This final chapter will examine how someone with OCD can help themselves and seek treatment. Advice will be given on setting up a self-treatment exposure and response prevention (ERP) programme, and resources and organisations which can be helpful in achieving this are discussed. The advice will be given as a step-by-step guide for developing a personal ERP programme to tackle OCD.
This chapter will also examine what to do if an individual is having difficulty accessing help, and it will give useful contacts and organisations as well as written material.
I Have OCD But How Do I Get Help?
This section is geared towards people living in the United Kingdom but may also be applicable to other countries. OCD (and body dysmorphic disorder [BDD]) have official guidance produced by the National Institute for Health and Care Excellence (NICE). This body declares the treatment one should receive within the National Health Service (NHS) and is produced for England and Wales. In Scotland, the Scottish Intercollegiate Guidelines Network (SIGN) adopts and monitors the application of NICE guidance as well as producing some of its own guidance. In Northern Ireland, the body is NICE in Northern Ireland, which adopts and monitors the NICE guidance. The original guidance for OCD came out in 2005 but has been regularly updated. The current guidance is lengthy but can be found at www.nice.org.uk/guidance/cg31/chapter/1-Guidance. It can also be obtained from Her Majesty's Stationery Office as CG31 and is available from the following:
National Institute for Health and Clinical Excellence
MidCity Place
71 High Holborn
London, WC1V 6NA
This guidance states that everyone with OCD should have access to specialised OCD treatment. This includes psychological therapy involving ERP. The intensity of treatment offered depends on the severity of the condition, but it varies from low-intensity therapy (usually ten hours) from local psychological services in primary care to intensive specialised services funded nationally. In addition, the guidance recommends treatment with selective serotonin reuptake inhibitors (SSRIs) or clomipramine and advises that those people who do not respond to these or to ERP should additionally be offered a dopamine blocking agent (as discussed in Chapter 3).
In short, everyone in the United Kingdom should be able to receive appropriate treatment for OCD. The first thing that someone needs to do when seeking help is to visit their general practitioner (GP) and ask to be referred for psychological therapy for OCD or to be prescribed an SSRI. If there is any difficulty with this, it is worthwhile referring to the NICE Guidance CG31 (2005). All GPs should have access to psychological treatment in primary care teams (sometime known as IAPT or Increasing Access for Psychological Therapy). Many of these psychological services will also accept direct referrals from patients themselves. Every region should have such services, but the waiting lists can vary from days to months.
Once referred or receiving an appointment, most people with OCD should be offered ERP. Occasionally, other treatments may be offered if there are complicating diagnoses. For example, people with emotional instability may first need to be seen by a specialised team for treatment of this condition, or people who have experienced extreme trauma may need that addressed first. Sometimes people with OCD are offered anxiety management training. Although this can be helpful for addressing some of the symptoms of anxiety, it is not generally helpful for OCD. If a person is worried you are not receiving the correct help, then you should raise this concern with your therapist.
If the treatment in the primary care service does not help, you should be moved into secondary care services and eventually should be sent to a specialist team that specialises in OCD. Some areas of the country have specialised regional treatment centres for OCD. Unfortunately, these services are not available everywhere. In addition, there is a shortage of therapists specialising in the treatment and management of OCD. However, it is usually possible to find someone locally.
If an individual has not responded to treatment locally and has been offered the treatments mentioned previously, then they may need to be referred to a national treatment centre for OCD. For England and Wales, people who fail to respond to a range of treatments locally can be referred to a highly specialist team for OCD and BDD via the provision of NHS England Highly Specialist Services for OCD and BDD. Details can be found atwww.england.nhs.uk/wp-content/uploads/2013/06/c09-sev-ocd-boy-dysm.pdf and also at www.swlstg-tr.nhs.uk/documents/related-documents/our-services/336-national-service-referral-criteria/file. People with OCD and BDD who live in Scotland, Wales, or Northern Ireland can also be referred to these services via their health department.
What Can I Do to Help Myself?
Some people with OCD may decide to try and tackle the OCD themselves. This may be because they have a mild problem and do not wish to take time from work or other commitments that therapy may entail. Others may have tried therapy before and found that the pace was too fast and they had difficulty complying. Still others may just want to try to overcome the difficulties themselves. Whatever the reason, you should remember that overcoming OCD does involve commitment and bravery and can be difficult to do on your own. Even if you do not wish to seek professional help immediately, it may be worthwhile contacting one of the self-help groups listed later in this chapter.
Next, it is important to remember that you are not ‘going mad’ but have a problem with nasty, anxiety-provoking thoughts, images, or ideas. In order to cope with these thoughts, you have undoubtedly developed a number of strategies to reduce the discomfort caused by the thoughts. These strategies have been fully described in Chapter 3 and include compulsive thoughts or behaviours which reduce the anxiety, such as checking and washing compulsions as well as seeking reassurance from others or taking some precautions and avoiding situations in which the obsessional thoughts are triggered. Unfortunately, these strategies have the effect of fuelling the problem and making the situation worse. Treatment will involve stopping these behaviours and learning to face the fear without these. Some people use alcohol or drugs in an attempt to block out the anxiety. If this is the case, then it is important to first obtain help to overcome these problems before embarking on an exposure programme which is likely to initially increase anxiety levels and therefore may mean that there is a greater tendency to resort to temporary relief from drugs or alcohol.
Before embarking on a self-guided therapy programme or any therapy programme, it is wise to try to be as physically fit and healthy as possible so that you are in the best situation to tackle the programme. This means ensuring that you drink sufficient fluids, eat regular healthy meals, and try to get plenty of sleep and some exercise.
Finally, you should try to discuss options with your GP and read about the treatment options available in general and in your local area.
How Should I Set about Starting Treatment for Myself?
The first thing to do if you want to start working on your OCD is to fully assess the problem yourself. Imagine you had a magic wand and could make all your OCD symptoms go away. What would your life look like? Where would you be living? What job would you be doing? What would your social life look like?
Next, assess what you would need to do to achieve your goals. Would you need to go back to college to gain some qualifications? What would be necessary for you to learn to be more independent, etc. This list may appear daunting, but bear in mind that there is no rush, and every step in the right direction is a step nearer your goal.
It may be helpful to keep a list of your goals nearby to remind yourself of your dreams when treatment is tough. Some people place a reminder of where they are aiming next to their bed or keep it written on a card to look at when they become disheartened.
What Next?
Think about the problems and write them down. These may be similar to the following:
‘Fear of dirt and germs for fear I may become ill and spread the infection to other people’
‘Fear I may contract HIV’
‘Fear I may be a paedophile and may act on this’
‘Fear that unless I perform everything perfectly I will be rejected’
‘Fear that unless I check doors, windows, gas, and electrical appliances, a disaster will occur’
‘Fear that unless I perform tasks in a set way I won't feel “just right” and will be anxious and uncomfortable’
These are just a few of the possibilities. It can be difficult to identify exactly what the fear is, but it is worth spending the time to try to identify it. Many people may have more than one major fear or ‘theme’ of their obsessions. Identifying the fear in this way not only makes it easier to perform the next step in the ERP but also makes the OCD seem more manageable. People with OCD are often overwhelmed by their problems and feel they ‘cannot see the wood for the trees’. By isolating a few ‘themes’ in this way, it can make you realise that the problem is, indeed, containable.
How Do I Develop My Goals of Treatment?
After you have identified the fear(s), consider what task you would be able to do to demonstrate to yourself and others that you have overcome it. For example, for a fear of contamination, the task might be ‘Visit a public toilet, sit on the toilet seat without using disinfectant, use the toilet and leave with a 30-second hand wash’. For fear of paedophilia, it might be ‘Sit in a place full of children without checking’. For fear of disaster occurring in the house, it might be ‘Leave the house without checking’. For perfectionistic fears, it might be ‘Deliberately leave the house without checking my hair and clothes’.
Although this stage is not essential, it can help with devising the hierarchy.
Set out a ‘Ladder’ or ‘Hierarchy’ of Fears
In this step, the stages on the way to facing the fear are identified without performing any anxiety-reducing compulsive rituals or reassurance-seeking. It is important to remember that these tasks need to be performed without the compulsions, and the anxiety needs to be scored in this way. For some compulsions, such as ‘hand washing’, there will still be a ban on the compulsions and a whole ‘new’ way of hand washing will be introduced. Once you have identified the stages in this way, score the anxiety/discomfort you think you will feel whilst engaging in them. A useful scoring system is to score as follows:
0 = no anxiety
2 = mild anxiety
4 = moderate anxiety
6 = severe anxiety
8 = extreme anxiety/cannot be higher/panic
As an example, Table 10.1 presents a hierarchy of someone who has fear of dirt and germs for fear of contracting and spreading an illness.
Table 10.1 Hierarchy for someone who has fear of dirt and germs for fear of contracting and spreading an illness
| Task (to be performed without washing rituals) | Anxiety rating (0–8) |
|---|---|
| Touch door handles in home (apart from toilet handles) | 1 |
| Get dressed without hand washing in between | 2 |
| Touch toilet door handles in home | 3 |
| Touch shop door handles, pedestrian crossing buttons | 4 |
| Bring items home from supermarket without washing outside packaging | 5 |
| Prepare food without first washing hands repeatedly | 6 |
| Touch public toilet door handle | 8 |
| Use public toilet | 8 |
The hierarchy may contain many more items than listed in Table 10.1. It is also important to remember that the exposure tasks should be performed without performing compulsive rituals. With regard to hand washing, clearly everyone needs to wash their hands during the day, but the key here is the extent and way in which this is done. Most people with ‘decontamination rituals’ perform them in set ways. For example, they may always wash in running water and may wash beyond their wrists. The hand wash may take several minutes. In the exposure programme, all hand washing except that before meals or food preparation should be banned. Hand washing should involve putting some water in the basin and then washing to the wrist only for approximately 30 seconds (or the time it takes to sing ‘Happy Birthday to You’ in your head). Programmes should not be performed immediately before preparing meals but, rather, are best performed after eating, and after the hand washing has been performed, to prolong exposure time.
How Should I Perform My Exposure Tasks?
Exposure tasks need to be performed consistently and regularly. You need to start at the bottom of the hierarchy and not jump to higher levels. Stick with one or two items and conquer those before moving on.
The exposure must also be performed regularly, ideally three times a day but at least daily if you are to experience benefit. Record your anxiety during each exposure task (using the same 0–8 scale discussed previously). You will find that initially your anxiety will last for two or three hours, but the more you practice, the shorter the anxiety will last, and the level of anxiety will also decline.
You may find yourself performing compulsive rituals before you realise it. This is normal and natural. If you do perform the compulsions, then go back and re-expose yourself to the fear. With decontamination compulsions, after touching the item it can be useful to touch your body, clothes, and hair and, if possible, lick your hands because this is much more difficult to ‘undo’.
Compulsive thoughts are much more difficult to control. For this reason, it is often best to make a recording of the obsessive fear-provoking thought and listen to this on repeat mode on your mobile phone or similar portable device whilst performing exposure. It is difficult to always ‘undo’ the exposure if the exposure is repeated.
Some people try to ‘jump around’ the hierarchy and suddenly perform a much more difficult item. This is not a good idea. People who do this end up disappointed and disillusioned. Remember that you need to learn to walk before you can run. It takes time, but the gradual approach is best.
Once the items at the bottom of your hierarchy are causing little or no anxiety, it is time to step up to the items causing moderate anxiety. You will probably find that having done the groundwork with easier items, these more difficult items are now easier than you expected and may only cause mild anxiety. Once you have conquered the items causing moderate anxiety, move on to the more difficult items.
At the end when you have performed all the items on the programme, take stock of where you are with respect to the initially stated therapy goals. Think about your life goals and whether now is the time to move forward by taking on a training course or other challenge. Remember that obsessions can expand to fill a vacuum in your life and so keeping busy can be useful in the battle to overcome OCD.
Troubleshooting
Therapy does not always work out as it does in books. There are certain things you need to be aware of.
First, the obsessions will still persist for a long time even after you have faced up to them. The important thing is not to give in to the compulsions. Eventually, over time, the obsessions will fade.
In addition, sometimes as you start to tackle one obsession, another even worse obsession develops. Do not get distracted by this. Remind yourself that, however unpleasant, it is just an obsession, and once you have dealt with the one obsession, you can move on to dealing with the next one. Do not get disheartened – this is all normal and will just take time. Remember, you will overcome the problems in the end.
What If the Anxiety Is Not Coming Down?
Have you exposed yourself for long enough without performing compulsions? Remember it will often take two or three hours before the anxiety comes down. The other issue is whether you have performed the exposure three times a day. Although it does not have to always be three times a day, it must be at least once or twice a day if you are to achieve good results. Three times a day usually leads to the quickest results. Have you been honest about your compulsions? Are you still getting some reassurance or performing other compulsions which will serve to maintain your anxiety? However tempting it can be to engage in compulsions, they really do help maintain anxiety.
If you are sure you have dealt with all the previously mentioned issues, then it may be worthwhile to consider either trying a course of SSRIs or trying some professional help.
Reward and Praise Yourself
Finally, remember that ERP is far from easy. You need to be very brave to face your fears. Once you have truly faced your fears, you need to reward yourself. Take stock and pride in what you have achieved. Remember that true heroes experience anxiety but face it. That is what you have been doing, so you deserve to be kind to yourself. OCD is not a weakness nor a character flaw but, rather, a very real illness, just as any physical illness is not a character flaw or weakness. Praise yourself for what you are doing for yourself, and remind yourself of where you are heading. Do not get disheartened if progress seems slow; it is much better to have a slow but effective programme than a ‘miracle cure’ which collapses within a short time.
Set yourself small rewards after completing your programmes – whatever you enjoy that does not completely break the bank. Maybe a relaxing soak in a bath (assuming you do not have washing compulsions!). Perhaps a walk in the park or a favourite meal? Pamper yourself a little!
Good luck and remember that even people who do not succeed the first time often succeed when they try again. Be kind to yourself, and keep your sense of humour!
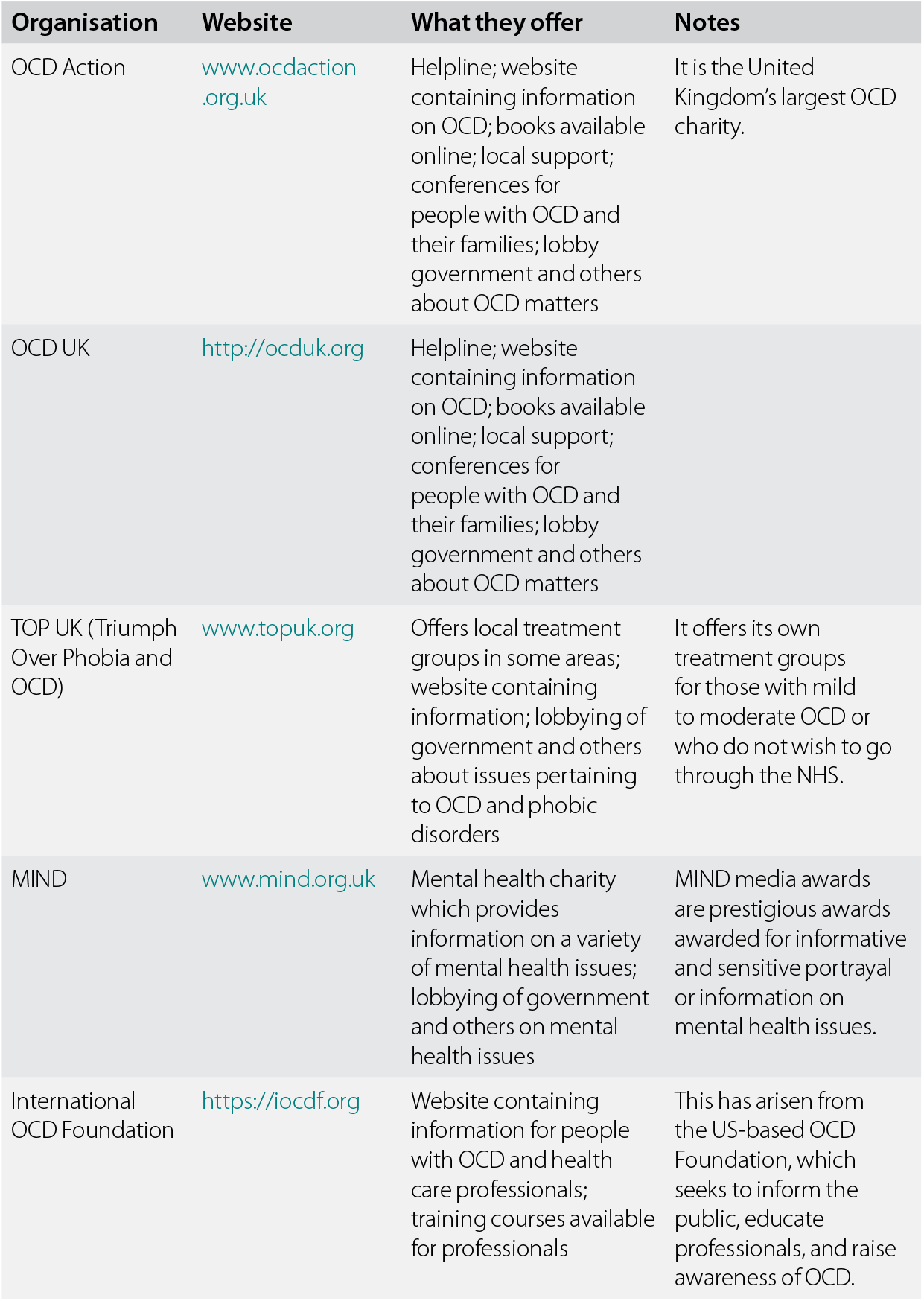
Are There Any Organisations That Offer Help and Support?
There are a variety of self-help and support organisations for people with OCD and their families. Many counties have several organisations; Table 10.2 is geared to the United Kingdom.
Table 10.2 Organisations in the United Kingdom that help people with OCD
| Organisation | Website | What they offer | Notes |
|---|---|---|---|
| OCD Action | www.ocdaction.org.uk | Helpline; website containing information on OCD; books available online; local support; conferences for people with OCD and their families; lobby government and others about OCD matters | It is the United Kingdom's largest OCD charity. |
| OCD UK | http://ocduk.org | Helpline; website containing information on OCD; books available online; local support; conferences for people with OCD and their families; lobby government and others about OCD matters | |
| TOP UK (Triumph Over Phobia and OCD) | www.topuk.org | Offers local treatment groups in some areas; website containing information; lobbying of government and others about issues pertaining to OCD and phobic disorders | It offers its own treatment groups for those with mild to moderate OCD or who do not wish to go through the NHS. |
| MIND | www.mind.org.uk | Mental health charity which provides information on a variety of mental health issues; lobbying of government and others on mental health issues | MIND media awards are prestigious awards awarded for informative and sensitive portrayal or information on mental health issues. |
| International OCD Foundation | https://iocdf.org | Website containing information for people with OCD and health care professionals; training courses available for professionals | This has arisen from the US-based OCD Foundation, which seeks to inform the public, educate professionals, and raise awareness of OCD. |
There are various ways in which you can access therapy. In the United Kingdom, all areas should have access to psychological therapies in primary care.
In the United Kingdom, the National Institute for Care and Health Care Excellence has published guidance on the treatments people with OCD and body dysmorphic disorder should receive. These are published in England but accepted in other areas of the United Kingdom.
Self-help means first identifying and setting out the problem and trying to think of what your life would be like without OCD.
A hierarchy of fears should be constructed of exposure tasks which would cause anxiety when performed without compulsions.
Exposure tasks should start with easier ones which should be performed ideally three times a day.
Initially, anxiety will take two or three hours to subside completely.
Once easier tasks have been achieved with ease, move on to slightly more difficult items.
Do not jump to the most difficult items; take it slow.
Be kind to yourself; ERP is difficult and you need to recognise your achievements. OCD is not evidence of weakness or a character flaw but, rather, a very real illness.
If the treatment does not seem to be working after at least a week of trying exposure to one or two items, think about whether you are performing the tasks often enough, for long enough, and without compulsive rituals.
If, despite performing ERP correctly, you do not improve, it is worthwhile thinking about medication or psychological help.
Reward yourself and take pride in your efforts. ERP is very difficult and you need to be brave to tackle it.
You are not alone, and there are many organisations and self-help groups that can help you.