Introduction
Telemedicine is emerging as a critical component of cancer care worldwide, facilitating access to timely and essential health services regardless of location (Kaye et al., Reference Kaye, Rosen-Zvi and Ron2020; Lloyd and Lee Reference Lloyd and Lee2022; Lopez et al., Reference Lopez, Lam and Thota2021; Naik et al., Reference Naik, Hameed, Nayak, Gera, Nandyal, Shetty, Shah, Ibrahim, Naik, Kamath and Mahdaviamiri2022). By leveraging technologies such as smartphone applications and video conferencing, telemedicine holds great potential to improve treatment quality and health outcomes for cancer patients (Baldwin-Medsker et al., Reference Baldwin-Medsker, Holland and Rodriguez2020; Burton et al., Reference Burton, Valet, Caty, Aboubakar and Reychler2022). Indeed, this technology becomes especially crucial when travel burdens limit access to healthcare, leading to delays in timely screening, diagnosis, and treatment of cancer (Baldwin-Medsker et al., Reference Baldwin-Medsker, Holland and Rodriguez2020). Additionally, for cancer survivors, access to in-person rehabilitation services may be limited or impractical, further complicating their recovery (Børøsund et al., Reference Børøsund, Varsi, Clark, Ehlers, Andrykowski, Sleveland, Bergland and Nes2020; Salifu et al., Reference Salifu, Almack and Caswell2021). This highlights the need to better understand how telemedicine can be effectively used in cancer care across different health systems.
For nearly two decades, oncologists made efforts to integrate telemedicine into standard care to capitalise on its benefits for cancer patients; however, progress remained rather limited (Lloyd and Lee Reference Lloyd and Lee2022). In countries within the World Health Organization (WHO) European Region, telemedicine implementation has faced barriers across multiple domains, including (i) individual challenges such as low digital literacy, resistance to change in clinical practice, and a general preference for in-person care; (ii) organisational issues like poor workflow integration, lack of governance, and financial constraints; (iii) clinical limitations such as insufficient evidence and loss of physical assessment; (iv) economic concerns around funding and unclear benefits of telemedicine; (v) technological hurdles like internet access and interoperability problems; and (vi) ethical concerns related to data security and patient safety (Saigí-Rubió et al., Reference Saigí-Rubió, Borges do Nascimento, Robles, Ivanovska, Katz, Azzopardi-Muscat and Novillo Ortiz2022). Nonetheless, the need to provide health services during the Covid-19 pandemic in a timely manner accelerated the use of telemedicine, not only for Covid-19 patients but also those suffering from non-communicable diseases like cancer (Gottlob et al., Reference Gottlob, Schmitt, Frydensberg, Rosińska, Leclercq and Habimana2025; Haimi Reference Haimi2023; Mehraeen et al., Reference Mehraeen, SeyedAlinaghi, Heydari, Karimi, Mahdavi, Mashoufi, Sarmad, Mirghaderi, Shamsabadi, Qaderi and Mirzapour2023). Although the pandemic served as catalyst for this rapid advancement, a closer examination of telemedicine use among cancer patients is necessary for the sustainability of these services in Europe (Gottlob et al., Reference Gottlob, Schmitt, Frydensberg, Rosińska, Leclercq and Habimana2025; Miziara et al., Reference Miziara, Maesaka, Matsumoto Danielle, Penteado, dos Santos Anacleto, Accorsi, Lima, Cordioli and Salum2021; Paleari et al., Reference Paleari, Malini, Paoli, Scillieri, Bighin, Blobel and Giacomini2022; Qaderi et al., Reference Qaderi, Swartjes, Vromen, Bremers, Custers and De Wilt2021).
The Joint Action ‘Strengthening eHealth including telemedicine and remote monitoring for health care systems for CANcer prevention and care’ (eCAN JA) aimed to make telemedicine accessible to cancer patients across the European Union (EU) Member States, especially those living in remote and rural areas (eCAN JA 2022b). Funded between September 2022 and December 2024, this collaborative effort successfully brought 16 countries together and engaged 35 partners from ministries, national public health institutes, universities, hospitals and cancer centres across the EU (eCAN JA 2022a). With the overarching goal of enhancing quality of life of cancer patients, the key objectives of this JA included (i) advancing telemedicine in cancer care to align with quality standards and user expectations; (ii) improving healthcare professionals’ readiness for telemedicine, especially for patients in geographically underserved regions in Europe; and (iii) promoting the development and integration of interoperable telemedicine solutions into health systems. In the European context, while substantial research has explored telemedicine at the health system level – such as national strategies, reimbursement schemes, and legal frameworks – as well as at the patient level, focusing on individual patient behaviour, acceptance, and digital literacy (Bente et al., Reference Bente, Van Dongen, Verdaasdonk and van Gemert-Pijnen2024; Kidholm et al., Reference Kidholm, Clemensen, Caffery and Smith2017; Raja et al., Reference Raja, Bjerkan, Kymre, Galvin and Uhrenfeldt2021; Raposo Reference Raposo2016; Walley et al., Reference Walley, McCombe, Broughan, O’Shea, Crowley, Quinlan, Wann, Crowley and Cullen2024), a significant gap remains in understanding how these two levels match with each other.
We addressed this gap by exploring the extent to which top-down policies align with bottom-up user needs, thereby applying a systems-thinking approach and highlighting the interconnectedness of actors at two different levels of the health system. Among the eight Work Packages (WPs) of the eCAN JA, the Sustainability WP (WP4) conducted a foresight exercise to gain insights into the EU Member State dynamics and give recommendations for a sustainable and broad implementation of telemedicine services for cancer patients in the EU. We employed a mixed-methods research approach, following an explanatory sequential design (Creswell and Plano Clark Reference Creswell and Plano Clark2018). Our study was thus designed to gather first quantitative and then qualitative insights from decision-makers and cancer patients, through two distinct surveys and a joint workshop, respectively. Ultimately, we aimed to elicit insights from different actors involved in telemedicine implementation, particularly on how regulatory strategies and decisions meet with patients’ needs and uptake. By bringing these policy and patient perspectives together, our study sought to generate integrative knowledge to help bridge the gap between policy intentions and on-the-ground implementation in cancer care in Europe.
Methods
Methodology of the survey for decision-makers
The survey questions for policy decision-makers in the EU Member States were defined based on a literature review conducted between June and August 2023. The review aimed to identify the main contextual factors influencing policy decisions on whether to provide coverage for telemedicine services in routine cancer care in European health systems. The term ‘context’ in the health policy literature is vaguely defined, even though it remains at the heart of policymaking (Barnfield et al., Reference Barnfield, Savolainen and Lounamaa2020; Schmitt et al., Reference Schmitt, Czabanowska and Schröder-Bäck2024; Seward et al., Reference Seward, Hanlon, Hinrichs-Kraples, Lund, Murdoch, Salisbury, Verhey, Shidhaye, Thornicroft, Araya and Sevdalis2021;). To guide our literature review in MEDLINE via Ovid, we used a public policy framework that categorises influential, i.e. contextual, factors in a systematic way (Leichter Reference Leichter1979). Our inclusion criteria and the search query are available in Supplementary Material I, and the detailed analysis of the included studies can be found in Supplementary Material II. Based on the literature review outcomes, the lead author of this study formulated the survey questions. The survey was piloted with two co-authors of this study and one external expert from the Ministry of Health (MoH) of an EU Member State, specialising in the implementation of digital health services. Questions were modified where necessary, and the final version of the survey contained 34 influential factors, to be evaluated based on a 7-point Likert scale.
The survey, designed only for this study and open only to invited experts to fill in, was conducted online via LimeSurvey. Capitalising on the large network of the eCAN JA, we sent the survey to decision-makers through our contacts in the EU Member States and newsletters disseminated in relevant networks. The inclusion criteria for participants were professionals with institutional roles related to digital health technologies and cancer care at the national or regional level, working in governmental or quasi-governmental organisations in the EU Member States. In total, 20 experts from 14 EU Member States participated in this first survey: Austria (1), Belgium (1), Croatia (2), Cyprus (1), Czechia (1), Estonia (1), Greece (1), Italy (3), Lithuania (1), Luxembourg (3), Malta (1), Poland (2), Portugal (1) and Spain (1).
Methodology of the survey for cancer patient associations
Similar to the first one, the survey questions for cancer patient associations were defined based on a literature review conducted between June and August 2023. The review focused on the needs of the cancer patients for telemedicine and was performed in the PubMed database. The inclusion criteria, search query and the detailed analysis of the studies can be found in Supplementary Material III. Based on the literature review outcomes, the lead author of this study formulated the survey questions. The survey was piloted with two other co-authors of this study and one external expert specialising in healthcare innovation from the patient perspective. Questions were modified where necessary, and the final survey for cancer patient associations contained 28 influential factors, to be evaluated based on a 7-point Likert scale.
The survey, designed only for this study and open only to invited experts to fill in, was conducted online via LimeSurvey. We approached cancer patient associations in the countries that participated in the first survey through our contacts in the eCAN JA and professional newsletters. We limited the invitations to associations based in the same countries as the participants of the first survey in order to ensure alignment and comparability between policy and patient perspectives within similar national contexts. Participants were selected from cancer patient associations familiar with the implementation of digital health technologies in the EU Member States and included both professionals specialised in oncological care and individuals with lived experience of cancer. In response, seven experts from five EU Member States and one more expert from an EU umbrella organisation participated in this second survey: Cyprus (1), Greece (1), Malta (1), Poland (2), Portugal (2) and EU-level (1).
Figure 1 provides an overview of the countries responding to the two surveys.

Figure 1. Country distribution of study participants, including health system experts (highlighted in green) and cancer patient associations (indicated with star).
Methodology of the joint foresight workshop
In preparation for the foresight workshop, the survey results and their interpretation were presented to the WP leads of the eCAN JA, including, but not limited to, information technology (IT) professionals, physicians, and stakeholder engagement experts, in a face-to-face meeting in Brussels on 21 February 2024. The discussion contributed to validating the interpretation of the survey findings. Following this meeting, all respondents of the two surveys were invited to an interactive foresight workshop on 29 February 2024 to understand their reasoning about their responses and collect qualitative data about the future of telemedicine implementation in Europe. A summary of the survey results was sent to these experts well in advance, including the scenarios to be presented during the workshop. Experts could, therefore, reflect on the results and consider their responses before the workshop to better prepare for the discussion.
On the workshop day, the participants were asked to comment on four hypothetical future scenarios, which were illustrated in detail by the lead author of this study as the moderator of the discussion. These four scenarios were the following:
-
1. An enabling policy environment and high openness of patients to use telemedicine services
-
2. A discouraging policy environment but high openness of patients to use telemedicine services
-
3. An enabling policy environment but low openness of patients to use telemedicine services
-
4. A discouraging policy environment and low openness of patients to use telemedicine services
To increase both the number and level of detail of expert insights, the same four scenarios were circulated to the survey respondents after the workshop for their written comments as follow-up. Statements emerged from the workshop discussion and written comments were analysed, and policy recommendations of the participants derived from their statements were sent back to them to check the accuracy. The recommendations were revised according to their feedback and the final outcomes were circulated within the group for transparency. Notably, for both surveys and the joint foresight workshop, participants provided informed consent by agreeing that their responses could be securely processed and disseminated for scientific and policy-related purposes. In line with the EU General Data Protection Regulation (GDPR), no personal identifiers – such as names or contact details – were shared with third parties during or after the study.
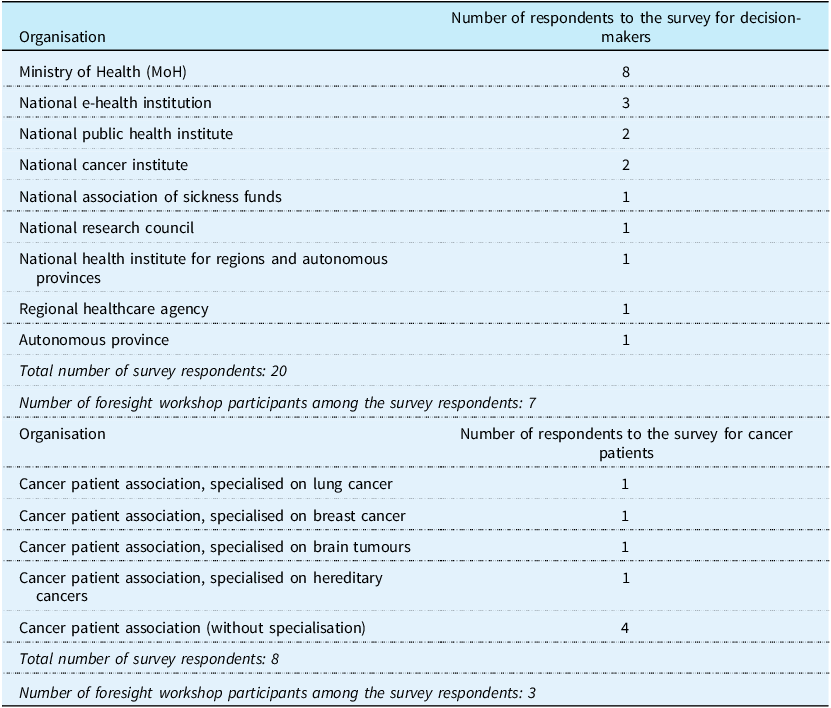
Table 1 provides an overview of the respondents for the two surveys and the joint workshop participants among them.
Table 1. Organisational distribution of respondents across both surveys, with workshop participants indicated among them

Results
Results of the survey for decision-makers
The results of the first survey are shown in Table 2.
Table 2. Results of the first survey, focusing on the health system

Results of the survey for cancer patient associations
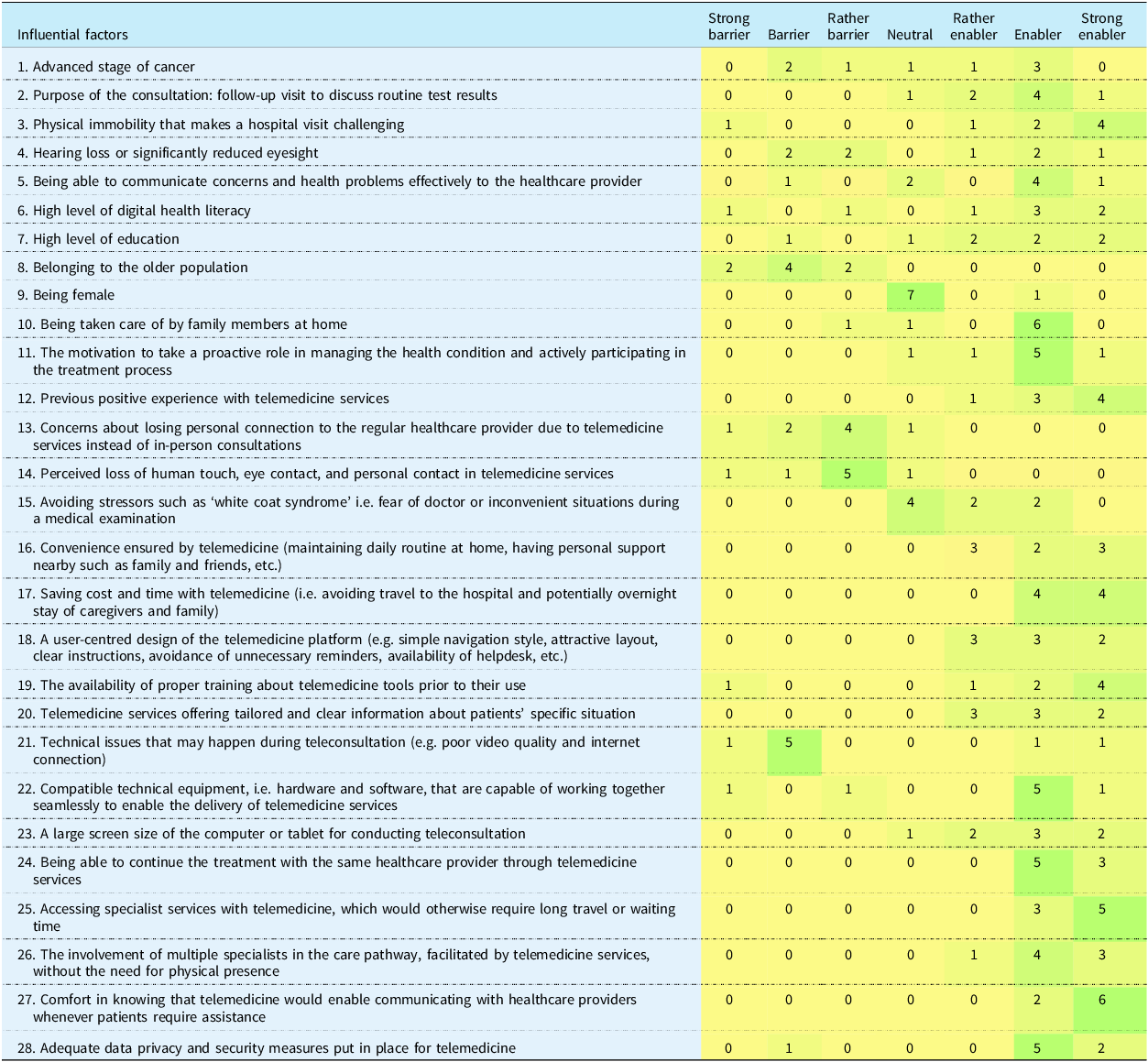
The results of the second survey are shown in Table 3.
Table 3. Results of the second survey, focusing on cancer patients

Results of the joint foresight workshop
Country 1, statements of the health policy expert from the national health institute
The expert expresses a strong belief in the dominance of telemedicine within health and care systems in the long term, specifically in the next 20 years. This optimism is grounded in the expectation that, with time, the necessary policy support and patient openness will align to favour the widespread adoption of telemedicine. In situations where national policies are supportive, there is a clear pathway to leveraging benefits of using telemedicine, provided there is concurrent work on improving patient openness or maintaining it. Conversely, even in a discouraging policy environment, the workshop participant sees regulatory tools of the EU like the European Health Data Space (EHDS) as pivotal in overcoming barriers within countries, suggesting that EHDS can compel them towards the adoption of digital technologies. Lastly, the significant impact of cultural and generational factors on the adoption of telemedicine is acknowledged. Short-term realisation of telemedicine’s potential is seen as constrained by these factors, with a particular emphasis on the need for clear, transparent communication and empowerment of citizens to overcome the implementation barriers.
Country 2, statements of the health policy expert from the national association of sickness funds
According to the expert, there is a strong likelihood of realising an optimistic scenario in the future, where supportive policy environment and high patient openness converge to foster digitalisation in healthcare. This optimism is underpinned by the existing policy support in the country, driven by the potential for more efficient health service delivery through digitalisation. Such efficiency is anticipated not only in financial savings and reducing traditional hospital stays but also in addressing the shortage of healthcare professionals. However, the transition towards digital health services entails significant initial investments in the IT infrastructure. Moreover, continuous innovation and evaluation of digital services are deemed necessary, with an overall trend towards digital openness among citizens, extending far beyond healthcare alone. The country is expected to adopt a hybrid approach rather than full digitalisation of healthcare, considering its relatively small size and the fact that access to healthcare facilities is less of an issue compared to larger countries. Finally, the expert notes that key to the success of telemedicine is physician acceptance; physicians prioritise efficiency and are inclined to support telemedicine if it allows them to dedicate more time to their clinical competencies.
Country 3, statements of the health policy expert from the MoH
According to the expert, the foundation for successful telemedicine integration requires a clear legal framework, transparent reimbursement methodologies and guidelines for all relevant stakeholders. Education and dissemination of information are critical to ensure both healthcare providers and patients are well-informed and capable of using telemedicine services effectively. The expert views the worst-case scenario of discouraging policy environment for telemedicine and low patient openness as less probable in the future, given global trends towards digital health and the increasing body of evidence and technology that favour telemedicine. However, telemedicine’s application should not be generalised across all diseases and treatments, necessitating a case-by-case evaluation to determine its appropriateness and effectiveness. This nuanced approach acknowledges the diverse needs of patients, underscoring the importance of evidence-based decision-making at both the national and hospital levels.
In this context, the expert noted that in their country, the MoH plays a crucial role in overseeing the healthcare system’s broader aspects but does not directly manage projects initiated by individual hospitals. The focus at the ministerial level is on fostering an environment conducive to evidence-based decision-making, particularly in determining the reimbursement and implementation of new treatments in collaboration with insurance companies, following Health Technology Assessment (HTA) processes. Given the complexity arising from the decentralised flow of funds – where financial transactions occur through health insurance rather than directly from the Ministry – the management of digital health practices faces at the national level significant challenges. The MoH, therefore, aims to support these initiatives indirectly by enhancing the digital health literacy of patients and ensuring the adherence to ethical principles in the deployment of digital services. Highlighting good practices within the EU and sharing methodologies for scaling successful models is suggested as a way forward.
Country 4, statements of the health policy expert from the national cancer institute
In the scenario of an enabling policy environment coupled with high patient openness, the expert underscores the necessity of a supportive legislative framework and adequate IT infrastructure. This ideal scenario would moreover require a concerted effort in education and training for both patients and healthcare providers. The emphasis on patient-centricity suggests a reimagining of healthcare to focus on the patients’ needs, alongside a continuous cycle of monitoring, evaluation and improvement of telemedicine services. Dedicated funding and reimbursement modalities are considered essential to sustain the implementation.
In a mixed situation characterised by a discouraging policy environment but high patient openness, the expert sees the need to advocate for policy changes that support telemedicine’s integration into standard care. This could involve collaborations with patient advocacy groups, healthcare providers and policymakers. Similarly, the implementation of pilot projects and partnerships between private and public sectors is suggested to demonstrate the effectiveness and benefits of telemedicine, with community-based initiatives developed to ensure equality in telemedicine services, especially in underserved areas.
For the scenario with an enabling policy environment but low openness among patients, the expert suggests a strategy focusing on educational campaigns to raise awareness about the benefits and safety of telemedicine. Addressing specific concerns by providing clear information about the privacy and security measures for telemedicine is highlighted as crucial. Communication strategies should emphasise telemedicine’s role in complementing traditional care rather than replacing it. Training sessions for patients, especially the elderly, on using telemedicine solutions, and involving patients in the design and testing of telemedicine services are recommended to improve usability and increase openness.
In the most challenging scenario (discouraging policy environment for telemedicine services and low openness among patients) the respondent suggests promoting grassroots initiatives to increase digital health literacy and awareness for telemedicine. Collaborating with non-governmental organisations (NGOs), the private sector, and healthcare professionals to pilot telemedicine solutions could demonstrate the effectiveness of telemedicine and patient satisfaction. Some approaches to promoting policy change include showcasing evidence from successful telemedicine integrations in different countries and securing funding for IT infrastructure and broadband internet in rural areas.
Country 5, statements of the health policy expert from the MoH and a cancer patient association, specialised on breast cancer
According to the expert from the MoH, the journey towards integrating telemedicine into their health system reflects a strategic, albeit gradual, approach. Positioned as neither the primary means of patient-physician interaction nor a standalone solution, telemedicine is envisioned as a complementary tool within the broader national digital health strategy. The expert notes that their country is relatively small and physical access to healthcare facilities is generally not a challenge. Supportive services for patients are readily available outside the governmental framework. Nonetheless, the Covid-19 pandemic was a catalyst for the country to initiate teleconsultations, a practice that has persisted at both the primary care and hospital levels. The introduction of telemedicine services and the recent addition of a live chat feature to the patient portal indicate incremental but purposeful steps towards enhancing digital health. These initiatives signal the MoH’s commitment to leveraging telemedicine technologies to bolster the existing infrastructure, aiming for an optimistic scenario with an integrated digital health ecosystem in the future.
The insights from the Ministry are enriched by the patient perspective. The expert from the cancer patient association states the following: In a scenario where both policy support and patient openness are high, the environment is suitable for piloting innovative telemedicine projects, facilitating feedback and adjustments as necessary. When facing a scenario of discouraging policy environment despite high patient openness, the strategy should involve addressing the underlying causes of this reluctance, gradually incorporating telemedicine by building on existing policies or technologies, and carefully considering the workload of healthcare professionals for adoption. In a scenario characterised by supportive policies but low patient openness, practical hands-on sessions and straightforward communication would be vital to fostering acceptance among patients. The suggestion here involves leveraging family support and organising group educational sessions to bridge the gap, particularly among older demographics, acknowledging a potentially lengthy process of adoption. The most challenging situation arises when both policy support and patient openness are lacking: Overcoming this double hurdle should require starting with small steps, emphasising clear, non-technical language and smooth introduction to telemedicine. Early positive experiences are deemed crucial to gradually building acceptance and trust. A personal home visit for first contact could help those who lag in technology or have difficulty in verbal communication.
Country 6, statements of the health policy expert from the MoH and a cancer patient association, specialised on hereditary cancers
According to the expert from the MoH, the approach to integrating telemedicine is driven by a commitment to place technology directly in the hands of healthcare providers and citizens. As part of digital transition, telemedicine emerges as a pivotal tool, particularly in primary care settings. During implementation, the focus should be on empowering end-users to use telemedicine effectively. In this context, investments in the necessary hardware (e.g. webcams) and software (e.g. telemonitoring apps) should target key infrastructural needs. However, according to the expert, the real challenge lies in integrating this technology seamlessly into the daily workflows of healthcare providers, who often face time constraints that hinder their engagement with digital innovations. Hence, the strategy for the optimistic scenario should consider the organisational aspects in clinical care, enabling them to harness telemedicine without disrupting their care duties.
On the other hand, the expert from the cancer patient association highlights that centralising medical reports and results in a secure, encrypted, and user-friendly platform is a notable issue in their country even within single hospital premises. Addressing the challenge of system non-interoperability, patient-led cancer registries could mark a significant step forward in empowering not only cancer patients but also individuals concerned about their familial cancer risk. Aspiring to integrate with EHDS, a country-level initiative offers a digital platform where users can assess their need for genetic counselling. Coupled with efforts to enhance health literacy through verified information and targeted webinars, this platform aims to overcome barriers in the cancer care continuum and improve patients’ openness to telemedicine.
Country 7, statements of the health policy expert from the MoH
The expert gives importance to collaboration between national and regional units, as well as among ministries with relevant competencies. Such a cooperative approach is deemed crucial in all future scenarios, whether the policy environment is enabling or discouraging, and irrespective of patient openness. The implementation of telemedicine requires an evidence-based evaluation of health outcomes and the establishment of adequate technical infrastructure. While telemedicine is to complement rather than replace traditional face-to-face consultations, it represents an asset in healthcare provision. However, the varying degrees of patient openness to telemedicine, particularly among different demographics, is a key challenge. Suggested strategies include ensuring support for older populations in using telemedicine and maintaining continuity of care by having follow-ups with the same healthcare professional to preserve the personal connection. In the scenario, where both the policy environment and patient openness are discouraging, the respondent suggests that sharing successful practices from other EU Member States and evidence about the benefits of telemedicine could serve as effective strategies for improvement.
Country 8, statements of a cancer patient association
According to the expert, in a scenario with a supportive policy environment and high patient openness, the key to realising telemedicine’s full potential lies in improving digital (health) literacy of patients and healthcare professionals. Special attention should be given to making technology accessible and user-friendly for vulnerable groups, such as the elderly and those with intellectual disabilities. Telemedicine can help enhance patient monitoring; however, the option for in-person visits should be maintained. When patients are ready for using these services but face policy barriers, the initiative to bridge this gap should come from both the patients and the state authorities. Patients should advocate for the adoption of secure digital tools and platforms that protect patient data, encouraging policymakers to recognise and act on the technological readiness and desires of patients. In the scenario where policies support telemedicine, but patient openness is lacking, authorities can incentivise technology adoption by digitising certain services. This transition, complemented by guidance and reassurance about the benefits and ease of digital tools, can gradually increase patient engagement. The most challenging scenario, characterised by both discouraging policy environments and low patient openness, calls for a proactive approach by policymakers to lead the change. Learning from international examples, creating safe and effective digital health policies and actively promoting digital health literacy would be crucial steps. Informational campaigns that highlight the benefits of digital health tools can also help.
Main recommendations of the workshop participants are summarised in Box 1.
Box 1 Recommendations of health policy experts and cancer patient associations to implement telemedicine services in European countries
Health policy experts
-
1. Strategic planning and governance
-
• Leverage telemedicine as a complementary tool in cancer care, not as a replacement for traditional patient-physician interactions
-
• Recognise the suitability of a hybrid model of cancer care over full digitalisation, especially in smaller countries where travel barriers are less pronounced
-
• Develop a clear legal and regulatory framework for telemedicine, including transparent reimbursement mechanisms
-
• Leverage EU regulations like EHDS to overcome policy barriers at the country level
-
• Define clear metrics and evaluation criteria before the implementation of telemedicine solutions in healthcare organisations
-
• Pursue a phased implementation, introducing telemedicine initiatives incrementally while assessing their impact and effectiveness at each stage
-
• Prioritise the integration of telemedicine into the existing systems to maintain physician workflow efficiency and their focus on clinical competencies
-
• Pilot new telemedicine interventions that can be candidates for inclusion into standard care, with the aim to provide evidence-base for future digital health services
-
• Support evidence-based decision-making for the coverage of health services, creating an enabling environment for digital health and the use of data
-
-
2. Equity, ethics and patient-centred design
-
• Develop guidelines that address privacy, data protection and patient rights
-
• Design telemedicine solutions to be user-friendly and accessible to all with a focus on patients’ needs, including those from traditionally hard-to-reach communities
-
• Integrate the concept of health equity into the development and deployment of telemedicine solutions to ensure all patients, regardless of their socioeconomic status, have equal access to quality healthcare services
-
• Adhere to ethical principles for digital health in the implementation and operation of telemedicine services, promote patient-centric approaches
-
• Engage patients in the design and testing of telemedicine services to ensure the solutions meet their preferences
-
-
3. Infrastructure, capacity building and communication
-
• Ensure the development of a solid IT infrastructure that supports telemedicine, including high-speed internet access, secure platforms for handling patient data and compatibility with the existing systems in healthcare organisations
-
• Enhance digital (health) literacy among patients and healthcare providers
-
• Offer specialised training and resources to healthcare providers to facilitate the transition to telemedicine
-
• Establish a collaborative framework that brings together policymakers, healthcare providers, patients, IT experts, and ethics specialists to ensure a comprehensive approach to telemedicine integration
-
• Implement continuous evaluation mechanisms for new digital health services to ensure they meet evolving healthcare needs
-
• Execute targeted public awareness campaigns on the benefits and availability of telemedicine services
-
• Share good practices within the EU to facilitate the scaling of successful telemedicine models in other regions
-
Cancer patient associations
-
1. Patient empowerment and choice
-
• Offer options to patients to choose between telemedicine and in-person visits, acknowledging the value of human contact and personal interaction
-
• Mobilise patient associations to advocate for policy changes that reflect the readiness and desires of the patient community for digital integration
-
• Implement pilot projects to test new ideas and gather feedback for immediate refinement
-
• Draw lessons from other countries to develop policies that safeguard data and promote the benefits of telemedicine, aiming to overcome reluctance and build a conducive environment
-
-
2. Digital health literacy and inclusion
-
• Digitise certain health services as a strategy to familiarise patients with online tools, supported by helpful educational materials
-
• Capitalise on existing practices and technology by introducing new elements step-by-step
-
• Train family members to assist patients in adopting digital health technologies, particularly in demographics showing lower openness to telemedicine
-
• Organise group educational sessions to bridge the gap between patients with varying levels of openness to telemedicine
-
• Improve digital (health) literacy among all healthcare system users, with special provisions for vulnerable groups to ensure accessibility
-
Discussion
Summary of the results
This study examined the main factors that influence the implementation of telemedicine services in cancer care at the policy and patient levels in European countries. Although not representative for the whole EU, by gathering insights from 14 EU Member States and eight cancer patient associations, it provided rich information. To start with, the results of the survey disseminated to health policy experts point towards Covid-19 pandemic, supportive policy commitments and agenda, as well as digital literacy of healthcare professionals as the most facilitating factors for telemedicine implementation (see Q1, Q5, Q6 and Q21 in Table 2). While barriers are seen as less impactful than enablers, the top-rated challenges (i.e. bureaucratic processes, conflicting policy commitments, traditional norms opposing telemedicine, and concerns about patient safety and privacy) should not be overlooked (see Q14, Q16, Q28 and Q32 in Table 2). Similarly, from patients’ perspective, enablers outweigh the barriers. While several factors such as cost and time savings, continuity of treatment, access to specialist services, and faster access to healthcare providers facilitate the use of telemedicine strongly (see Q17, Q24, Q25 and Q27 in Table 3), fewer items are perceived as a strict barrier. These include older age, concerns about losing personal connection with regular healthcare providers, and potential technical issues during teleconsultations (see Q8, Q13 and Q21 in Table 3). Overall, our findings highlight the need to capitalise on enablers such as policy commitments, digital literacy, and patient readiness, while addressing challenges such as infrastructure gaps, workloads of healthcare professionals, and privacy concerns to ensure the effective and equitable integration of telemedicine into European healthcare systems.
Contribution to the literature
Telemedicine has the potential to bridge gaps in cancer care; however, its effective implementation depends on a complex interplay of individual, organisational, and systemic factors. Evidence from the WHO Europe Region and beyond suggests that individual factors, such as patients’ age, satisfaction, and trust, may be as influential as, or even more so than, organisational, clinical, or technological factors in the use of telemedicine (Saigí-Rubió et al., Reference Saigí-Rubió, Borges do Nascimento, Robles, Ivanovska, Katz, Azzopardi-Muscat and Novillo Ortiz2022; Scott Kruse et al., Reference Scott Kruse, Karem, Shifflett, Vegi, Ravi and Brooks2018). In our study, we did not compare the impacts of system-level and patient-level influences with each other. However, establishing a proper regulatory framework and digital infrastructure can be stated as a prerequisite for equitable telemedicine implementation and its possible acceptance by (cancer) patients (Kobeissi and Hickey Reference Kobeissi and Hickey2023; Knudsen et al., Reference Knudsen, Willman and Winn2021; Parimbelli et al., Reference Parimbelli, Bottalico, Losiouk, Tomasi, Santosuosso, Lanzola, Quaglini and Bellazzi2018; Payne et al., Reference Payne, Begovic, Salifu, Nelson, Payne, Downing, Natsiavas and Ling2024; Ricke and Bartelink Reference Ricke and Bartelink2000). The EHDS serves as a promising catalyst in harmonising regulatory frameworks across the EU, fostering the development of a robust digital infrastructure that could facilitate the implementation of telemedicine services (Schmitt et al., Reference Schmitt, Cosgrove, Pajić, Papadopoulos and Gille2023). On the other hand, the availability of regulations or reimbursement of telemedicine in health systems alone does not guarantee the use of these services. According to a recent scoping review, the most notable barrier in this context is the digital literacy of patients (Reinhardt et al., Reference Reinhardt, Schwarz and Harst2021). Indeed, infrastructural investments in rural areas should go hand in hand with training opportunities for patients living there, as well as tailored health campaigns to support the implementation of telemedicine services for cancer patients (Nelson et al., Reference Nelson, Selby, Kane, Harding-Bell, Kenny, McPeake, Cooke, Hogue, Oliver, Gussy and Lawler2024). Ultimately, the success of telemedicine hinges on a holistic strategy that addresses both systemic barriers and individual needs, ensuring no patient is left behind (Leclercq et al., Reference Leclercq, Vandervliet, Schmitt, Van den Bulcke and Delnord2025b).
Strengths and limitations
Our study demonstrates several strengths. The use of a rigorous methodology, including comprehensive literature reviews, well-structured surveys, and a joint foresight workshop, ensured a robust exploration of telemedicine implementation in Europe. By engaging health policy experts and cancer patient associations from several EU Member States, the study could capture a range of expertise from a broad geographical area. The systematic design of the surveys, grounded in a public policy framework, provided a credible foundation for our foresight workshop. Lastly, the iterative feedback process and transparent validation of recommendations after the workshop enhanced the reliability of our results. Overall, this study could provide balanced and forward-looking insights into potential pathways for telemedicine adoption in Europe. However, it also has limitations. The relatively small number of respondents (especially cancer patient associations) may not fully represent the diversity of perspectives across the EU, and the recruitment of experts potentially introduced a selection bias. In addition, the hypothetical scenarios for the foresight workshop, while insightful, may not entirely reflect the complexities of real-world implementation of telemedicine practices. While the study addresses influences of different factors on health systems and cancer patients concerning telemedicine, it does not directly compare their relative impacts on telemedicine implementation, which could be further explored in future studies.
Larger implications
As digital health continues to reshape healthcare delivery, this study offers important insights into how telemedicine can be sustainably integrated into cancer care across Europe. Most notably, our results highlight the willingness of both health policy experts and cancer patients to integrate telemedicine into health systems; however, only as a complementary tool to traditional care, as pointed out by other studies as well (Worster and Swartz Reference Worster and Swartz2017). Another systematic mapping study on telemedicine in cancer care supports this statement by emphasising that the relationship between physician and patient is the most decisive factor when providing telemedicine-based services (Garavand et al., Reference Garavand, Khodaveisi, Aslani, Hosseiniravandi, Shams and Behmanesh2023). Telemedicine can be an impactful tool to support the continuum of care by providing cancer patients the option of receiving health services from their accustomed healthcare provider, or rare specialists, without changing their location. To make this a reality and accelerate the implementation of these services into routine care, studies suggest designing pragmatic trials in countries (Shaffer et al., Reference Shaffer, Turner, Siwik, Gonzalez, Upasani, Glazer, Ferguson, Joshua and Low2023). With its multi-centric trials run across several EU Member States and policy recommendations resulting from the Sustainability WP (WP4), the eCAN JA contributed to advance research and implementation in this promising field (eCAN JA 2022b; Leclercq et al., Reference Leclercq, Saesen, Schmitt, Habimana, Habl, Gottlob, Van den Bulcke and Delnord2025). Country-level efforts should take into account similar international guidance such as the WHO support tool to strengthen telemedicine, which supports stakeholders in assessing ecosystem readiness, defining a strategic vision, identifying necessary organisational changes, determining required resources and skills, and establishing mechanisms for monitoring, evaluation, and optimisation (WHO/Europe 2024).
Conclusion
Conducted as part of the Sustainability WP (WP4) of the eCAN JA (September 2022 – December 2024), this study fills a critical gap in the literature by providing cross-country, stakeholder-informed implementation guidance for telemedicine in oncology. Its findings are directly relevant to EU policy agendas, and offer timely, practice-oriented knowledge for navigating the digital transition in cancer care. Our recommendations for future policies can be summarised as follows: i) develop legal frameworks to complement in-person care with telemedicine; ii) boost digital literacy and IT infrastructure, ensuring privacy and health equity; and iii) engage patients in the co-design of telemedicine services. While the decision-making responsibilities and policy actors involved in telemedicine for cancer care may differ across EU Member States, these recommendations help ensure solutions are responsive to cancer patients’ needs. Implementing them will enhance the integration of telemedicine into European health systems, ultimately improving patient outcomes and satisfaction.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1744133125100273.
Acknowledgements
The authors are grateful to the survey and workshop participants. The authors moreover thank the following researchers from Greece, who kindly supported the literature review for the cancer patient associations survey: Panos Bonotis (Institute of Applied Biosciences, Centre for Research and Technology Hellas), Dr. Petros Sountoulides (3rd Regional Health Authority), Dr. Stergiani Spyrou (3rd Regional Health Authority) and Dr. Pantelis Natsiavas (Institute of Applied Biosciences, Centre for Research and Technology Hellas).
Funding Statement
Open access funding provided by Maastricht University.
Financial support
The Joint Action eCAN was co-funded by the European Union (Grant number: 101075326) under the EU4Health programme between 2022 and 2024. Views and opinions expressed are however those of the authors only and do not necessarily reflect those of the European Union or HaDEA. Neither the European Union nor the granting authority can be held responsible for them.