Introduction
Approximately one in six Americans become ill from foodborne infections each year; Salmonella spp. cause more than 1 million foodborne infections annually in the USA [Reference Scallan1]. Sprouted seeds like alfalfa and clover, and sprouted mung beans have been repeatedly implicated as a cause of enteric disease outbreaks [Reference Backer2–Reference Winthrop7], and outbreaks linked to raw sprouted products, like sprouted, ground and dried chia seeds, are emerging [Reference Harvey8]. Citing food safety concerns, some consumer advocacy groups support warning labels on packaging for sprouted seeds, beans and other sprouted products; some companies refuse to sell sprouts altogether [Reference Leschin-Hoar9]. Despite these concerns, sprouted seeds may have nutritional benefits. The nutritional value of some types of sprouts are well-established; they often contain higher levels of some vitamins, minerals and amino acids than their unsprouted counterparts, though this varies by sprout type [Reference Price10]. Raw nuts [Reference Gould11–Reference Frelka and Harris13] and nut butters are also known sources of foodborne illness and outbreaks [14–Reference Sheth16]. Additionally, an outbreak linked to cashew cheese made with raw nuts was reported in 2014 [17].
On 19 August 2015, the Oregon Public Health Division (OPHD) began investigating two cases of Salmonella Paratyphi B variant L(+) tartrate(+) (Salmonella Paratyphi B dT+, and since this outbreak, referred to as Salmonella I 4, [5], 12:b:-) infection with the same pulsed-field gel electrophoresis (PFGE) pattern. These cases occurred within a 30-day timeframe; a third case was identified on 7 October 2015. On 26 October 2015, Centers for Disease Control and Prevention's (CDC's) PulseNet, the national molecular subtyping laboratory network, identified seven additional Salmonella Paratyphi B dT+ infections with the same PFGE pattern from six additional states. This PFGE pattern was new to the PulseNet database, making it more likely that these illnesses shared a common source. CDC began investigating in coordination with OPHD, and other state and federal partners.
Methods
Case definition and case finding
We defined a case as infection with Salmonella Paratyphi B dT+ PFGE XbaI pattern JKXX01.1538, with illness onset during 1 July–30 November 2015. State public health laboratories determined PFGE patterns of clinical isolates, and uploaded them to PulseNet, where the patterns were confirmed and named.
Hypothesis generation
State and local health officials initially interviewed ill people with state-developed questionnaires or CDC's standard national hypothesis generating questionnaire (NHGQ). In Oregon, ill people were interviewed with an OPHD hypothesis-generating ‘shotgun’ questionnaire. This questionnaire collects data on 884 food and animal exposures during the week before a person became ill, including a variety of health foods, meat, dairy, vegetables, fruits, processed foods, spices, foods eaten raw or intentionally undercooked, and foods eaten outside of the home.
After preliminary common exposures were identified, a single CDC interviewer conducted iterative open-ended interviews with people who became ill more recently. We chose to conduct open-ended interviews because they allowed us to identify whether ill people ate foods that were not on state questionnaires or the NHGQ. We asked about foods the ill person generally avoided or disliked, foods (and brands) they commonly consumed and where they usually purchased food (including grocery stores and restaurants). As more ill people were interviewed, we identified additional foods to include in subsequent interviews to help narrow our hypothesis.
We developed a focused questionnaire by combining suspected foods identified through open-ended interviewing with information collected from the OPHD shotgun interviews and the NHGQ. The focused questionnaire collected detailed information on brand, type, flavour, purchase date and location, best-by dates, lot codes, and whether leftover product was available for microbiological testing.
To evaluate exposures of interest, we compared foods reported among ill people in the 7 days before illness began with 7-day food exposure estimates from two different population-based surveys using a standard binomial probability model. First, we compared the frequencies of foods reported by ill people in this outbreak with the 2006–2007 FoodNet Population Survey, which collected information on foods reported by healthy people during the 7 days before interview [18]. Second, for foods not included in the FoodNet Population Survey, we compared frequencies of foods reported by ill people in this outbreak with those reported by other ill people interviewed using the OPHD shotgun questionnaire database. This dataset includes interview data collected for both sporadic and cluster-associated cases of Salmonella and Shiga toxin-producing E. coli infection since 2007. For this second comparison, we excluded sporadic infection among people that reported international travel in the 7 days before illness onset, infection among people without acute onset of either vomiting or diarrhoea, and infections suspected to be secondary to another person's illness in the same household.
Regulatory investigation
After we identified the suspected food vehicle, the Oregon Department of Agriculture (ODA) made an initial site inspection at the firm on 24 November 2015. ODA then conducted a joint inspection of the firm with the Food and Drug Administration (FDA) Seattle District Office on 1 December 2015. FDA conducted a traceback investigation of select product ingredients. ODA made two additional visits to the firm, on 14 and 22 December 2015, as part of the regulatory response to the product recall.
Laboratory investigation
Leftover, opened products from ill peoples’ homes in California, Hawaii and Oregon were collected for testing by the California Department of Public Health (CDPH) Food and Drug Laboratory Branch, the State Laboratories Division at the Hawaii State Department of Health (HSDH) and Deschutes County Health Services (Oregon), respectively. ODA collected samples of finished product during their initial inspection at the firm. The firm also provided OPHD with open samples of retained, finished product that contained 1 oz. or less of product. Additionally, OPHD purchased unopened finished product from a local store in Oregon. All samples and product ingredient samples collected from the firm and at retail were cultured for Salmonella at a private laboratory for analysis on behalf of OPHD. ODA and FDA Seattle District Office collected environmental samples during the second inspection and during a subsequent follow-up inspection. Environmental samples were collected using sponges and Q-tips, and were cultured for Salmonella by FDA.
Results
Case finding
We identified 13 cases from 10 states: California (one), Colorado (one), Georgia (one), Hawaii (one), Idaho (one), Illinois (one), Maine (one), North Carolina (one), New Jersey (one) and Oregon (four) (Fig. 1). Illness onset dates ranged from 18 July–22 November 2015 (Fig. 2). Ill people ranged in age from 1 to 79 years (median: 41), and five (38%) were female. Of 12 ill people with information, none were hospitalised, and no ill people died.
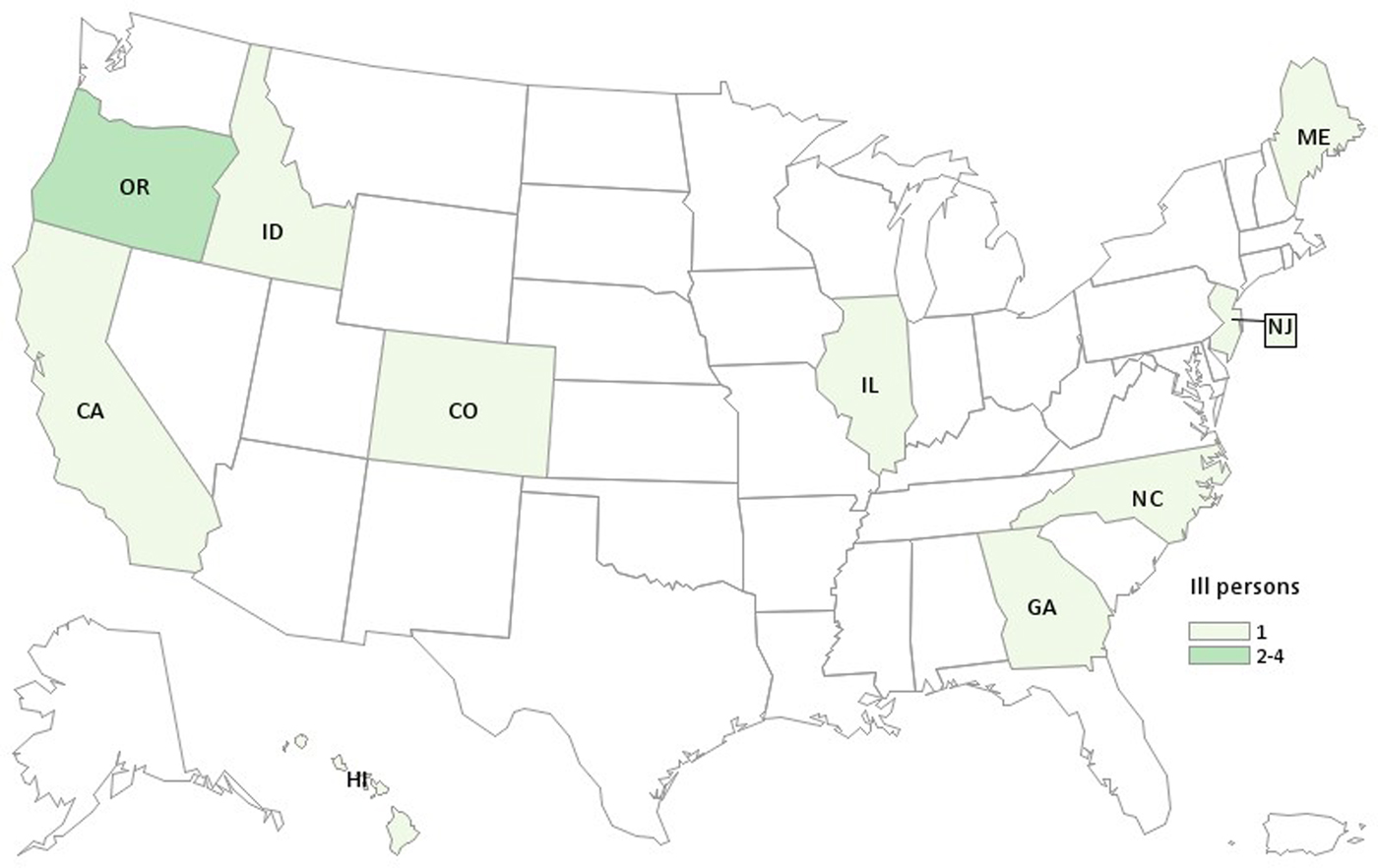
Fig. 1. People infected with the outbreak strain of Salmonella Paratyphi B var. L(+) tartrate (+), by state of residence, 2015 (n = 13).

Fig. 2. People infected with the outbreak strain of Salmonella Paratyphi B var. L(+) tartrate (+), by date of illness onset, 2015 (n = 13).
Hypothesis generation
Information from state questionnaires and the OPHD shotgun questionnaire revealed that several health foods were reported by two or more ill people in this outbreak the week before they became ill: kale (five ill people), almonds (three), seaweed (two) and organic foods (two). Six ill people reported shopping at various health food stores. This ‘healthy eater’ signal suggested that the outbreak vehicle might not be captured on the NHGQ, so we conducted open-ended interviews. We completed four open-ended interviews during 13–23 November. All four ill people reported eating nut butters, and two reported the same product: cacao-flavoured Brand A raw sprouted nut butter (Fig. 3). The remaining two ill people reported eating peanut butter (one ill person) and almond butter (one ill person). Other commonly reported foods were kale (three), nutrition bars (three, same brand), chia seeds (three, two of the same brand) and kombucha (two ill people, same brand). To further investigate Brand A raw sprouted nut butter as a possible outbreak source, we developed a focused questionnaire to specifically ask ill people about this exposure. Brand A raw sprouted nut butter, other nuts butters and the other commonly reported foods above, and specific brands, were included in the focused questionnaire.
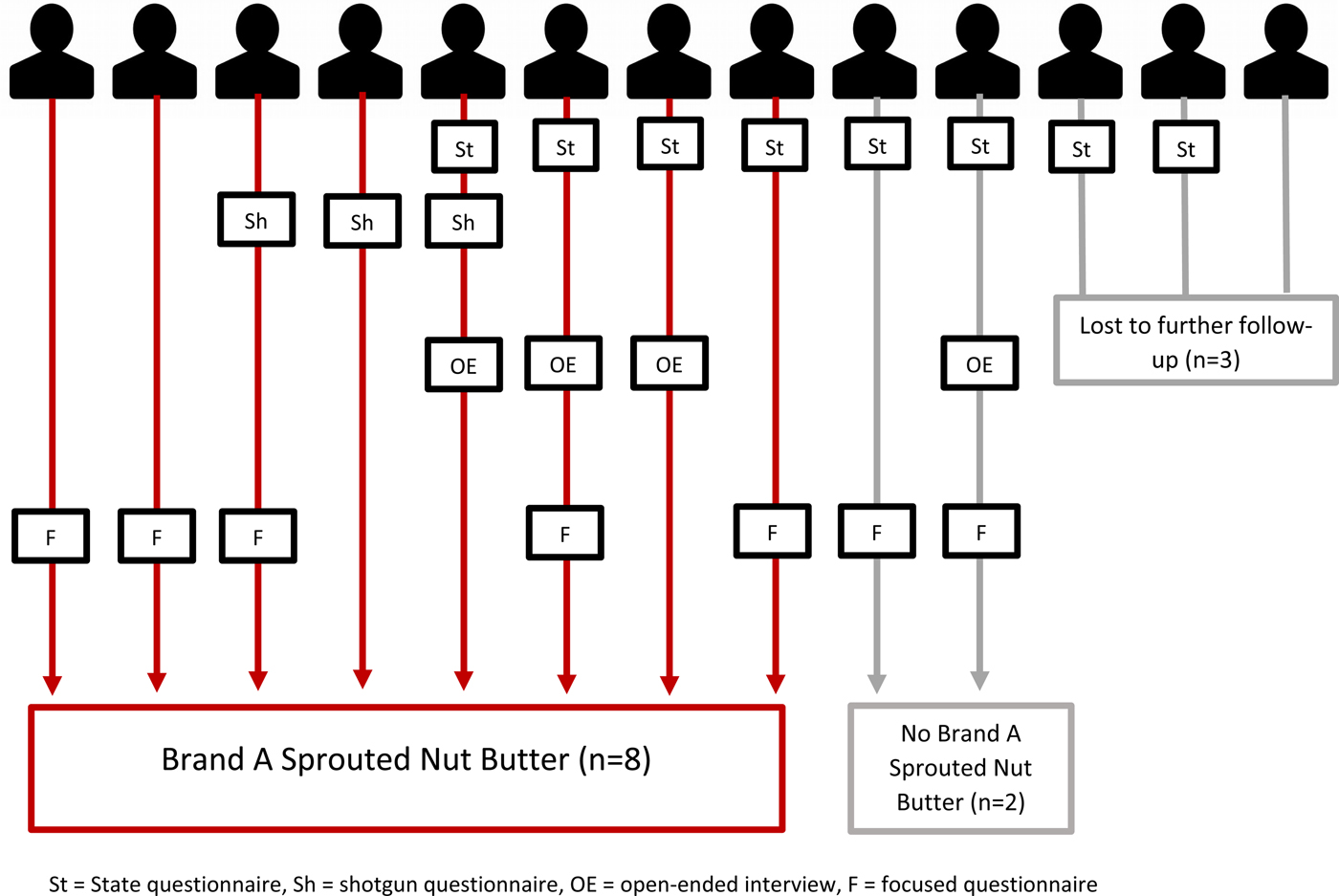
Fig. 3. Hypothesis generation and hypothesis testing questionnaires administered, and Brand A raw sprouted nut butter exposure, by ill person.
Seven ill people were interviewed or re-interviewed with the focused questionnaire, including the two ill people who reported nut butter during open-ended interviews but had not spontaneously reported eating Brand A raw sprouted nut butter (Fig. 3). All seven reported eating nut butters, which was significantly higher when compared with peanut butter consumption from the FoodNet population survey (100% vs. 58%, P = 0.04). We used peanut butter consumption, which likely overestimates consumption of other nut butters, as a proxy since no data were available for other nut butters in the FoodNet Population Survey. However, the OPHD shotgun questionnaire included a question about ‘ground nut butters, pastes or spreads’ other than peanut butter, which would include nut butters made from both roasted and raw nuts; 9.2% of ill people interviewed using the OPHD shotgun questionnaire reported this exposure. We rounded up to 10% for a conservative estimate, and the binomial probability was significant (100% vs. 10%, P ⩽ 0.0005), supporting nut butters as a suspected food vehicle for this outbreak. Of the seven ill people who reported eating nut butters, five (71%) were exposed to Brand A raw sprouted nut butter. Four of the five reported eating Brand A raw sprouted nut butter, including one ill person who did not spontaneously report this brand during an open-ended interview. The fifth ill person was a child who did not eat Brand A raw sprouted nut butter but whose parent did; the child may have been exposed through cross-contamination in the household. Two of five (40%) ill people reported eating chia seeds, two of four (50%) reported nutrition bars (different brands) and none of five reported kombucha.
Identification of the outbreak source
By the end of the investigation, eight of 10 (80%) ill people interviewed with any type of questionnaire were exposed to Brand A raw sprouted nut butters (Fig. 3). Four flavours of Brand A raw sprouted nut butters were available for purchase during this outbreak. Information on flavours consumed was available for seven ill people; six (86%) reported cashew almond butter (four ate only this flavour), three (43%) reported hazelnut cacao butter (one ate only this flavour) and one each reported two different flavours of almond butter. Purchase information was available for five ill people. One ill person ate Brand A raw sprouted nut butter as part of a dish served at a restaurant, one received a sampler pack in the mail, one sampled it at a farmers market, one purchased it from an online store and a health food store and one purchased it only from a health food store. Lot information was available for two Brand A raw sprouted nut butters purchased by ill people; different lots were reported.
Regulatory investigation
A single facility in Oregon produced Brand A raw sprouted nut butters. Nut butters were made by sprouting raw organic cashews, almonds and hazelnuts. The nuts were soaked in water under refrigeration to initiate the sprouting process, then dehydrated and ground. The firm did not apply a kill step to reduce pathogens. All other ingredients, according to the firm, were raw and certified organic; none were sprouted. For the purposes of this outbreak investigation, we defined raw items as those which did not undergo heat or other treatment sufficient to kill pathogens. The firm reported the shelf life of the products was 1 year.
During the initial ODA investigation on 24 November 2015, three critical violations requiring immediate attention were noted: a lack of sanitation of food contact surfaces, unclean food processing equipment and no preventive pest control programme in place. The firm was not actively in production at the time of this visit and agreed to halt further food processing in light of these critical violations and the suspected association of their product with this outbreak.
On 17 December 2015, and after their inspection, FDA issued FDA Form 483, which documented observations of objectionable conditions at the firm, including certain failures to protect against contamination and to take effective measures to exclude pests. FDA's traceback investigation identified the USA, Indonesia and Turkey as the countries of origin of the raw almonds, cashews and hazelnuts, respectively. No investigation of whether other firms that may have received the same lots of these nuts used to make Brand A sprouted nut butter (traceforward) occurred. ODA returned to the production facility at the firm's invitation on 14 December 2015, to review the correction of the violations discovered on 24 November. Although production was supposed to have been halted, inspectors found that the firm had resumed production earlier that morning and that a proper inspection of previously unsanitary equipment could not be conducted. Nut butter produced between 24 November and 14 December (a total of 882 pounds), and all nuts that had already been soaked and dehydrated were placed under embargo by ODA and prevented from being sold over concern of possible Salmonella contamination.
Laboratory investigation
Salmonella was not isolated from any of the three open, leftover samples collected from ill people's homes. Of note, Brand A raw sprouted nut butter collected from the ill person in Hawaii was not the same jar as was consumed before the person became ill. Samples of nut butter ingredients were collected at the firm, and included coconut sugar and dried, sprouted cashews, hazelnuts and almonds. Five samples of raw sprouted nut butters ready for distribution retained from the firm were collected, and included each of the four flavours that were sold at the time, and one flavour that had been discontinued. None of the retained product or product ingredient samples yielded Salmonella. Four unopened retail samples of four flavours of Brand A raw sprouted nut butters also did not yield Salmonella.
Environmental samples collected during the 1 December 2015 visit included samples from processing surfaces, all nut grinders, all dehydrators and screens, bulk ingredient containers, storage shelving and various other equipment throughout the facility. None of these 104 environmental samples yielded Salmonella. Additional environmental samples were collected on 5 December, with an emphasis on areas that might periodically become wet (providing an ideal environment for Salmonella growth); sampled areas included an equipment washing sink, drain pipes, floor sinks and a loose metal support leg beneath a sink used for food processing. Culture of these 96 environmental samples did not yield Salmonella.
Recall and public health impact
On 2 December 2015, the firm announced a voluntary recall of all Brand A raw sprouted nut butters distributed between June and November 2015. CDC and FDA posted outbreak notices and consumer warnings on their websites. The recalled products were distributed nationwide in retail stores, through mail order, and also sold online via the firm's website and online retailers.
Discussion
While sprouts are a known source of foodborne outbreaks [Reference Backer2–Reference Winthrop7], raw sprouted nut butters are a novel outbreak food vehicle. Open-ended interviewing helped identify Brand A raw sprouted nut butter as the likely source of this outbreak of Salmonella Paratyphi B dT+ infections, though the outbreak strain was not cultured from food samples or the production environment. Raw sprouted nut butters are biologically plausible vehicles for Salmonella: contaminated raw nuts, nut butters, sprouted seeds and beans, and sprouted seed products have all caused outbreaks in the past [Reference Backer2–Reference Harvey8, Reference Gould11, Reference Miller12, 14–17, Reference Cavallaro19]. Our findings add to the growing body of evidence that any raw products made using raw sprouted ingredients may carry a risk of foodborne illness similar to that posed by sprouts.
Salmonella was not identified in any Brand A nut butter samples tested, nor from the production environment or nut butter ingredients. Reasons for this may have included transient contamination of the production environment, uneven contamination of raw nuts used to make sprouted nut butter, uneven contamination of lots or inadequate amount of leftover product available for testing. A study examining Salmonella contamination of raw California almonds noted that Salmonella cells were distributed unevenly [Reference Danyluk20]. Another study found Salmonella cells in peanut butter aggregated in clumps around water/lipid suspensions [Reference Podolak21]. Therefore, it is possible that Salmonella bacteria were present in Brand A sprouted nut butter, but not in the samples that were collected and tested.
The ultimate source of contamination of Brand A raw sprouted nut butter remains unknown; we hypothesise that sprouted raw nuts were the most likely source for two reasons. First, raw nuts can become contaminated with bacteria like Salmonella during harvest. Nuts like almonds and walnuts are harvested by shaking them from trees to the ground, where they can become contaminated by grazing animals, wildlife, irrigation water or even poor worker hygiene practices [Reference Frelka and Harris13]. Two studies of raw California almonds sampled at processors before processing found Salmonella prevalence ranging from 0.83% to 1.6%, with estimated most probable number (MPN)s of 1–18.3 per 100 g [Reference Danyluk20, Reference Bansal22]. Another study determined the prevalence of Salmonella in retail samples of raw cashews and macadamia nuts was 0.55% and 4.23%, respectively [Reference Zhang23]. Second, low-level contamination of raw nuts could have been amplified during the sprouting process. We found no data on the microbial safety of sprouted nuts. However, an assessment of Salmonella growth during sprouting of naturally contaminated alfalfa seeds found that an initial Salmonella concentration of <1 MPN/g in the seeds eventually increased to a maximum of 104 MPN/g within 2 days of sprouting [Reference Stewart24]. However, since all ingredients, leftover product and environmental samples that were collected were negative, it cannot be ruled out that another common ingredient, pests, equipment or the environment may have been the source of product contamination.
Producing nut butter that is raw, sprouted and consistently free of Salmonella may be challenging. Roasting and blanching nuts reduces Salmonella bacteria on raw nuts but would result in a product that is not considered raw. Treatment with propylene oxide, another means to reduce Salmonella contamination, would potentially leave the product in what may be considered a raw state, but would result in a non-organic product, which may be important for companies that are interested in producing an organic product. Sprouting carries a risk for bacterial contamination, because the warm, moist and nutrient-rich conditions required to produce sprouts are also ideal for the proliferation of pathogens, such as Salmonella, if present. Because of this risk, FDA recently established sprout-specific production requirements (in 21 CFR Part 112, Subpart M), as part of implementing the FDA Food Safety Modernization Act (FSMA), as well as a Draft Sprout Guidance. These requirements include treatment of seeds or beans used to grow sprouts to reduce microorganisms of public health significance, testing spent sprout irrigation water or sprouts for pathogens, and monitoring the sprout growing, harvesting, packing and holding environments for Listeria or L. monocytogenes. FDA often refers collectively to everything sprouted to produce sprouts for human consumption, simply as ‘seeds’. References to ‘seeds’ in this FDA's Draft Sprout Guidance should not be read to exclude other things that are sprouted to produce sprouts for human consumption. At the time of this outbreak, FDA policy was unclear as to whether sprouted nuts would be regulated under these sprout-specific requirements of Subpart M. As sprouting nuts is an emerging production practice, FDA is evaluating this issue in light of the Produce Safety Rule and Subpart M to determine the best approach in terms of food safety policy. Whether sprouting seeds, beans or nuts, producers should be aware that the sprouting environment and process may amplify even low levels of bacteria present.
Several methods for mitigating the risk of Salmonella contamination after sprouting exist, but they too have limitations. Testing spent irrigation water and/or sprouted nuts for Salmonella, as required by 21 CFR § 112.144(b), is one such measure. However, if every lot of sprouted nuts is not tested, sprouted nuts are tested improperly, or contamination is uneven, contamination may not be detected. A second method, grinding dehydrated sprouted nuts at a temperature high enough to kill pathogens, would result in a non-raw product. Furthermore, the water content of dehydrated nuts might be low enough that Salmonella is not easily destroyed even if high temperatures are applied [Reference Simonsen25]. Finally, the final raw sprouted nut butter product could be heat-treated, but this process might not eliminate Salmonella, especially if the bacterial load is high. The low water activity and high fat content of peanut butter may increase the heat resistance of Salmonella within the product [Reference Stewart24, Reference Shachar and Yaron26]. A study found that some heat-resistant Salmonella strains could survive in peanut butter for the duration of its shelf life, even when exposed to temperatures as high as 194 °F (90 °C) for 50 min [Reference Shachar and Yaron26]. A study assessing in-package thermal inactivation of Salmonella spp., including this outbreak strain, inoculated in Brand A nut butters determined that treatment at >90 °C with a 30 min hold-time achieved a >5 log CFU/g reduction, though there were changes in texture, which the authors noted may make the final product unacceptable [Reference Wright27].
This investigation identified sprouted nut butter as the likely source of a multistate outbreak of Salmonella Paratyphi B variant L(+) tartrate(+) infections, adding to the growing list of outbreaks linked to raw sprouted products. The number and frequency of outbreaks linked to sprouted seeds and raw sprouted products is concerning. Consumers continue to perceive sprouted products as a healthy food with nutritional benefits. However, the risks associated with consuming sprouted seeds in particular are well-documented, and children, the elderly, pregnant women and people with weakened immune systems should avoid eating raw sprouts of any kind [28]. Given this risk, firms that produce foods containing raw sprouted ingredients should consider implementing a kill step to reduce bacterial contamination and subsequent foodborne illness. People at greater risk for foodborne illness should not only avoid eating raw sprouts, but should also consider avoiding eating any products made with raw sprouted ingredients that have not undergone a kill step.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268818002716
Acknowledgements
Tasha Poissant and Paul Cieslak (Oregon Public Health Division, Portland, OR, USA), Matthew Wise, Christine VanTubbergen, CDC's PulseNet Next Generation sequencing laboratory, April McDaniel, and Darlene Wagner (Centers for Disease Control and Prevention, Atlanta, Georgia, USA), State and local health departments.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Disclaimer
The statements expressed in this paper are of the authors and do not necessarily reflect the views of the institution.




