Spectrum Diagnostic Scale | |||||
|---|---|---|---|---|---|---|
| MDD-manic symptoms group (score 18 or more) (n = 42) | MDD group (score 17 or less) (n = 103) | P | MDD-manic symptoms group (score 12 or more) (n =78) | MDD group (score 11 or less) (n = 67) | P | |
| Age, years: mean (s.d.) | 38.7 (9.5) | 46.7 (12.8) | 0.0004a | 41.7 (11.4) | 47.6 (12.9) | 0.004a |
| Male, n (%) | 19 (45) | 27 (26) | 0.03b | 29 (37) | 17 (25) | 0.13b |
| Ethnicity, White: n (%) | 41 (98) | 100 (97) | 0.86b | 76 (97) | 65 (97) | 0.88b |
| Currently employed, n (%) | 19 (45) | 41 (40) | 0.55b | 32 (41) | 28 (42) | 0.93b |
| Premorbid IQ (NART), median (range) | 35 (4–54) | 31 (4–49) | 0.14c | 32 (4–54) | 34 (4–48) | 0.58c |
| Age at onset of depression, years: mean (s.d.) | 20.6 (8.1) | 26.6 (14.2) | 0.01a | 22.7 (12.0) | 27.3 (13.7) | 0.03a |
| MADRS, median (range) | 17.5 (0–35) | 10.0 (0-49) | 0.01c | 17 (0–40) | 7 (0–49) | 0.00004c |
| YMRS, median (range) | 0 (0–5) | 0 (0–5) | 0.04c | 0 (0–5) | 0 (0–5) | 0.03c |
| Chronic depression, n (%) | 20 (48) | 58 (56) | 0.34b | 34 (44) | 44 (66) | 0.008b |
| Episodes of depression,d median (range) | 6 (3–40) | 3 (1–30) | 0.003c | 6 (1–40) | 3 (1–30) | 0.02c |
| Ever admitted, n (%) | 4 (10) | 12 (12) | 0.71b | 8 (10) | 8 (12) | 0.75b |
| MGH score, median (range) | 1.5 (0–8) | 1.5 (0–8) | 0.97c | 1.5 (0–10) | 1.5 (0–6) | 0.13c |
| On psychotropic medication, n (%) | 35 (83) | 79 (77) | 0.38b | 62 (80) | 52 (78) | 0.78b |
| First-degree relative with depression, n (%) | 23 (55) | 47 (46) | 0.32b | 40 (51) | 30 (45) | 0.44b |
| First-degree relative with bipolar disorder, n (%) | 4 (10) | 3(3) | 0.09b | 3 (4) | 4 (6) | 0.55b |
| Comorbid panic disorder, n (%) | 18 (31) | 25 (24) | 0.41b | 27 (35) | 11 (16) | 0.01b |
| Comorbid alcohol misuse, n (%) | 23 (55) | 18 (18) | 0.00001b | 29 (37) | 12 (18) | 0.01b |
| Comorbid alcohol dependence, n (%) | 17 (41) | 7(7) | 0.00001b | 19 (24) | 5 (8) | 0.006b |
| GAF score, mean (s.d.) | 63.4 (14) | 69.0 (12.4) | 0.001a | 64.1 (12.3) | 71.2 (13.1) | 0.001a |
| FAST: total score, median (range) | 31 (1–70) | 24 (0–62) | 0.02c | 31 (1–70) | 18 (0–57) | 0.0001c |
| WHOQOL-Bref, total score: median (range) | 45.5 (19–69) | 51 (29–73) | 0.007c | 47 (19–68) | 55 (29–73) | 0.00002c |
MDD, major depressive disorder; NART, National Adult Reading Test; MADRS, Montgomery–Asberg Depression Rating Scale; YMRS, Young Mania Rating Scale; MGH, Massachusetts General Hospital; GAF, Global Assessment of Functioning scale; FAST, Functional Assessment Screening Tool; WHOQOL-Bref, World Health Organization Quality of Life Instrument.
a Independent t-test.
b χ2-test.
c Mann-Whitney U-test.
d For episodes of depression: sample size n = 78.
disorder, although it is possible that they may be useful for broader definitions of bipolar disorder. Third, a history of manic symptoms in primary care patients with DSM–IV major depressive disorder is relatively common and is associated with a more morbid course of illness, worse psychosocial functioning and poorer quality of life.
Underdiagnosis of bipolar disorder in primary care
Our first finding, that unrecognised bipolar disorder could be diagnosed in at least 3.3% and at most 21.6% of our sample of primary care patients with unipolar depression, is in keeping with several studies that have found that bipolar disorder is often misdiagnosed as major depressive disorder. Reference Angst1,Reference Ghaemi, Ko and Goodwin3–Reference Chilakamarri, Filkowski and Ghaemi7,Reference Angst30 To our knowledge, our study is the first to investigate this issue in a sample of primary care patients within the UK. The three estimates of prevalence of previously undiagnosed bipolar disorder we obtained (21.6, 9.6 and 3.3%) were each based on different assumptions. The smallest proportion of 3.3% was based on the strictest assumption that all individuals who dropped out in this study did not have bipolar disorder. This seems unlikely and therefore provides an extreme lower bound for the proportion of people with undiagnosed bipolar disorder in this population. Even under the assumption that all of those who were invited to interview but not interviewed did not have bipolar disorder (and that the 576 responders were representative of the 3117 approached) the proportion of people with undiagnosed bipolar disorder was as high as 9.6%.
Although our findings will require replication, we suggest that at least 1 in 30 patients in primary care with a working diagnosis of unipolar depression may in fact have unrecognised bipolar disorder. Although challenging, this is potentially a finding with considerable implications for they way in which GPs approach the diagnosis and treatment of their patients with depression, Reference Smith, Thapar and Simpson31 especially when we consider how commonly antidepressants are prescribed in primary care and the potential for harm when antidepressants are used as monotherapy for bipolar disorder. Although there have as yet been no empirical studies of antidepressant therapy for subthreshold bipolar disorder, antidepressants are now known to be of only limited benefit in the treatment of DSM–IV bipolar depression Reference Sachs, Nierenberg, Calabrese, Marangell, Wisniewski and Gyulai32,Reference Smith, Forty, Russell, Caesar, Walters and Gordon-Smith33 and, at least for a proportion of individual’s with a DSM–IV bipolar diagnosis, they may be unhelpful by causing suicidal behaviour, treatment resistance and more frequent cycling of mood episodes. Reference El-Mallakh, Karippot, Ghaemi, El-Mallakh and Ghaemi34
Greater recognition of bipolar disorders in primary care will also have important resource implications for the way in which primary and secondary care services work together to manage individuals with depression.
Use of the HCL–32 and BSDS screening instruments in primary care
Although the HCL–32 and BSDS questionnaires had relatively low positive predictive values for detecting DSM–IV bipolar disorder (50.0% for the HCL–32 and 32.1% for the BSDS), it should be noted that there is now a consensus that the definition of bipolar disorder (particularly bipolar II disorder) within DSM–IV is overly restrictive and, further, that these questionnaires were designed to identify broadly defined hypomania. The American Psychiatric Association’s proposed draft of DSM–5 (www.dsm5.org) recommends a broadening of the diagnostic criteria for hypomania to include increased activity/energy as an additional core (or ‘gate’) symptom and the removal of antidepressant-associated hypomania as an exclusion criterion for hypomania. It is therefore likely that the gold-standard (DSM–IV) definition we have used in this study is too restrictive and it is possible that the HCL–32 and BSDS may have had improved positive predictive values had we used broader diagnostic criteria for hypomania. Further work on these instruments is important because there is currently a vogue for the unsupervised use of these questionnaires by patients (for example, via the internet) and GPs are increasingly faced with having to explain to people why scoring highly on such questionnaires may or may not be diagnostic of bipolar disorder.
The broad clinical spectrum of bipolar disorder
Major depressive disorder may be a heterogeneous diagnostic grouping that contains a substantial proportion of individuals who have subtle (but clinically relevant) bipolar features that fall just below the DSM–IV diagnostic threshold for bipolar disorder. Reference Smith, Ghaemi and Craddock35 Several recent epidemiological studies support the view that mild or ‘subthreshold’ features of bipolar disorder in people with a diagnosis of major depression are relatively common and clinically important.
In the latest wave of the Munich Early Developmental Stages of Psychopathology (EDSP) Study, 202 participants (41.4%) out of 488 identified with DSM–IV major depressive disorder fulfilled diagnostic criteria for ‘subthreshold bipolar disorder’. Reference Zimmermann, Bruckl, Nocon, Pfister, Lieb and Wittchen36 The criteria for subthreshold bipolar disorder in this study were: major depression, plus hypomania defined as ‘at least 4 days of either elated or expansive mood that caused problems or that was noticed by others (plus <3 other manic symptoms), or unusually irritable mood plus at least 3 other manic symptoms (not observed by others)’. These participants with subthreshold bipolar disorder differed from the remaining participants with major depressive disorder on a number of clinical variables. As a group, they had a significantly higher rate of family history of mania, higher rates of nicotine dependence and alcohol use disorders, higher rates of panic disorder, a tendency to more frequent criminality and a greater prospective risk of converting to DSM–IV bipolar disorder. This suggests that they represent a clinically important bipolar subgroup that is intermediate between DSM–IV bipolar disorder and DSM–IV major depressive disorder.
Similar findings were observed in the Zurich Longitudinal Study that used two definitions of hypomania that were less restrictive than the DSM–IV definition of hypomania (the so-called ‘Strict Zurich’ and ‘Broad Zurich’ criteria). Reference Angst, Gamma, Bennazzi, Ajdacic, Eich and Rossler37 Under DSM–IV criteria for hypomania, 7.4% of the Zurich cohort fulfilled criteria for bipolar II disorder but using the Strict Zurich criteria this figure rose to 23.7% and according to the Broad Zurich criteria the figure was 49.2%. Reference Angst, Gamma, Bennazzi, Ajdacic, Eich and Rossler37
In the US National Comorbidity Replication Study, Merikangas and colleagues defined subthreshold bipolar disorder as hypomania without a history of major depression or with fewer symptoms than required for DSM–IV hypomania. Reference Merikangas, Akiskal, Angst, Greenberg, Hirschfeld and Petukhova38 They found lifetime prevalence rates of 1.0% for bipolar I disorder, 1.1% for bipolar II disorder and 2.4% for subthreshold bipolar disorder. Participants with subthreshold bipolar disorder were not clinically benign. They had frequent psychiatric comorbidity, moderate to severe clinical severity, significant role impairment and only rarely had been prescribed mood stabilising medication. Furthermore, almost 40% of study participants with a history of major depressive disorder also had a history of subthreshold hypomania and these participants had a younger age at onset, more episodes of depression and higher rates of comorbidity. Reference Angst, Cui, Swendsen, Rothen, Cravchik and Kessler39
Our finding that people with major depressive disorder from primary care with a history of subdiagnostic manic symptoms were different from individuals with major depressive disorder with no or minimal history of manic symptoms on some clinical features and on several measures of both psychosocial functioning and quality of life is consistent with the findings in the Zurich longitudinal study, Reference Angst, Gamma, Bennazzi, Ajdacic, Eich and Rossler37 the Munich EDSP Study Reference Zimmermann, Bruckl, Nocon, Pfister, Lieb and Wittchen36 and the National Comorbidity Replication Study. Reference Merikangas, Akiskal, Angst, Greenberg, Hirschfeld and Petukhova38,Reference Angst, Cui, Swendsen, Rothen, Cravchik and Kessler39 Taken together, these studies suggest that low-grade, subdiagnostic levels of manic symptoms in people with major depressive disorder are clinically important and are associated with a more morbid illness course, poorer functioning and worse quality of life.
Although in this study we have used DSM–IV definitions of bipolar disorder as the gold-standard diagnoses, as noted above, there are limitations with a threshold approach to diagnosing bipolar disorder. One possible interpretation of our findings is that they provide support for a dimensional view of bipolar disorder that goes beyond the use of formal (and somewhat arbitrary) DSM–IV categories and thresholds. It may be that ICD–11 and DSM–5 should incorporate the measurement of dimensions of bipolar symptoms into the diagnostic criteria for both recurrent major depressive disorder and bipolar disorder.
A further suggestion is that assessing manic symptoms should become part of the routine diagnostic assessment of all individuals presenting with depression and that these assessments should guide treatment, for example, with regard to antidepressants. If we extrapolate from studies of DSM–IV bipolar depression, it is possible that many people with major depressive disorder who also have subdiagnostic bipolar features will not benefit from antidepressant therapy and may even do worse in the longer term because antidepressants could induce a course of depressive disorder with more frequent relapses and worsening mood instability. This is potentially a very large group of people and it is important that future research is less constrained by strict DSM–IV diagnoses and instead tries to evaluate the likely usefulness (or harm) caused by antidepressants in those people with depression who have subthreshold or mild features of bipolar disorder.
Strengths of this study
This is the first large-scale, systematic assessment of bipolar features in individuals with depression within a UK primary care setting. We were careful to recruit from several practices with a spread of participants from different social and economic backgrounds and we carried out formal diagnostic assessments on a representative subsample. As noted earlier, the two-stage methodological approach recommended by Dunn and colleagues Reference Dunn, Pickles, Tansella and Vazque-Barquero28 allowed us to obtain three increasingly conservative estimates of the likely prevalence of unrecognised bipolar disorder within our sample.
Limitations of this study
There are several limitations in this study. Only 18.5% of the 3117 people we invited to take part volunteered and returned their questionnaires. In general, volunteers for this study were similar to non-volunteers in terms of age, gender, time since diagnosis, medication use and medical comorbidity (Table 1). However, volunteers were significantly more likely to be taking antidepressant medication than non-volunteers. This could have several implications. It may suggest that those who volunteered had a more severe form of depressive illness; that they were more likely to report low-grade manic symptoms which were being caused by antidepressants; that they had depression which was treated by antidepressants and they were therefore more motivated to take part in a research study; or even that they were more interested in taking part because their current antidepressant treatment was ineffective. It is also possible, however, that individuals with bipolar disorder were overrepresented in the group who did not volunteer because they were resistant to the possibility of receiving this diagnosis during the study.
Similarly, from the group of participants who were invited to interview, those who were interviewed were similar to those who were not interviewed in terms of gender, ethnicity and mean HCL–32 and BSDS scores but were significantly older as a group. This age difference (although relatively small at only 4.1 years) could make it more likely that the interviewed group would contain more individuals with bipolar disorder.
Implications
In summary, our findings suggest that a significant minority of primary care patients with a working diagnosis of unipolar depression (between 3.3 and 21.6%) may have an undiagnosed DSM–IV bipolar disorder. Across the UK, this could represent a large number of individuals. Given the likelihood that many of these individuals are receiving antidepressants as monotherapy (which may be at best unhelpful and at worst harmful), it will be important that GPs are supported in developing strategies to ensure that their patients with depression receive the correct diagnosis with regard to the possibility of a primary bipolar illness. We also found that the HCL–32 and BSDS screening questionnaires had relatively low positive predictive values for DSM–IV bipolar disorder but it is possible that they could be useful for identifying broader definitions of bipolar disorder. Finally, in keeping with several other studies from around the world, we found that subthreshold features of bipolar disorder were relatively common in individuals with unipolar depression (even in primary care) and were associated with a more morbid course of illness and greater psychosocial and quality of life impairments. These findings have important implications for the classification, assessment and treatment of large numbers of people with depression managed in both primary and secondary care settings.
Funding
Funded by an MRC/Welsh Assembly Government Partnership Award (2008–2010). D.J.S. is funded by a Postdoctoral Fellowship from the National Institute of Health Research (NIHR).









eLetters
No eLetters have been published for this article.