Introduction
CHD is the most common congenital condition and a global disease. Advancements in healthcare services have significantly improved survival, with over 97% of individuals with CHD now reaching adulthood. Reference Dellborg1 This growing adult CHD (ACHD) population requires ongoing care and lifelong engagement with healthcare services, highlighting the importance of collaborative, patient-clinician partnerships.
Healthcare policymakers increasingly recognise the need for effective, sustainable management of long-term conditions, both from a cost-effectiveness perspective towards improving prognosis and quality of life. Reference Hussain2 ACHD patients like others with chronic conditions often need support in managing their health beyond clinical encounters. In addition to clinical care, self-management support, including medication adherence, lifestyle choices, and emotional coping strategies, is essential. Reference Habibi3
Digital health innovations offer new opportunities to enhance care for this patient population. These tools are increasingly used to empower individuals to track their health, access information, and actively participate in clinical decision-making. One such method involves the use of question prompt lists (QPLs), which have shown benefits in various settings, including oncology. QPLs have been associated with increased information exchange, improved understanding, reduced anxiety, and enhanced patient satisfaction. Reference Roe4
Taking a design-led approach
This idea of a digital tool was part of a collaborative design project to empower ACHD patients to have more ownership of their health. The project used design thinking, which is well regarded as an effective approach for improving healthcare services, leading to better outcomes for patients and clinicians. Reference Oliveira, Zancul and Fleury5 The Double Diamond provides a useful way to visualise a design process, characterised by divergent and convergent thinking, developed by the United Kingdom (UK) Design Council in 2005 (Figure 1). The first diamond emphasises the need to first understand the problem through engagement with patients and clinicians, resulting in a clear problem statement that can be addressed in different ways. The second diamond encourages an iterative approach of co-designing, developing and testing solutions before investing in large-scale implementation.

Figure 1. Adapted from the Double Diamond by the Design Council, licensed under CC BY 4.0.
Aim of the study
Our pilot study aimed to evaluate the feasibility and effectiveness of a CHD-specific digital health tool designed to engage ACHD patients in their care. With the focus on how QPLs could be integrated into consultations to empower patients, enhance shared decision-making, and support clinicians in delivering timely patient-centred care.
Intervention development
Discovery stage
Patient and clinician perspectives on communication barriers were highlighted during the discovery stage:
Quotes from patients
“I didn’t understand the terminology. I still don’t know exactly what is wrong with me.” “When you’re calm you think, ‘oh, I should have asked this.’”
Quote from clinical staff
“If the patient can communicate difficulties and be open and honest, that underpins everything else.”
Definition stage
Through thematic mapping, key themes were identified based on patient engagement and clinic observations. What emerged was the clear need for a new digital tool to connect with the electronic health records (EHRs). Patients expressed scepticism that clinicians would not take the time to review the questions they had submitted unless they were embedded with their current way of working. This outlines the need for any digital tool to integrate with HERs and clinicians’ existing processes, and it cannot be a new system or additional process.
Quotes from ACHD patients
“Will the doctor actually bother to look at it before I go in?”
“Doctors won’t have time to make it that personal.”
Development stage
A theory of change was developed to map out how the intervention of AMA could lead to the desired outcomes, as a basis for pilot planning and evaluation (Figure 2). This proposed that empowering ACHD patients to ask questions and direct the conversation in their consultations would result in more engagement with their health and promote self-management behaviours. This was tested through one of the early pilot studies, a “paper prototyping” study. The goal was to simulate the functionality of a digital QPL without any investment in software development to evaluate the impact on patient knowledge and engagement.

Figure 2. Theory of change (copyright Emily Tulloh).
Methods
Study design
This was a pilot study evaluating the feasibility and utility of a digital QPL for adults with CHD (ACHD).
Participants and recruitment
The study targeted ACHD patients attending outpatient follow-up clinics. Eligibility criteria included adults (≥18 years) with CHD attending clinic who had online access to their electronic medical records and agreed to participate. No additional exclusions were applied based on comorbidities, learning disabilities, or cognitive function.
A patient information sheet was provided, and patients were able to opt in by responding to the QPL digitally. Patients were contacted by phone to ensure completion of the questionnaire and to provide assistance if needed.
During the study period, 172 patients were seen in the clinic. Of these, 110 did not have online access to their medical records. As a result, online questionnaires were sent to 70 eligible patients, and 58 completed responses were received, corresponding to a response rate of 82.9%. Participants ranged in age from 22 to 82 years (mean, 44.9 years). The cohort included 31 men (53.4%) and 27 women (46.6%), representing a balanced gender distribution. Lesion complexity was classified as simple (8 patients, 13.8%), moderate (45 patients, 77.6%), and complex (5 patients, 8.6%).
Development of the question prompt list (QPL)
A specialised QPL was developed for ACHD patients, consisting of fifty-five predetermined questions. The QPL was designed to help patients better understand their heart condition and its long-term effects. The list of questions was created directly from the lived experiences of ACHD patients through focus groups, with additional questions contributed by ACHD clinicians through individual interviews during the development process. Key topics included the impact of ACHD on daily life, mental health concerns such as anxiety and depression, prognosis, treatment options and considerations for ageing with CHD.
Pilot procedure
In the initial paper prototyping stage, conducted across four clinics, paper questionnaires were mailed to patients and shared with their clinicians in advance of consultation. Fifteen patients completed the questionnaire. Two-thirds of patients reported increased knowledge of their health condition, and clinicians reported that four in five patients were more engaged. Although this was a small sample size, it provided sufficient confidence to proceed to a larger pilot study. In the larger digital pilot phase, conducted from July 2024 to February 2025, the QPL was sent digitally to patients two weeks prior to their scheduled clinic appointment. Patients were asked to select up to three questions they wished to discuss during the consultation and were encouraged to add any personalised questions. Completed responses were visible to clinicians in advance of the consultation.
Data collection and analysis
Patient demographics, including age, gender, ethnicity, and lesion classification, were collected to explore potential patterns in question selection. Data gathered through the EHR system was analysed descriptively. Frequency analysis was conducted to assess the most commonly selected questions, while thematic analysis was applied to open-ended responses. Clinician feedback on patient engagement and the relevance of questions was also analysed. Local approval was obtained to recruit patients for this pilot study. A patient information sheet was provided, and completion of the digital QPL was taken as implied consent. Patients were provided with the team’s contact information should they require further details.
Results
Of the 70 patients who were sent questionnaires, 58 completed responses were returned, yielding a response rate of 82.9%.
Delivery stage
Building on the encouraging results from the paper prototyping, we moved to the second stage of the digital pilot phase. In this phase of the study, the QPR was directly integrated into the EPIC system. A total of 58 patients participated between July 2024 and February 2025.
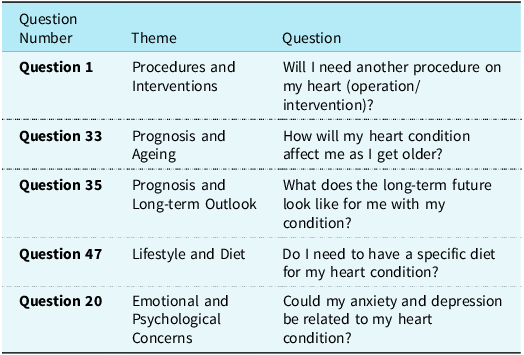
Questions focused on understanding specific symptoms, such as fatigue, and their relation to heart conditions. Patients inquired about the impact of stress and anxiety on their heart condition and sought guidance on managing these emotions and the long-term outcome of their lesion (Table 1).
Table 1. Frequency analysis of selected patient questions using the AMA list

The importance of iterative design and format flexibility
Digital innovation often comes with pressure to build comprehensive systems early, but without iterative testing, solutions may fall short of user needs or clinical feasibility. Engaging with patients early ensures the focus remains on solving the right problem rather than becoming overly invested in specific features or formats.
For example, the AMA tool was originally envisioned as a native mobile app. However, through continuous patient feedback and clinical input, a more accessible web-based format was identified as better suited to both users and healthcare providers. Methods such as user needs mapping and structured problem statements helped ensure development remained aligned with core goals rather than locked into a predetermined solution.
Transdisciplinary collaboration
The development of AMA was the result of close collaboration across disciplines, combining clinical expertise with a design-led approach. This partnership demonstrated the value of integrating diverse perspectives and skill sets throughout the development process.
Clinician leadership was instrumental, providing subject matter expertise in CHD and a deep understanding of hospital systems. Collaboration extended to stakeholders in IT and information governance, ensuring operational alignment. Working alongside a service designer brought a sustained focus on patient experience and introduced key methods such as prototyping, iterative development, and user-centred design.
Design-led practices, including problem framing, co-design focus groups, and low-fidelity prototyping, enabled the team to remain focused on user needs. This transdisciplinary process produced a solution that aligns with clinical workflows in addressing patient priorities and is supported by a strong foundation of user engagement. Reference Woodward6
Integration with electronic system
The integration with the EHR system enabled the responses to be shared with clinicians before consultations. However, challenges arose as some patients were not registered electronically, limiting access to the digital tool. Technical issues also caused delays in questionnaire distribution and the sharing of patient responses.
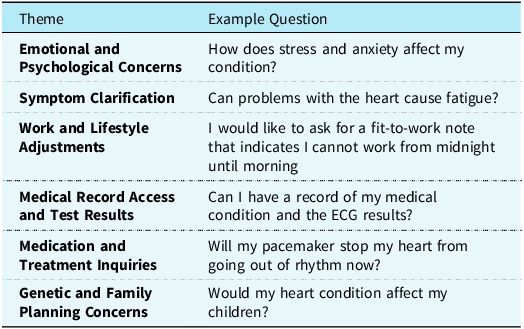
Analysis of open-ended questions
The additional questions provided by patients reflect a wide range of concerns about living with CHD. These questions highlight key areas such as understanding the risks of their condition, exploring future treatments, addressing emotional well-being, managing lifestyle choices, and handling healthcare logistics.
Topics raised included hereditary and family health, symptom management, risk and prognosis, treatment options, psychological impact, lifestyle and physical activity, medication and side effects, and other healthcare-related issues. They also demonstrate patients’ desire to be more informed and actively involved in their care, seeking clarity on how CHD affects various aspects of their lives.
A frequency analysis was conducted to identify the most commonly selected questions from the AMA QPL list during the digital pilot phase. Patients frequently selected questions related to prognosis, ageing, emotional well-being, lifestyle, and potential future interventions. These selections highlight the importance of both clinical and psychosocial topics in ACHD consultations. Table 2 summarises the most frequently selected questions and their associated themes.
Table 2. Analysis of open-ended questions from patients using the AMA list

Patient characteristics and implications for care
Understanding the characteristics of the ACHD population is essential for delivering patient-centred care. The increasing age of ACHD patients highlights the need to address age-related comorbidities alongside congenital conditions. Our study participants were largely representative in terms of gender and case mix of CHD complexity.
Discussion
The need for a digital tool for ACHD patients
The best way to engage patients in their care is to equip them with relevant information about their health, allowing them to ask informed questions during consultations and leading to a shared decision-making process. Reference Nashat7 Furthermore, digital health is rapidly evolving in the healthcare sector, offering new ways to educate patients and empower them to self-manage their care, track and manage their health, and access critical health-related information from their healthcare providers. Reference Abernethy, Adams and Blackford8 In the case of ACHD patients, digital health tools enable them to share baseline information with their local healthcare providers, enhancing care co-ordination and supporting patient empowerment. Reference Nashat7
Previous studies have demonstrated that patients with long-term conditions are often motivated to participate in care planning and co-design initiatives. Reference Coulter9 Adults with CHD require comprehensive care that extends beyond survival, addressing physical, psychological, and social needs throughout their lifespan. Reference Leezer10
Addressing patients and priorities
As the population of CHD patients grows and their need for lifelong care increases, it is essential to develop a tailored health-related quality of life questionnaire that specifically addresses their healthcare needs and management of their long-term condition. Such a tool would not only facilitate personalised care but also provide continuous support in a shared decision-making process, helping patients actively participate in their care. Reference Krist11 This approach is vital for improving outcomes and enhancing the overall patient experience and use of their personal health records. Reference Brands12
These questions reflect the patients’ desire for reassurance and clarity surrounding their health, their long-term prognosis, and the potential need for further medical interventions. Addressing these concerns through effective communication and shared decision-making is crucial in improving patient outcomes and reducing anxiety. Reference Roodbeen13
Despite challenges related to system integration and variable patient engagement, preliminary findings suggest that digital health tools developed through the AMA approach can enhance patient knowledge, promote shared decision-making, and improve the quality of consultations. Our tool facilitated more personalised and focused discussions, helping build stronger partnerships between patients and clinicians. While encouraging patient registration for electronic health record access may expand the reach of digital tools like AMA, additional strategies may be needed to accommodate patients who face barriers to digital engagement. Reference Brands12
However, translating innovative, staff-led ideas into a clinical environment presented several structural challenges. The AMA concept was originally conceived over a decade ago, and its development journey has involved both intensive periods of progress and prolonged delays awaiting approval from various levels of leadership.
Organisational restructuring and turnover in senior personnel introduced uncertainty and new governance pathways, which delayed implementation. Meanwhile, the digital health landscape evolved rapidly, requiring the team to continually reassess the relevance of their approach in light of changing patient expectations and technological standards.
Enduring these barriers required persistence, adaptability, and sustained commitment from the multidisciplinary team. Patience, strong working relationships, and a shared focus on meeting patient needs proved vital in maintaining momentum and adapting a culture of optimism despite setbacks. This pilot study demonstrates the potential of a digital QPL to enhance patient engagement and shared decision-making in ACHD care.
Conclusion
The pilot study demonstrates the potential of digital health tools, such as the AMA approach, to improve patient engagement and shared decision-making in long-term conditions. In this study, the AMA tool was tested in 58 ACHD patients, with a high response rate and consistent patient engagement across both clinical and psychosocial domains. These preliminary findings suggest that such tools can enhance patient involvement and satisfaction with care; however, further research is needed to optimise system integration and evaluate the long-term impact on clinical outcomes in ACHD patients.
Acknowledgements
We thank the patients and clinicians whose contributions and insights were essential to the development of this work.
Financial support
This research received no funding.
Competing interests
The authors declare no conflicts of interest.