Impact statement
Global best practices promote the training of psychiatry trainees in various techniques of psychotherapy and its incorporation into the training curriculum, hence the need to assess the extent and factors associated with the completion of psychotherapy training among early career psychiatrists (ECPs). Almost half of the ECPs in Nigeria had some form of psychotherapy training, however, only a few had full psychotherapy training. This study reveals the need for the inclusion of mandatory psychotherapy in the current psychiatry training curriculum, which will consequently improve psychiatric practice and decrease the treatment gap in mental healthcare. This inclusion will go a long way in improving the quality of holistic care delivered to mental health patients by ECPs.
Introduction
Nigeria is a low and middle-income country in West Africa with an estimated population of 40 million people living with mental disorders, which span across mild to severe forms (Lansana, Reference Lansana2017). Interventions to support people with mental disorders may require psychotherapy alone or in combination with other biomedical therapies (Madu, Reference Madu2016). Despite the high prevalence of mental disorders, Nigeria has only about 250 Nigerian-trained and qualified psychiatrists, 200 psychiatry trainees, and 319 licensed clinical psychologists (Bakare, Reference Bakare2021; Coker, Reference Coker2022). As part of their clinical education, psychiatric trainees should be well-equipped with psychotherapeutic techniques. Psychotherapy is a useful therapeutic resource that, over time, has evolved and expanded, and is currently considered a mainstay of treatment for mental disorders (Locher et al., Reference Locher, Meier and Gaab2019). Although recent advances in biological psychiatry and neuroscience have put pharmacotherapy at the forefront giving it more clinical consideration, psychotherapy remains a widely accepted and evidence-based form of treatment for mental disorders (Tavakoli, Reference Tavakoli2014). Psychiatrists and psychiatry trainees have a critical role in the management of individuals with mental disorders, as they represent a significant part of mental healthcare providers capable of providing integrative pharmacotherapy and psychotherapy (Locher et al., Reference Locher, Meier and Gaab2019). Despite this proviso, a considerable number of psychiatrists seem to lack skills in specialized psychotherapeutic techniques and seem to shy away from conducting this form of intervention (Madu, Reference Madu2016).
According to the Specialist Training General Psychiatry curriculum of the National Postgraduate Medical College of Nigeria, the minimum duration of psychiatry training is 4 years. Successfully passing the primary examination qualifies a doctor to commence residency training. The junior residency training is expected to last a minimum of 24 months, and after passing the part 1 examination, trainees proceed to senior residency training for another 24 months, at the minimum. At the end of the senior residency training, the part 2 examinations are written, and successful trainees are awarded the College Fellowship in Psychiatry (FMCPsych).
To qualify for the part 1 examination, a minimum of 6 months rotation in adult psychiatry, 3 months rotation in neurology, and 3 months in each of any 5 out of the 7 following core rotation areas is required: child psychiatry, psychiatry of later life, forensic psychiatry, community psychiatry, substance use psychiatry, emergency psychiatry and consultation-liaison psychiatry. During the senior residency training, the two outstanding core rotations are completed in 6 months, 3 months rotation in a subspecialty area apart from intended subspecialization, 3 months elective rotation and the remaining 12 months is expected to be in the area of intended subspecialization. Although the curriculum incorporates psychotherapy training during the postgraduate training, it does not include psychotherapy as one of the mandatory rotations and it is unclear how well this is supervised, considering the limited number of psychotherapists and psychologists within the country (NPMCN, 2018). Psychotherapy is mostly conducted by psychologists. Previously, concerns have been raised that psychiatrists who lack psychotherapeutic skills will be unable to offer appropriate care to the burgeoning number of individuals with mental disorders if all they continue to offer is pharmacotherapy (Holmes et al., Reference Holmes, Mizen and Jacobs2007).
In Nigeria, the National Postgraduate Medical College of Nigeria and the West Africa College of Physicians are the two recognized institutions that coordinate and superintend postgraduate medical education programs (Okonofua, Reference Okonofua2018). Postgraduate psychiatry training has existed in Nigeria for over four decades. Nigeria has over 20 postgraduate psychiatry training centers with variations in the exposure to clinical psychotherapy training due to the absence of a consistent psychotherapy evaluation program beyond course modules. Psychotherapy was incorporated into the junior postgraduate psychiatry training in Nigeria, but the program does not address the exact duration of psychotherapy training within the first 24 months period for junior residency (NPMCN, 2018).
Little is known about psychotherapy training in Nigeria, leading to the dire need to assess the views and experiences of ECPs in Nigeria on their psychotherapy curriculum and training.
To address this, this study aimed to investigate the access to, and experiences with, psychotherapy in the various training centers across Nigeria, namely:
-
i) To determine the extent to which psychotherapy training is included in psychiatry training programs in Nigeria;
-
ii) To determine the factors associated with the completion of psychotherapy training by psychiatric trainees in Nigeria.
Methods
This has been a cross-sectional study, part of a larger international study, the World Psychotherapy Survey. Study participants were ECPs recruited from the database (containing the names and contact details) of the ECP section of the Association of Psychiatrists in Nigeria (APN). In Nigeria, ECP is defined as psychiatry trainees (those currently undertaking residency training) and psychiatrists within 5 years post qualification from both postgraduate training colleges (National Postgraduate Medical College of Nigeria, Faculty of Psychiatry; West African College of Physicians, Faculty of Psychiatry). There is no age criteria in this definition.
The questionnaire was distributed via email to ECPs between November 2021 and February 2022 through a google form. The questionnaire was developed for the World Psychotherapy Survey conducted by the Early Career Psychiatrists Section of the World Psychiatric Association (Eissazade et al., Reference Eissazade, Shalbafan and Eftekhar Ardebili2021; Rai et al., Reference Rai, Karki and Pinto da Costa2021; Belinati Loureiro et al., Reference Belinati Loureiro, Ratzke, Nogueira Dutra, Mesadri Gewehr, Cantilino and Pinto da Costa2023; Kaya et al., Reference Kaya, Tasdelen, Ayik and Pinto da Costa2023). The self-administered questionnaire has 16 items covering three areas: i) socio-demographics, ii) psychotherapy training (types and modalities) and iii) satisfaction with psychotherapy training.
Participation in the survey was voluntary, and all information was kept confidential.
Data was transferred to the statistical package for social sciences version 20 (SPSS 20) for data analysis. Descriptive statistics were used to report the socio-demographics of the study participants, types and modalities of psychotherapy training received and training satisfaction. Non-parametric tests (chi-square and Fisher’s exact) were used to determine factors associated with the modalities of psychotherapy training.
Results
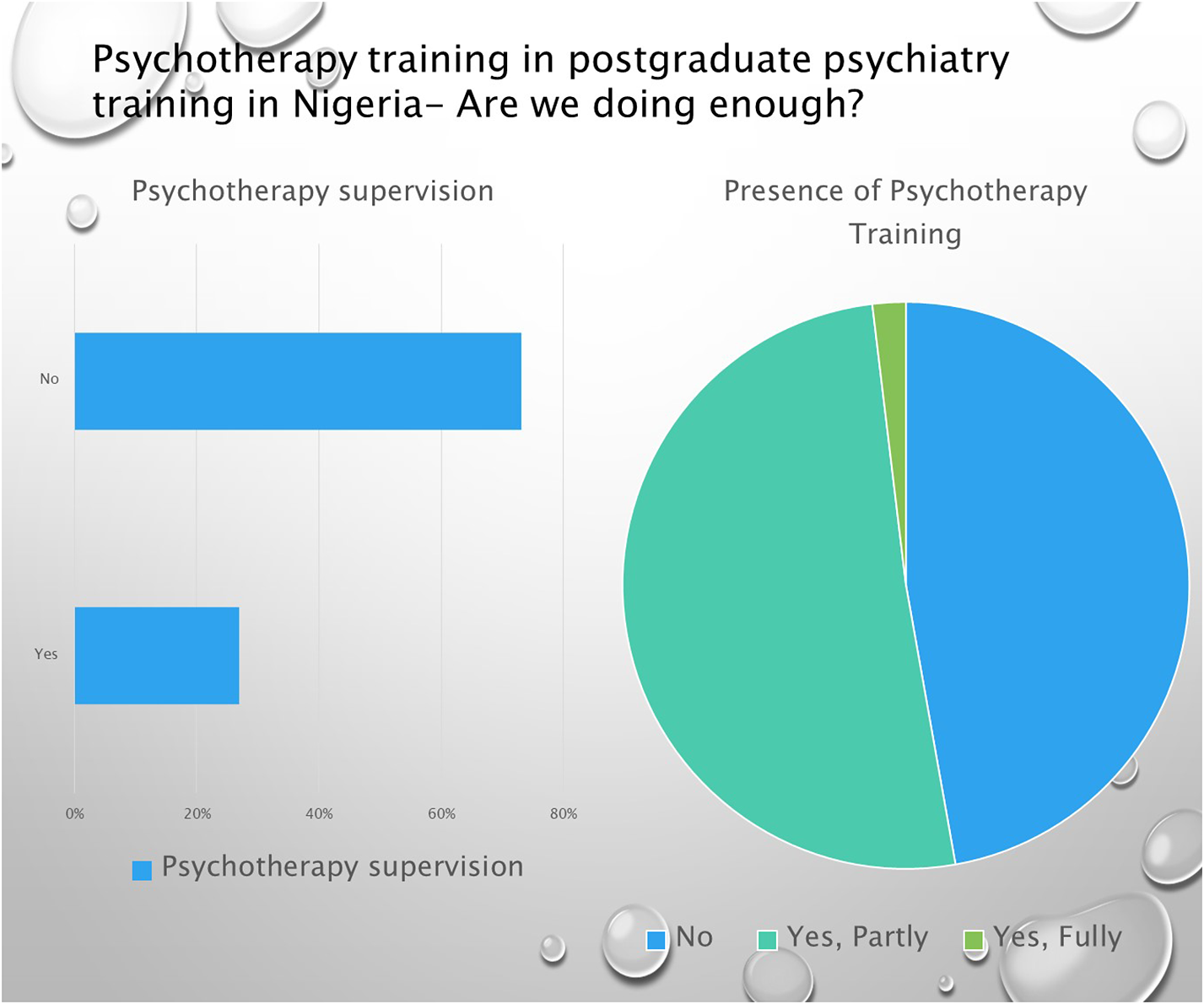
The survey was distributed to 252 members of the ECP section of the APN. One hundred and eight participants submitted the completed survey form, giving a response rate of 42.9%. Fifty percent of the participants were males and 50% were females. The majority, 56.7% (n = 59) of participants, were within the 36–45 years of age bracket. Among the professionals, psychiatry trainees accounted for 73.2% (n = 79), and the psychiatrists within their first 5 years after training for 26.8% (n = 29). Of the study participants, most (n = 86, 79.6%) reported awareness of the inclusion of psychotherapy training during the residency training program in Nigeria and most (n = 60, 71.4%) reported psychotherapy training as mandatory. More than half (n = 57, 52.8%) of participants had psychotherapy training, whether completed or partial (which is the case in the majority of the cases), during their residency training period (during junior residency training where it is included in their training curriculum), and only three (2.8%) completed psychotherapy training during residency (Table 1).
Table 1. Participants socio-demographics and psychotherapy training experience

NR: Not responded.
Where psychotherapy training was available during the junior residency training program, it was fully funded by the participants in more than half (n = 61, 56.5%) of the cases. Psychotherapy training was given in theory in the majority of the cases, with cognitive behavioral therapy being the most taught form of psychotherapy (Table 2).
Table 2. Details on the format of training

Psychotherapy supervision
Of the participants who received psychotherapy training, about one-third received supervision for their training. To these, training supervision was mandatory for only 48% (n = 14) of the participants. Training was mostly given in groups and lasted less than 50 hours in total (Table 3).
Table 3. Psychotherapy supervision

Factors associated with mandatory psychotherapy training
Where psychotherapy training was mandatory, it also tended to have optional supervision (p = 0.027), which was funded by the participants (p = 0.002). Other factors such as the psychiatry specialty, type of psychotherapy training available, and whether training was theoretical or practical did not have any association with the training being either mandatory or optional (Table 4).
Table 4. Factors associated with mandatory psychotherapy training

F, Fisher’s exact test.
Discussion
Main findings
Despite over half of the participants stating that psychotherapy training was included in their psychiatry postgraduate training and as a mandatory requirement, just about half received some form of psychotherapy training, and only 3% of the participants in Nigeria had full psychotherapy training. This might be a result of this mandatory training being self-funded as well as being theoretical in nature in the majority of the cases.
Despite the relatively low number, all qualified psychotherapists undertook self-sponsored psychotherapy training. Mandatory psychotherapy training was associated with it being self-funded and mandatory supervision of the training. Despite this, the completion rate was poor, indicating that priority was not being given to psychotherapy training in Nigerian psychiatry postgraduate training. These findings also show a general dissatisfaction with the psychotherapy training received during the training period.
Comparison with other literature
There is generally less emphasis on psychotherapy training during postgraduate training in Nigeria than in other countries, as it is not mandatory in the curriculum (Jain et al., Reference Jain, Mazhar and Uga2012).
The findings from this study in Nigeria are consistent with the results from this survey in Nepal, where one-third of ECPs received psychotherapy training (Rai et al., Reference Rai, Karki and Pinto da Costa2021). The present study also observed that psychotherapy training varies in different training institutions and was not made mandatory, with low supervision rates. However, findings from this survey in Iran reported that almost all participants had mandatory psychotherapy training (Eissazade et al., Reference Eissazade, Shalbafan and Eftekhar Ardebili2021). While there are a lot of constraints in psychotherapy training during psychiatry training, which includes poor funding and supervision, over half of the respondents in Nigeria sponsored their own psychotherapy training. This is similar to the results from a psychotherapy survey conducted across Europe, where trainees reported self-funding for psychotherapy training (Giacco et al., Reference Giacco, Luciano and Del Vecchio2012). Nonetheless, many participants in Nigeria considered that the payment for the psychotherapy training should not be done by the participants themselves and wished the current training be improved upon through full incorporation and implementation of a uniform, mandatory, well-supervised accredited psychotherapy curriculum during postgraduate training in line with global best practices. Evidence suggests that online psychotherapy training provides equal knowledge, competency and confidence in psychotherapy when compared with supervised training. This, therefore, may create an option for a cheaper form of training that can be undertaken by psychiatry trainees and ECPs in low- and middle-income countries (Bennett-Levy et al., Reference Bennett-Levy, Hawkins, Perry and Mills2020).
Implications of the findings for practice, policies and research
While there are different psychotherapy modalities, psychotherapy training should focus on common models such as cognitive behavioral therapy, family therapy and interpersonal therapy as well as group and individual therapy techniques. In Nigeria, psychiatry trainees and ECPs undergoing psychotherapy training are exposed to the common models listed above where such training exists. There is a need for the current psychiatry postgraduate training curriculum to make psychotherapy training mandatory and ensure adequate supervision as a requirement for qualification as a psychiatrist. Increased attention should be given to psychotherapy training in the postgraduate psychiatry training program curriculum. This will improve psychiatric practice and decrease the treatment gap that exists in mental health care.
Strengths and limitations
This is the first study to investigate psychotherapy training in Nigeria; however, its limitations are the relatively low response rate and small sample size. This affects the power of the study and the reliability of the measures of associations used to determine factors affecting psychotherapy training.
Conclusions
Psychotherapy training offered during psychiatry postgraduate training, though present in the postgraduate curriculum, lacks structure and mandatory supervision and is not mandatory for qualification as a psychiatrist in Nigeria. ECPs are largely unsatisfied with the training and tend to seek further training outside of the postgraduate training. Despite this, very few are qualified psychotherapists. This highlights the need to improve the delivery of the training curriculum as it pertains to psychotherapy training so as to decrease the treatment gap in psychiatry present in Nigeria.
Data availability statement
The data used to support the findings of this study are included within the article.
Acknowledgements
The authors acknowledge the Early Career Psychiatrists Section of the World Psychiatric Association for the development of the survey instrument.
Author contribution
All authors contributed to different aspects of this manuscript. M.P.d.C. conceived this study and its design and all authors were involved in data collection. Analysis and interpretation of data were performed and written by F.N.A., O.O.A., U.B.M. and M.Y.M. while the rest of the literature was written by F.N.A., M.I.O., A.S.K. and M.O.S. F.N.A., O.O.A., A.S.K. and M.P.d.C. edited the final manuscript. All authors agree to be accountable for all aspects of this manuscript.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interest
The authors declare none.
Ethical approval
Ethical approval was obtained from the Ethics Review Committee of the University of Ilorin Teaching Hospital, Kwara State, Nigeria.







Comments
Royal Cornhill Hospital
Cornhill Road
Aberdeen
AB25 2ZH
United Kingdom
06-02-2023
The Editors-in-Chief,
Cambridge Prisms: Global Mental Health
COVER LETTER
Dear Editors,
We wish to submit our manuscript entitled ‘’Psychotherapy training in Postgraduate Psychiatry training in Nigeria’’ for consideration for publication in your reputable journal.
The manuscript is being published as part of a larger international study (World Psychotherapy Survey). This study is the first of its kind in Nigeria and our contribution to an ongoing worldwide survey.
Psychotherapy undoubtedly forms a crucial part of psychiatry training. Global best practice would be to promote structured, supervised training of psychiatric trainees in various psychotherapy techniques as an integral part of the training curriculum.
Within the context of psychiatric training in Nigeria, very little is known concerning the experience of psychiatric trainees regarding their psychotherapy training. Hence, this study contributes to the broader global literature on psychotherapy training as well as our specific understanding of the experiences of Nigerian psychiatric trainees and Early Career Psychiatrists with respect to their psychotherapy training.
The identified factors related to completion of psychotherapy training among psychiatric trainees will aid training institutions to standardize the psychotherapy curriculum as well as provide necessary supervision support for trainees during better structured psychotherapy training.
As we are certain that the content of our manuscript fits the remit of your journal, it is our hope that you will find it suitable for publication.
Thank you.
Yours Sincerely,
Dr Oluwadolapo Olujinmi Adedapo
(Corresponding Author)
dradedapodolapo@gmail.com
07454952279