Introduction
Depressive disorders are ranked as the third leading cause of ‘years lived with disability’ worldwide (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). This is due in part to their high prevalence, with a lifetime prevalence of 10.6% and a 12-month prevalence of 4.5% for major depressive disorder (MDD) (Bromet et al., Reference Bromet, Andrade, Bruffaerts, Williams, Scott, de Jonge, Stein and Kessler2018). Additionally, MDD is often characterised by a recurrent course (Hardeveld et al., Reference Hardeveld, Spijker, De Graaf, Nolen and Beekman2013), suggesting the importance of taking a lifespan perspective when studying MDD (Hardeveld et al., Reference Hardeveld, Spijker, De Graaf, Nolen and Beekman2010; Bockting et al., Reference Bockting, Hollon, Jarrett, Kuyken and Dobson2015).
Comorbidity with other mental disorders is high in individuals with MDD (e.g. Grant, Reference Grant1995; Kessler et al., Reference Kessler, Berglund, Demler, Jin, Koretz, Merikangas, Rush, Walters and Wang2003; Alonso and Lépine, Reference Alonso and Lépine2007; Bromet et al., Reference Bromet, Andrade, Bruffaerts, Williams, Scott, de Jonge, Stein and Kessler2018). Since MDD has a rather late median age of onset (AOO) (Kessler and Bromet, Reference Kessler and Bromet2013), i.e. around 38 years (Bromet et al., Reference Bromet, Andrade, Bruffaerts, Williams, Scott, de Jonge, Stein and Kessler2018), other mental disorders with earlier AOOs, such as anxiety disorders (Goodwin, Reference Goodwin2002; Bittner et al., Reference Bittner, Goodwin, Wittchen, Beesdo, Hofler and Lieb2004; Beesdo et al., Reference Beesdo, Bittner, Pine, Stein, Höfler, Lieb and Wittchen2007; Mathew et al., Reference Mathew, Pettit, Lewinsohn, Seeley and Roberts2011; Kessler et al., Reference Kessler, Avenevoli, McLaughlin, Green, Lakoma, Petukhova, Pine, Sampson, Zaslavsky and Merikangas2012; Gundel et al., Reference Gundel, Pedersen, Munk-Olsen and Dalsgaard2018) and behavioural disorders (including oppositional defiant disorder (ODD), conduct disorder (CD) and attention deficit hyperactivity disorder (ADHD)) (Kessler et al., Reference Kessler, Avenevoli, McLaughlin, Green, Lakoma, Petukhova, Pine, Sampson, Zaslavsky and Merikangas2012; Gundel et al., Reference Gundel, Pedersen, Munk-Olsen and Dalsgaard2018) often precede first-onset MDD. Assessing the clinical history of mental disorders in individuals with current MDD could provide valuable information regarding management and treatment strategies, especially since this history may be a prognostic marker of the further clinical course of MDD (Wittchen et al., Reference Wittchen, Beesdo, Bittner and Goodwin2003). Mental disorder comorbidity is predictive of depression outcomes, including impairment (Andrews et al., Reference Andrews, Henderson and Hall2001; Alonso et al., Reference Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, Bryson, de Girolamo, Graaf, Demyttenaere, Gasquet, Haro, Katz, Kessler, Kovess, Lépine, Ormel, Polidori, Russo, Vilagut, Almansa, Arbabzadeh-Bouchez, Autonell, Bernal, Buist-Bouwman, Codony, Domingo-Salvany, Ferrer, Joo, Martínez-Alonso, Matschinger, Mazzi, Morgan, Morosini, Palacín, Romera, Taub and Vollebergh2004; Kessler et al., Reference Kessler, Sampson, Berglund, Gruber, Al-Hamzawi, Andrade, Bunting, Demyttenaere, Florescu, de Girolamo, Gureje, He, Hu, Huang, Karam, Kovess-Masfety, Lee, Levinson, Medina Mora, Moskalewicz, Nakamura, Navarro-Mateu, Browne, Piazza, Posada-Villa, Slade, Ten Have, Torres, Vilagut, Xavier, Zarkov, Shahly and Wilcox2015) and suicidal thoughts and behaviours (Stein et al., Reference Stein, Fuetsch, Müller, Höfler, Lieb and Wittchen2001; Bolton et al., Reference Bolton, Pagura, Enns, Grant and Sareen2010; Kessler et al., Reference Kessler, Sampson, Berglund, Gruber, Al-Hamzawi, Andrade, Bunting, Demyttenaere, Florescu, de Girolamo, Gureje, He, Hu, Huang, Karam, Kovess-Masfety, Lee, Levinson, Medina Mora, Moskalewicz, Nakamura, Navarro-Mateu, Browne, Piazza, Posada-Villa, Slade, Ten Have, Torres, Vilagut, Xavier, Zarkov, Shahly and Wilcox2015). However, to our knowledge, no study has comprehensively examined the associations between a wide range of mental disorders with an onset before 12-month MDD diagnosis with multiple depression outcomes.
The overall aim of the present study is to examine associations between 12-month MDD, previous mental disorders and MDD outcomes. First, we examine the strength of associations between 12-month MDD and preceding individual lifetime mental disorders in the cross-national World Mental Health (WMH) surveys. Second, we examine whether previous mental disorders, i.e. with an onset prior to the respondent's age at interview, are predictive of current depression outcomes including impairment and suicidality.
Methods
WMH surveys
Data came from 29 cross-sectional surveys administered between 2001/2002 and 2015 in low/middle-income countries (Brazil, Bulgaria, Colombia, Colombia (Medellin), China (Shenzhen), Iraq, Lebanon, Mexico, Nigeria, Peru, Romania, South Africa and Ukraine) and high-income countries (Argentina, Australia, Belgium, France, Germany, Israel, Italy, Japan, the Netherlands, New Zealand, Northern Ireland, Poland, Portugal, Spain, Spain (Murcia), USA). A total of 145 990 respondents participated. Adults were selected based on multistage clustered area probability sampling designs designed to generate samples that were representative of the household populations in each country. Face-to-face interviews were conducted in respondent homes. The details of sampling methods in the different countries are described in detail elsewhere (Heeringa et al., Reference Heeringa, Wells, Hubbard, Mneimneh, Chiu, Sampson, Berglund, Kessler and Üstün2008; Pennell et al., Reference Pennell, Mneimneh, Bowers, Chardoul, Wells, Viana, Dinkelmann, Gebler, Florescu, He YanLing, Yue, Tomov, Saiz, Kessler and Üstün2008). The weighted average response rate across surveys was 69.5%. Informed consent was obtained according to protocols endorsed by local Institutional Review Boards. Further information on the surveys is provided in online Supplementary Table 1.
MDD and other comorbid DSM-IV diagnoses
The WHO Composite International Diagnostic Interview (CIDI), a fully structured interview administered by trained lay interviewers, was used to assess DSM-IV mental disorders (Kessler and Üstün, Reference Kessler and Üstün2004). Interviews were administered in two parts to diminish respondent burden. All respondents completed Part I, assessing MDD and other core mental disorders. Part II, assessing other disorders and disorder correlates, was administered to all respondents with any lifetime Part I diagnosis and a probability subsample of other respondents. Part II data were weighted to adjust for the undersampling of Part I non-cases. Analyses for this study were performed in the Part II sample (N = 80 190).
Since mental disorders are significantly correlated, which may be indicative of shared underlying vulnerability factors, a model-based approach of comorbidity of mental disorders was used (Krueger and Markon, Reference Krueger and Markon2006). Grouping of DSM-IV disorders was based on the underlying structure of disorders found previously in the WMH surveys (de Jonge et al., Reference de Jonge, Wardenaar, Lim, Aguilar-Gaxiola, Alonso, Andrade, Bunting, Chatterji, Ciutan, Gureje, Karam, Lee, Medina-Mora, Moskalewicz, Navarro-Mateu, Pennell, Piazza, Posada-Villa, Torres, Kessler and Scott2018). Given our focus on MDD, we separated two groups of distress disorders: depressive distress disorders (MDD and dysthymia (hierarchical)) and non-depressive distress disorders (generalised anxiety disorder (GAD) and post-traumatic stress disorder (PTSD)). Fear disorders included agoraphobia (non-hierarchical), panic disorder, social anxiety disorder, specific phobia and (childhood or adult) separation anxiety disorder. Externalising disorders included intermittent explosive disorder, ADHD, CD, ODD, alcohol abuse, alcohol dependence, drug abuse and drug dependence. The AOO of disorders was assessed using special recall probes that have been shown to yield more plausible distributions of AOO of disorders than conventional recall questions (Knäuper et al., Reference Knäuper, Cannell, Schwarz, Bruce and Kessler1999). Lifetime comorbid disorders were taken into account when they had an onset prior to the respondent's age at interview, regardless of whether or not they persisted into the past year.
Outcomes
Role impairment
Role impairment due to MDD was assessed with a modified version of the Sheehan Disability Scale (SDS) (Leon et al., Reference Leon, Olfson, Portera, Farber and Sheehan1997). This scale assesses impairment in different domains, namely home management, ability to work, ability to form and maintain close relationships, and social life, during the month in the past year when MDD was most severe. Severe impairment was defined as a score ⩾7 on a response scale of 0–10 for each domain. Respondents were defined as having any severe impairment if they scored ⩾7 in at least one domain. Additionally, respondents were asked how many days in the past year they were unable to work or carry out their normal activities because of their depression, i.e. days out of role (Ormel et al., Reference Ormel, Petukhova, Chatterji, Aguilar-Gaxiola, Alonso, Angermeyer, Bromet, Burger, Demyttenaere, de Girolamo, Haro, Hwang, Karam, Kawakami, Lépine, Medina-Mora, Posada-Villa, Sampson, Scott, Ustün, Von Korff, Williams, Zhang and Kessler2008).
Suicidal thoughts and behaviours
Respondents were asked whether they had ever seriously thought about suicide, and if so, whether they had ever made a suicide plan or attempted suicide. Respondents who reported these experiences were asked whether these experiences had also occurred in the past 12 months.
Statistical analysis
The actuarial method was used to calculate the median AOO of MDD in respondents with 12-month MDD. We used logistic regression to examine the association between 12-month MDD and other mental disorders (controlling for country of origin). If a specific disorder was not assessed in a particular country, that country was not included in that analysis; however, if a country assessed at least one of the disorders in a disorder group (e.g. fear disorders), the country was included in the analysis of that disorder group, and non-assessed disorders were assumed not to be present.
We also used logistic regression to examine the association between previous mental disorder groups and depression outcomes (role impairment and suicidality). Linear regression was used for days out of role due to MDD in the past year, a continuous outcome. The models included all disorder groups simultaneously. We tested three models: model 1 only controlled for country of origin of the participant; model 2 additionally adjusted for age and sex; and model 3 additionally adjusted for educational status, marital status and employment status.
In post-hoc analyses, we added depression characteristics, namely AOO of MDD, lifetime history of chronic MDD (duration of longest episode >2 years) and severity of MDD in the worst month of the past year (according to the Quick Inventory of Depressive Symptomatology Self Report (QIDS-SR)) (Rush et al., Reference Rush, Carmody and Reimitz2000), to model 3. Furthermore, in a previous study, current, but not remitted anxiety disorders and dysthymia, predicted MDD episode duration (ten Have et al., Reference Ten Have, Penninx, Tuithof, van Dorsselaer, Kleinjan, Spijker and de Graaf2017). As our main analyses include both remitted disorders and disorders that had onset prior to the current age but persisted into the past year, we distinguished remitted (i.e. no 12-month diagnosis) from current disorders in additional post-hoc analyses.
Results
Sample characteristics
A full description of the sample's characteristics stratified by 12-month MDD status is presented in online Supplementary Table 2. The number of respondents who met the criteria for 12-month MDD was 6684. The (weighted) prevalence of 12-month MDD was 4.9% (standard error (s.e.) = 0.1). Of the respondents with 12-month MDD, 66.8% were female. In this group, the median age of MDD onset was 38 years (interquartile range = 23–54) and 34.4% had a lifetime history of chronic MDD.
History of mental disorders
Among respondents with 12-month MDD, 92.0% (s.e. = 0.5) had a prior history of MDD, and 94.9% (s.e. = 0.4) had a history of any previous mental disorder (including previous MDD). After excluding prior MDD episodes, this percentage dropped to 64.6% (s.e. = 0.9). Compared to respondents without 12-month MDD, prevalence rates of all other mental disorders with an onset prior to the respondent's age at interview were statistically significantly increased in respondents with 12-month MDD. The ORs ranged from 1.7 (alcohol abuse) to 20.2 (dysthymia) (see Table 1). ORs were largest for depressive distress disorders (including previous MDD) (OR = 161.1; 95% CI 140.0–185.4; p < 0.001), followed by non-depressive distress disorders (OR = 7.4; 95% CI 6.8–8.0; p < 0.001), fear disorders (OR = 4.8; 95% CI 4.5–5.2; p < 0.001) and externalising disorders (OR = 2.3; 95% CI 2.1–2.5; p < 0.001).
Table 1. Lifetime prevalence of previous disorders among respondents with 12-month MDD and respondents without 12-month MDD

MDD, major depressive disorder; s.e., standard error; OR, odds ratio; CI, confidence interval.
Analyses controlled for country.
Role impairment
Overall impairment rates in respondents with 12-month MDD were 58.6% (s.e. = 0.9) for any severe impairment, 35.2% (s.e. = 0.9) for severe impairment in home management, 35.6% (s.e. = 0.9) for severe impairment in ability to work, 33.7% (s.e. = 0.9) for severe impairment in the ability to form and maintain close relationships, and 40.2% (s.e. = 0.9) for severe impairment in social life.
Among respondents with 12-month MDD, those with a previous depressive distress disorder were less likely to be severely impaired due to MDD in home management (OR = 0.6; 95% CI 0.4–0.8; p = 0.001), ability to work (OR = 0.6; 95% CI 0.4–0.8; p < 0.001) and social life (OR = 0.6; 95% CI 0.4–0.8; p < 0.001) compared to respondents without a previous mental disorder (see model 1, Table 2). However, the association between history of depressive distress disorders and ability to form and maintain close relationships was not statistically significant (OR = 0.7; 95% CI 0.5–1.0; p = 0.061). Respondents with a previous non-depressive distress disorder (GAD or PTSD) or fear disorder had significantly increased odds (ORs ranging from 1.3 to 1.7) of impairment due to MDD in all roles, compared to respondents without previous mental disorders. Respondents with a previous externalising disorder also had an increased risk of impairment in ability to work, social life and relationships (ORs = 1.2–1.3), but not of impairment in home management (OR = 1.0; 95% CI 0.8–1.2; p = 0.96). Adjustment for sex and age in model 2, and additionally for education, marital status and employment in model 3, did not change these findings (see Table 2).
Table 2. Association between previous disorders and severe role impairment
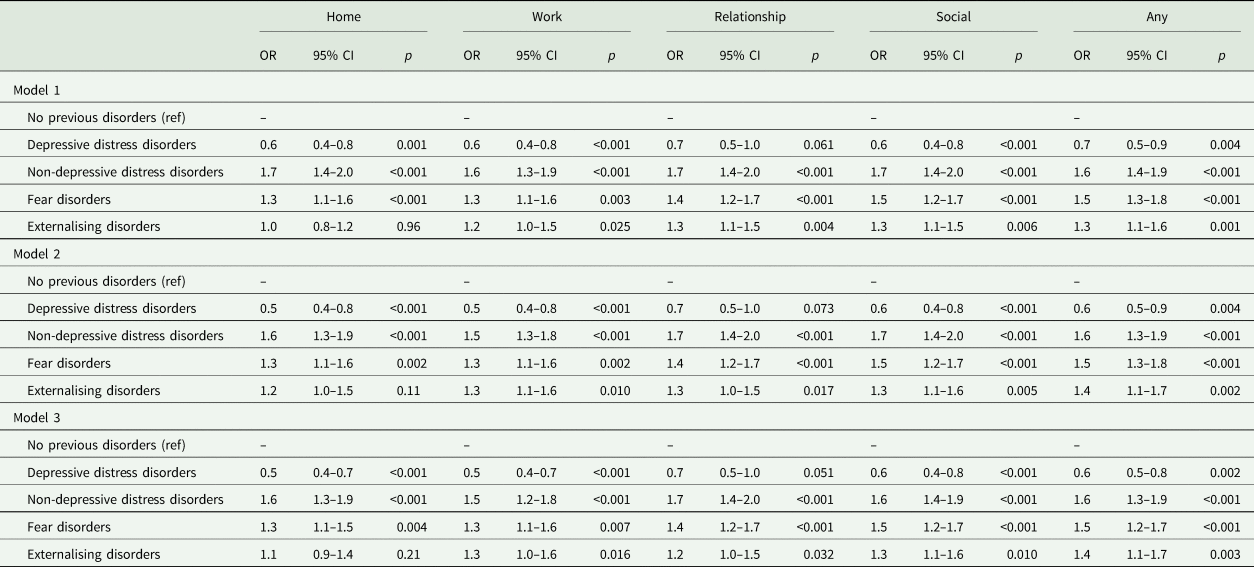
MDD, major depressive disorder; OR, odds ratio; CI, confidence interval.
Association between severe role impairment and previous depressive distress, non-depressive distress, fear or externalising disorders, among respondents with 12-month MDD.
Depressive distress disorders: major depressive disorder and dysthymia; non-depressive distress disorders: generalised anxiety disorder and post-traumatic stress disorder; fear disorders: agoraphobia, panic disorder, separation anxiety disorder, social anxiety disorder, specific phobia; externalising disorders: intermittent explosive disorder, attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, alcohol abuse, alcohol dependence, drug abuse and drug dependence.
Model 1: adjusted for country.
Model 2: adjusted for country, age, sex.
Model 3: adjusted for country, age, sex, education, marital status and employment status.
Days out of role
The mean number of days out of role in the past year due to MDD for participants with 12-month MDD was 36.4 (s.e. = 1.8). Compared to respondents with 12-month MDD without previous mental disorders, those with previous depressive distress disorders (B = 10.9; 95% CI 1.1–20.8; p = 0.030), non-depressive distress disorders (B = 16.6; 95% CI 8.4–24.8; p < 0.001) or fear disorders (B = 13.8; 95% CI 6.4–21.3; p < 0.001) had higher numbers of days out of role (online Supplementary Table 3). The number of days out of role was not significantly higher for respondents with previous externalising disorders (B = 5.1; 95% CI −2.5 to 12.6; p = 0.19). After adjustment for sex and age, the association for previous depressive distress disorders lost statistical significance (B = 9.3; 95% CI −0.3 to 18.8; p = 0.057). However, previous non-depressive distress disorders (B = 13.2; 95% CI 4.9–21.4; p = 0.002) and previous fear disorders (B = 14.1; 95% CI 6.8–21.4; p < 0.001) remained significant predictors of days out of role even in the fully adjusted model.
Suicidal thoughts and behaviours
Of all respondents with 12-month MDD, 13.2% (s.e. = 0.5) reported suicidal ideation in the past 12 months and 4.4% (s.e. = 0.3) and 2.6% (s.e. = 0.2), respectively, reported suicide plans and attempts over this period. Previous depressive distress disorders were not significantly associated with 12-month suicidal ideation, plan or attempt in any model (ORs = 0.9–1.3) (Table 3). Previous non-depressive distress disorders were associated with suicidal ideation, plan and attempts in respondents with 12-month MDD, but not all associations were statistically significant in each model (ORs = 1.3–1.7) (see Table 3). Previous fear disorders (ORs = 1.5–1.7) and previous externalising disorders (ORs = 1.9–2.9) were consistently associated with suicidal ideation, plan and attempt in all models.
Table 3. Association between previous disorders and suicidality
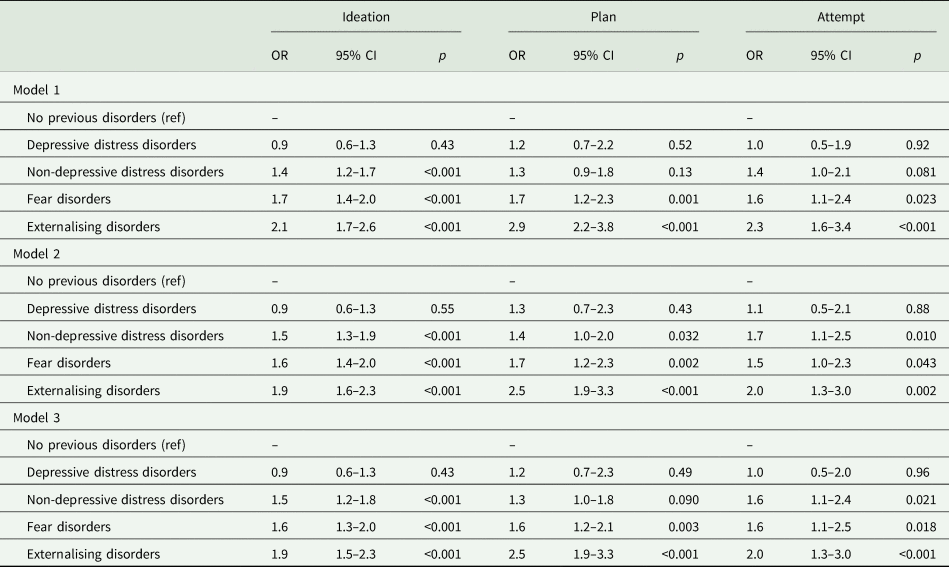
MDD, major depressive disorder; OR, odds ratio, CI, confidence interval.
Association between suicidality and previous depressive distress, non-depressive distress, fear or externalising disorders, among respondents with 12-month MDD.
Depressive distress disorders: major depressive disorder and dysthymia; non-depressive distress disorders: generalised anxiety disorder and post-traumatic stress disorder; fear disorders: agoraphobia, panic disorder, separation anxiety disorder, social anxiety disorder, specific phobia; externalising disorders: intermittent explosive disorder, attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, alcohol abuse, alcohol dependence, drug abuse and drug dependence.
Model 1: adjusted for country.
Model 2: adjusted for country, age, sex.
Model 3: adjusted for country, age, sex, education, marital status and employment status.
Post-hoc analyses including MDD characteristics
When depression characteristics were added to the models, a higher age of MDD onset and 12-month MDD severity were associated with role impairment due to MDD (online Supplementary Table 4). In this model, previous fear disorders were no longer associated with role impairment in any of the roles, except social life (OR = 1.2; 95% CI 1.0–1.5; p = 0.029). Associations between previous non-depressive distress disorders and previous externalising disorders with role impairment remained statistically significant (ORs = 1.1–1.4), with the exception of the association between previous externalising disorders and work impairment (OR = 1.1; 95% CI 0.9–1.4; p = 0.30).
Only previous fear disorders were associated with a higher number of days out of role compared to respondents with 12-month MDD without previous mental disorders (B = 7.2; 95% CI 0.0–14.4; p = 0.049) after additional adjustment for depression characteristics. Lifetime MDD chronicity and 12-month MDD severity were strongly related to days out of role in this model (online Supplementary Table 5).
Additionally, previous non-depressive distress disorders were no longer statistically significantly related to suicidal thoughts and behaviours. However, previous fear and externalising disorders (ORs = 1.4–2.1), as well as MDD severity, were associated with suicidal ideation, plans and attempts (online Supplementary Table 6).
Post-hoc analyses on remitted disorders
After separating previous disorders into those still present in the past 12 months and those that had remitted, 52.3% (s.e. = 0.9) of participants with 12-month MDD had any current comorbidity, while 12.3% (s.e. = 0.5) only had remitted comorbidity. Previous mental disorders were only associated with role impairment when they were also present in the past 12 months, with the exception of remitted externalising disorders and social impairment (OR = 1.3; 95% CI 1.0–1.6; p = 0.027) (Table 4). Similarly, days out of role due to MDD and suicidal thoughts and behaviours were related to current, but not remitted, fear disorders (online Supplementary Table 7 and Table 5). Current externalising disorders were associated with suicidal ideation (OR = 2.0; 95% CI 1.5–2.5; p < 0.001) and plans (OR = 2.6; 95% CI 1.8–3.8, p < 0.001), but not with suicide attempts (OR = 1.6; 95% CI 0.9–2.7; p = 0.10). Remitted externalising disorders, however, were only significantly associated with suicide attempts (OR = 1.7; 95% CI 1.0–3.0; p = 0.0498) and not with suicidal ideation (OR = 1.3; 95% CI 1.0–1.8; p = 0.06) or plans (OR = 1.5; 95% CI 1.0–2.4; p = 0.07) (Table 5).
Table 4. Association between previous disorders, divided into remitted or current comorbid disorders, and severe role impairment
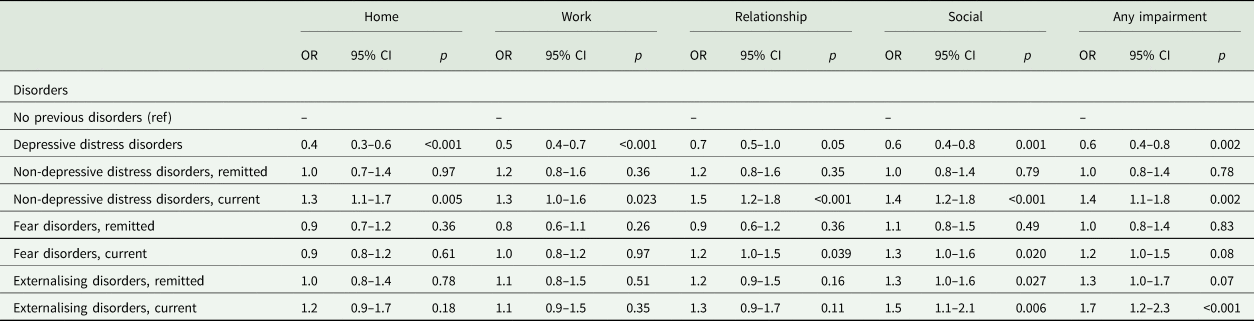
MDD, major depressive disorder; OR, odds ratio; CI, confidence interval.
Association between severe role impairment and previous depressive distress, non-depressive distress, fear or externalising disorders, among respondents with 12-month MDD. Previous disorders are divided into remitted and current disorders.
Depressive distress disorders: major depressive disorder and dysthymia; non-depressive distress disorders: generalised anxiety disorder and post-traumatic stress disorder; fear disorders: agoraphobia, panic disorder, separation anxiety disorder, social anxiety disorder, specific phobia; externalising disorders: intermittent explosive disorder, attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, alcohol abuse, alcohol dependence, drug abuse and drug dependence.
Analyses are adjusted for country, age, sex, education, marital status, employment status and MDD characteristics (age of onset, chronicity, severity).
Table 5. Association between previous disorders, divided into remitted or current comorbid disorders, and suicidality
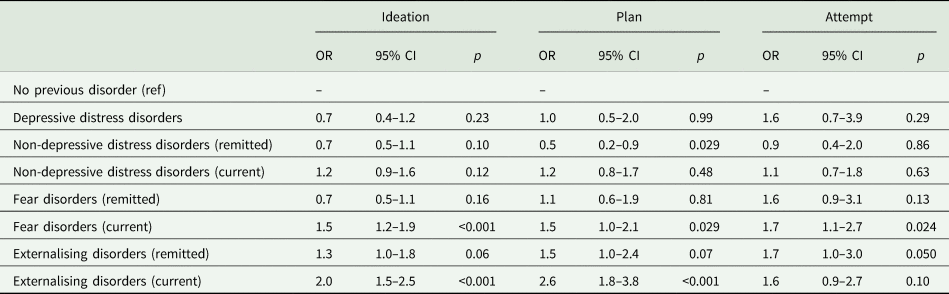
MDD, major depressive disorder; OR, odds ratio; CI, confidence interval.
Association between suicidality and previous depressive distress, non-depressive distress, fear or externalising disorders, among respondents with 12-month MDD. Previous disorders are divided into remitted and current disorders.
Depressive distress disorder: major depressive disorder and dysthymia; non-depressive distress disorder: generalised anxiety disorder and post-traumatic stress disorder; fear disorder: agoraphobia, panic disorder, separation anxiety disorder, social anxiety disorder, specific phobia; externalising disorders: intermittent explosive disorder, attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, alcohol abuse, alcohol dependence, drug abuse and drug dependence.
Analyses adjusted for country, age, sex, education, marital status, employment status and MDD characteristics (age on onset, chronicity and severity).
Discussion
To our knowledge, this is the first epidemiological study that comprehensively examined the history of mental disorders in individuals with current MDD and their impact on depression outcomes. The results of this study show the importance of applying a lifespan perspective when studying MDD. We found that 95% of respondents with 12-month MDD had a previous mental disorder. Many had suffered from previous MDD episodes, confirming the recurrent and/or chronic nature of MDD and demonstrating that first-onset cases are rare among people with a 12-month MDD episode. However, even after excluding previous MDD, 65% of respondents reported previous mental disorders. Compared to respondents without MDD, those with MDD had higher lifetime prevalence rates of all other individual mental disorders.
Previous disorders and depression outcomes
Importantly, previous mental disorders in respondents with MDD were associated with impairment and suicidality. Previous non-depressive distress disorders and fear disorders were most strongly associated with impairment. These results are consistent with other studies that reported high impairment rates in individuals with MDD and comorbid anxiety disorders (Wittchen et al., Reference Wittchen, Beesdo, Bittner and Goodwin2003; Van Der Werff et al., Reference Van Der Werff, Verboom, Penninx, Nolen and Ormel2010; Kessler et al., Reference Kessler, Sampson, Berglund, Gruber, Al-Hamzawi, Andrade, Bunting, Demyttenaere, Florescu, de Girolamo, Gureje, He, Hu, Huang, Karam, Kovess-Masfety, Lee, Levinson, Medina Mora, Moskalewicz, Nakamura, Navarro-Mateu, Browne, Piazza, Posada-Villa, Slade, Ten Have, Torres, Vilagut, Xavier, Zarkov, Shahly and Wilcox2015) and reinforce the clinical importance of anxiety symptoms in MDD (Gaspersz et al., Reference Gaspersz, Nawijn, Lamers and Penninx2018). Further, previous non-depressive distress, fear and externalising disorders were related to past-year suicidal ideation, plans and attempts in respondents with 12-month MDD. The strongest associations were found for previous externalising disorders, consistent with other epidemiological studies that found associations between externalising psychopathology and suicide attempts independent from internalising psychopathology (Verona et al., Reference Verona, Sachs-Ericsson and Joiner2004; Hills et al., Reference Hills, Cox, McWilliams and Sareen2005, Reference Hills, Afifi, Cox, Bienvenu and Sareen2009).
Surprisingly, previous depressive distress disorders were associated with less frequent severe role impairment. However, respondents with previous depressive distress disorders did have a higher number of days out of role compared to respondents with first-onset MDD, although this association did not remain statistically significant after adjustment for covariates. Individuals with recurrent or chronic MDD may be less likely to report severe impairment in different domains as a result of habituation or adaptation to depressive episodes (Kruijshaar et al., Reference Kruijshaar, Hoeymans, Bijl, Spijker and Essink-Bot2003). For example, it is possible that recurrent or chronic MDD has led to the individual having reduced activity in some roles (e.g. being under-employed); an ability to function adequately in a reduced role may or may not be interpreted as impairment. However, individuals with recurrent or chronic MDD may also have reduced insight regarding impairment. The finding that people with previous depression do report a higher number of days out of role, a more objective measure of impairment, argues that reduced insight may play some role, yet this is a post-hoc speculation. Previous research has found conflicting results, with some other studies reporting that recurrence of MDD was related to increased functional impairment and work disability (Merikangas et al., Reference Merikangas, Wicki and Angst1994; Rytsälä et al., Reference Rytsälä, Melartin, Leskelä, Sokero, Lestelä-Mielonen and Isometsä2005), while others also found lower reported impairment among those with recurrent MDD (Kruijshaar et al., Reference Kruijshaar, Hoeymans, Bijl, Spijker and Essink-Bot2003; Van Der Werff et al., Reference Van Der Werff, Verboom, Penninx, Nolen and Ormel2010), although this latter finding lost statistical significance after adjustment for depression characteristics, including symptom severity (Van Der Werff et al., Reference Van Der Werff, Verboom, Penninx, Nolen and Ormel2010). Interestingly, we found that a history of depressive distress disorders remained a protective factor for role impairment even after adjustment for MDD characteristics, including severity.
Somewhat surprisingly, a history of depressive disorder was not associated with 12-month suicidal ideation, plan or attempt. This suggests that people with a longer history of depression are not currently at higher risk of suicidal thoughts and behaviours than people with first onset of depression. Nevertheless, it is likely that people with a longer history of depression do have a higher lifetime risk of suicidality as risk increases over the years since persons with (a history of) MDD remain vulnerable for suicidal ideation over time (de Beurs et al., Reference de Beurs, Ten Have, Cuijpers and de Graaf2019).
Lifespan perspective to MDD and other mental disorders
Applying a lifespan perspective to MDD appears to be of importance, since individuals with MDD are highly likely to have suffered from previous MDD and other mental disorders and these disorders predict current, and potentially also future, depression outcomes. Other epidemiological studies have also shown that comorbidity is associated with increased depressive episode duration (ten Have et al., Reference Ten Have, Penninx, Tuithof, van Dorsselaer, Kleinjan, Spijker and de Graaf2017), lower likelihood of MDD remission (Kelly and Mezuk, Reference Kelly and Mezuk2017) and chronicity of MDD (Satyanarayana et al., Reference Satyanarayana, Enns, Cox and Sareen2009; Murphy and Byrne, Reference Murphy and Byrne2012; ten Have et al., Reference Ten Have, de Graaf, van Dorsselaer, Tuithof, Kleinjan and Penninx2018). On the other hand, research findings have not been consistent. For example, Hoertel et al. (Reference Hoertel, Franco, Wall, Oquendo, Kerridge, Limosin and Blanco2015) concluded that patient accounts of previous mental disorders would probably not improve the prediction of future suicidality, because current comorbid mental disorders explained the associations of remitted mental disorders with suicide attempts. Our post-hoc analyses also showed that most of the associations between comorbid mental disorders and outcomes were explained by current, rather than remitted, disorders, but our results contrast with Hoertel et al.'s since we found that both current and remitted externalising disorders were associated with 12-month suicidal thoughts and behaviours. Another study also suggested residual effects of (comorbid) psychopathology, finding that individuals with previous internalising and externalising disorders still reported higher functional impairment even 12 months after remission of the disorder (Bijl and Ravelli, Reference Bijl and Ravelli2000).
Potential benefits of taking a lifespan perspective when examining mental disorders are probably not restricted to MDD. Future studies could examine the role of previous disorders in onset and associated disability of other mental disorders with a relatively late median AOO such as panic disorder, or instead, focus on early-onset disorders as causes or markers of future psychopathology. For example, in another report of the WMH surveys, specific phobia in childhood was predictive of other internalising disorders as well as impairment throughout the life course (de Vries et al., Reference de Vries, Al-Hamzawi, Alonso, Borges, Bruffaerts, Bunting, Caldas-de-Almeida, Cia, De Girolamo, Dinolova, Esan, Florescu, Gureje, Haro, Hu, Karam, Karam, Kawakami, Kiejna, Kovess-Masfety, Lee, Mneimneh, Navarro-Mateu, Piazza, Scott, Ten Have, Torres, Viana, Kessler and de Jonge2019).
Comparison with clinical studies
The results of the current study are in line with clinical studies. Among outpatients with a primary diagnosis of current MDD, 91% had another lifetime mental disorder diagnosis (including previous MDD) (Brown et al., Reference Brown, Campbell, Lehman, Grisham and Mancill2001). Another study in outpatients with MDD also showed high prevalence rates of lifetime and current comorbidity (Zimmerman et al., Reference Zimmerman, Chelminski and McDermut2002; Zimmerman et al., Reference Zimmerman, McGlinchey, Chelminski and Young2008). However, these findings do raise the question of whether these high comorbidity rates represent an artefact of current diagnostic systems, for example, as a result of the increasing number of diagnoses in the DSM (Maj, Reference Maj2005a), while different diagnoses may actually result from a single clinical entity (Maj, Reference Maj2005b). Nevertheless, detecting the presence of comorbid psychiatric symptoms may be very relevant in clinical management (Mai, Reference Maj2005a). Indeed, the importance of taking comorbidity into account was exemplified by Zimmerman et al. (Reference Zimmerman, Chelminski and McDermut2002); their study showed that the majority of patients with primary MDD and comorbidity wanted treatment to also focus on these comorbid current disorders, partially remitted disorders or symptoms not meeting full diagnostic criteria (Zimmerman et al., Reference Zimmerman, Chelminski and McDermut2002). Unfortunately, underrecognition of comorbidity is likely to be common in routine clinical care when unstructured clinical evaluations are used and time is limited (Zimmerman et al., Reference Zimmerman, McGlinchey, Chelminski and Young2008).
The importance of a lifetime approach to MDD in clinical care has been advocated before, for example, by Bockting et al. who argued that knowledge on risk factors of MDD recurrence, such as number of previous MDD episodes, may guide treatment choices (Bockting et al., Reference Bockting, Hollon, Jarrett, Kuyken and Dobson2015). The current study suggests the importance of additionally taking other previous mental disorders into account to further enhance personalised treatment, especially since most associations between previous lifetime comorbid disorders and current MDD outcomes remained statistically significant even after adjustment for MDD characteristics.
Strengths and limitations
An important strength of the current study is the large, cross-national sample, providing the opportunity to examine the associations between MDD and histories of individual mental disorders. Another strength is the comprehensive assessment of multiple depression outcomes and post-hoc analyses that adjusted for MDD characteristics and separated remitted from current comorbid mental disorders. Yet this study also has several limitations. First, disorders were retrospectively assessed, so recall bias may be present, particularly with regard to retrospectively-reported AOO (Johnson et al., Reference Johnson, Gerstein and Rasinski1997). Second, although we distinguished first-onset from non-first-onset MDD episodes, we did not distinguish recurrent from persistent or chronic 12-month episodes. However, post-hoc analyses were adjusted for lifetime presence of chronic MDD. We also did not consider the duration or severity of comorbid disorders, although it is likely that more long-lasting and more severe comorbid disorders are more strongly associated with MDD outcomes. Finally, we did not consider the potential influence of prior treatment for either MDD or comorbid disorders.
Conclusions
In this general population sample, almost all individuals with 12-month MDD had suffered from previous mental disorders. Among these individuals, previous non-depressive distress and fear disorders were particularly strongly associated with greater role impairment, confirming the clinical importance of anxiety in MDD. Previous externalising disorders were most strongly associated with suicidal ideation, plans and attempts. The risks of adverse depression outcomes associated with previous mental disorders were reduced in strength, but did not disappear, after adjustment for MDD characteristics. Risks were mostly conveyed through current, rather than remitted, previous mental disorders, except for the risk of impairment in social life and suicide attempts associated with remitted externalising disorders. These results illustrate the importance of careful psychiatric history taking regarding current anxiety disorders and lifetime externalising disorders in individuals with MDD.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796021000573.
Data
Access to the cross-national World Mental Health (WMH) data is governed by the organisations funding and responsible for survey data collection in each country. These organisations made data available to the WMH consortium through restricted data sharing agreements that do not allow us to release the data to third parties. The exception is that the US data are available for secondary analysis via the Inter-University Consortium for Political and Social Research (ICPSR), http://www.icpsr.umich.edu/icpsrweb/ICPSR/series/00527.
Acknowledgement
The WHO World Mental Health Survey collaborators are Sergio Aguilar-Gaxiola, MD, PhD; Ali Al-Hamzawi, MD; Mohammed Salih Al-Kaisy, MD; Jordi Alonso, MD, PhD; Laura Helena Andrade, MD, PhD; Lukoye Atwoli, MD, PhD; Corina Benjet, PhD; Guilherme Borges, ScD; Evelyn J. Bromet, PhD; Ronny Bruffaerts, PhD; Brendan Bunting, PhD; Jose Miguel Caldas-de-Almeida, MD, PhD; Graça Cardoso, MD, PhD; Somnath Chatterji, MD; Alfredo H. Cia, MD; Louisa Degenhardt, PhD; Koen Demyttenaere, MD, PhD; Silvia Florescu, MD, PhD; Giovanni de Girolamo, MD; Oye Gureje, MD, DSc, FRCPsych; Josep Maria Haro, MD, PhD; Meredith G. Harris, PhD; Hristo Hinkov, MD, PhD; Chi-yi Hu, MD, PhD; Peter de Jonge, PhD; Aimee Nasser Karam, PhD; Elie G. Karam, MD; Norito Kawakami, MD, DMSc; Ronald C. Kessler, PhD; Andrzej Kiejna, MD, PhD; Viviane Kovess-Masfety, MD, PhD; Sing Lee, MB, BS; Jean-Pierre Lepine, MD; John J. McGrath, MD, PhD; Maria Elena Medina-Mora, PhD; Zeina Mneimneh, PhD; Jacek Moskalewicz, PhD; Fernando Navarro-Mateu, MD, PhD; Marina Piazza, MPH, ScD; Jose Posada-Villa, MD; Kate M. Scott, PhD; Tim Slade, PhD; Juan Carlos Stagnaro, MD, PhD; Dan J. Stein, FRCPC, PhD; Margreet ten Have, PhD; Yolanda Torres, MPH, Dra.HC; Maria Carmen Viana, MD, PhD; Daniel V. Vigo, MD, DrPH; Harvey Whiteford, MBBS, PhD; David R. Williams, MPH, PhD; Bogdan Wojtyniak, ScD.
Financial support
The World Health Organization World Mental Health (WMH) Survey Initiative is supported by the United States National Institute of Mental Health (NIMH; R01 MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the United States Public Health Service (R13-MH066849, R01-MH069864 and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical Inc., GlaxoSmithKline, and Bristol-Myers Squibb. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork and consultation on data analysis. None of the funders had any role in the design, analysis, interpretation of results or preparation of this paper. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of the World Health Organization, other sponsoring organisations, agencies or governments. The 2007 Australian National Survey of Mental Health and Wellbeing is funded by the Australian Government Department of Health and Ageing. The Argentina survey – Estudio Argentino de Epidemiología en Salud Mental (EASM) – was supported by a grant from the Argentinian Ministry of Health (Ministerio de Salud de la Nación) – (Grant Number 2002–17270/13−5). The São Paulo Megacity Mental Health Survey is supported by the State of São Paulo Research Foundation (FAPESP) Thematic Project Grant 03/00204-3. The Bulgarian Epidemiological Study of common mental disorders, EPIBUL, is supported by the Ministry of Health and the National Center for Public Health Protection. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection. The Mental Health Study Medellín – Colombia was carried out and supported jointly by the Center for Excellence on Research in Mental Health (CES University) and the Secretary of Health of Medellín. The ESEMeD project is funded by the European Commission (Contracts QLG5-1999-01042; SANCO 2004123, and EAHC 20081308), the Piedmont Region (Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000-158-CE), Generalitat de Catalunya (2017 SGR 452; 2014 SGR 748), Instituto de Salud Carlos III (CIBER CB06/02/0046, RETICS RD06/0011 REM-TAP), and other local agencies and by an unrestricted educational grant from GlaxoSmithKline. Implementation of the Iraq Mental Health Survey (IMHS) and data entry were carried out by the staff of the Iraqi MOH and MOP with direct support from the Iraqi IMHS team with funding from both the Japanese and European Funds through United Nations Development Group Iraq Trust Fund (UNDG ITF). The Israel National Health Survey is funded by the Ministry of Health with support from the Israel National Institute for Health Policy and Health Services Research and the National Insurance Institute of Israel. The World Mental Health Japan (WMHJ) Survey is supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013, H25-SEISHIN-IPPAN-006) from the Japan Ministry of Health, Labour and Welfare. The Lebanese Evaluation of the Burden of Ailments and Needs of the Nation (L.E.B.A.N.O.N.) is supported by the Lebanese Ministry of Public Health, the WHO (Lebanon), National Institute of Health/Fogarty International Center (R03 TW006481-01), anonymous private donations to IDRAAC, Lebanon, and unrestricted grants from, Algorithm, AstraZeneca, Benta, Bella Pharma, Eli Lilly, Glaxo Smith Kline, Lundbeck, Novartis, OmniPharma, Pfizer, Phenicia, Servier, UPO. The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONACyT-G30544- H), with supplemental support from the Pan American Health Organization (PAHO). Te Rau Hinengaro: The New Zealand Mental Health Survey (NZMHS) is supported by the New Zealand Ministry of Health, Alcohol Advisory Council and the Health Research Council. The Nigerian Survey of Mental Health and Wellbeing (NSMHW) is supported by the WHO (Geneva), the WHO (Nigeria) and the Federal Ministry of Health, Abuja, Nigeria. The Northern Ireland Study of Mental Health was funded by the Health & Social Care Research & Development Division of the Public Health Agency. The Peruvian World Mental Health Study was funded by the National Institute of Health of the Ministry of Health of Peru. The Polish project Epidemiology of Mental Health and Access to Care –EZOP Project (PL 0256) was carried out by the Institute of Psychiatry and Neurology in Warsaw in consortium with the Department of Psychiatry – Medical University in Wroclaw and National Institute of Public Health-National Institute of Hygiene in Warsaw and in partnership with Psykiatrist Institut Vinderen–Universitet, Oslo. The project was funded by the European Economic Area Financial Mechanism and the Norwegian Financial Mechanism. EZOP project was co-financed by the Polish Ministry of Health. The Portuguese Mental Health Study was carried out by the Department of Mental Health, Faculty of Medical Sciences, NOVA University of Lisbon, with the collaboration of the Portuguese Catholic University, and was funded by Champalimaud Foundation, Gulbenkian Foundation, Foundation for Science and Technology (FCT) and Ministry of Health. The Romania WMH study projects ‘Policies in Mental Health Area’ and ‘National Study regarding Mental Health and Services Use’ were carried out by the National School of Public Health & Health Services Management (former National Institute for Research & Development in Health), with technical support of Metro Media Transilvania, the National Institute of Statistics-National Centre for Training in Statistics, SC Cheyenne Services SRL, Statistics Netherlands and were funded by the Ministry of Public Health (former Ministry of Health) with supplemental support of Eli Lilly Romania SRL. The South Africa Stress and Health Study (SASH) is supported by the US National Institute of Mental Health (R01-MH059575) and the National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. The Shenzhen Mental Health Survey is supported by the Shenzhen Bureau of Health and the Shenzhen Bureau of Science, Technology, and Information. The Psychiatric Enquiry to General Population in Southeast Spain – Murcia (PEGASUS-Murcia) Project has been financed by the Regional Health Authorities of Murcia (Servicio Murciano de Salud and Consejería de Sanidad y Política Social) and Fundación para la Formación e Investigación Sanitarias (FFIS) of Murcia. The Ukraine Comorbid Mental Disorders during Periods of Social Disruption (CMDPSD) study is funded by the US National Institute of Mental Health (RO1-MH61905). The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708), and the John W. Alden Trust. Dr Dan J. Stein is supported by the Medical Research Council of South Africa (MRC). A complete list of all within-country and cross-national WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.
Conflict of interest
Dr Degenhardt reports grants from Seqirus and Indivior, outside the submitted work. In the past 3 years, Dr Kessler was a consultant for Datastat, Inc., Holmusk, RallyPoint Networks, Inc. and Sage Therapeutics. He has stock options in Mirah, PYM and Roga Sciences. Dr Navarro-Mateu reports non-financial support from Otsuka during 2019 outside the submitted work. Dr Stein has received research grants and/or honoraria from Lundbeck, Johnson & Johnson, Servier, Takeda and Vistagen.






