Introduction
As prevalence rates of overweight and obesity have risen, there has been an increasing focus on maternal pre-pregnancy overweight and obesity and excessive gestational weight gain (GWG) in relation both to the effects on women themselves and their children. Reference Poston, Caleyachetty and Cnattingius1,Reference Godfrey, Reynolds and Prescott2 Clinically, there is concern about women entering pregnancy affected by overweight or obesity, not least in relation to the associated risks of gestational diabetes and poor birth outcomes. Reference Poston, Caleyachetty and Cnattingius1 Many cohort studies and trials have assessed pre-pregnancy body composition and GWG and related them to outcomes in women, such as gestational diabetes and weight retention, birth outcomes, and childhood health, body composition, temperament, mental health and educational attainment. Reference Diouf, Charles, Thiebaugeorges, Forhan, Kaminski and Heude3–Reference Robinson, Zubrick and Pennell16 Additionally, influences on GWG itself have been investigated, and interventions conducted to try to reduce it. Reference Holowko, Chaparro and Nilsson17–Reference Bennett, Walker and Blumfield20
In 1990, the Institute of Medicine (IOM) produced guidelines for weight gain during pregnancy, 21 with the recommended amount of weight gain varying according to pre-pregnancy body mass index (BMI). These guidelines were revised in 2009 Reference Rasmussen and Yaktine22 and are used widely in clinical practice and research for categorising GWG as inadequate, adequate or excessive. The 1990 guidelines included guidance on assessment of GWG and recommended that pre-pregnancy weight is best determined from a weight measured at a recent preconceptional visit and that self-reported pre-pregnancy weights must be evaluated for plausibility and discarded if they are suspect. In the 2009 revision, it was noted that a pre-pregnancy measure was the ideal but that, practically, pre-pregnancy weight should be recalled at the first prenatal visit using a standardised question. In reality, a measured pre-pregnancy weight is rarely available and, furthermore, a measured weight obtained too long before conception may differ from the woman’s actual weight in the periconceptional period. Clinically, most women are not weighed until already pregnant, and most research studies recruit participants during pregnancy or after the child’s birth. Generally, pre-pregnant weight is obtained by recall. More recently, GWG charts have been produced using data on more than 200,000 women in 33 cohorts from Europe, North America and Oceania, but for almost all the women, pre-pregnancy weight was self-reported during or after pregnancy. Reference Santos, Eekhout and Voerman23
To date, the focus on estimation of pre-pregnancy weight has been on the accuracy of recalled weight. Reference Headen, Cohen, Mujahid and Abrams24–Reference Mandujano, Huston-Presley, Waters and Catalano26 There is little information on whether an early pregnancy weight, before major pregnancy weight changes have taken place, might be as accurate as, or better than, a recalled measure. Gillmore and Redman Reference Gilmore and Redman27 reviewed alternative methods but did not find any that they could recommend. However, they only identified one study of the use of early pregnancy weight as an estimate of pre-pregnancy weight on which to base their assessment. Reference Butte, Wong, Treuth, Ellis and O’Brian Smith28
Recently, Thomas et al. Reference Thomas, Oken and Rifas-Shiman29 used data from Project Viva and other studies to estimate pre-pregnancy weight. Their method was developed using measures of pre-pregnant weight that had been recorded in clinical records in the 3 months before conception.
To our knowledge, no studies have compared proxy measures of preconception weight based on recalled or early pregnancy weight with a gold standard pre-pregnancy measurement made according to research standards in the general population, rather than in those seeking healthcare before conception. Thus, our aim was to compare actual measured weights taken in the 3 months before conception with three proxy assessments as follows:
-
Recalled weight reported by the women at around 11 weeks’ gestation;
-
Weight measured at around 11 weeks’ gestation;
-
The Thomas method described above. Reference Thomas, Oken and Rifas-Shiman29
We also aimed to compare the recalled, early pregnancy and Thomas weights in a larger group of women and assess how the allocation of the women to pre-pregnancy BMI groups and to IOM GWG categories differed when the three pre-pregnancy weight proxy estimates were used.
Methods
Participants and measurements
We conducted a validation study of different methods of assessing pre-pregnancy weight using data from the Southampton Women’s Survey (SWS) prospective cohort study. A detailed description of the SWS has been reported previously. Reference Inskip, Godfrey and Robinson30 Briefly, between 1998 and 2002, 12,583 women aged 20–34 years from the general population who were not pregnant were recruited through general practitioners in Southampton, UK, and the surrounding area. They were interviewed in their homes, where their weights were measured to the nearest 0.1 kg using portable digital scales (Seca, Germany), which were regularly calibrated. Height to the nearest 0.1 cm was measured with a portable stadiometer (Harpenden, CMS Weighing Equipment Ltd, London), with the woman’s head in the Frankfort plane. Women who subsequently became pregnant were invited to visit the SWS Ultrasound Unit at the Princess Anne Hospital in Southampton at around 11, 19 and 34 weeks’ gestation. In total, 3158 women participated in the pregnancy follow-up phase of the study and delivered a live-born singleton baby. At the early pregnancy visit (around 11 weeks’ gestation), the women were again weighed on digital scales, calibrated using the same procedure as the scales used in the initial pre-pregnancy interviews. The women were also asked ‘How much did you weigh 3–4 months ago, i.e. before you became pregnant?’ Height was not re-measured during pregnancy. Gestational age at birth was determined using a detailed algorithm combining last menstrual period date and early ultrasound data. Estimated date of conception was derived from the date of delivery minus gestational age at delivery plus 14 days.
Fig. 1 shows how SWS women were selected for particular comparisons. The main analysis (see left-hand side of Fig. 1) was based on women whose estimated date of conception was within 3 months of the initial recruitment interview, as this is traditionally considered to be the pregnancy-planning period. Reference Stephenson, Heslehurst and Hall31 Among these women, we used the weight as measured at the recruitment interview as the ‘gold standard’. We considered three estimates of this measure, namely the pre-pregnancy weight recalled by each woman, the weight measured in early pregnancy and a pre-pregnancy weight estimated according to the formula of Thomas et al.: Reference Thomas, Oken and Rifas-Shiman29
where y = pre-pregnancy weight (kg)
-
• x 1 = first trimester measured weight (kg)
-
• x 2 = gestational age (d) at first weight measurement
-
• x 3 = height (cm)
-
• x 4 = maternal age (years)
-
• x 5 = parity

Fig. 1. Flow chart showing classification of Southampton Women’s Survey participants into the analysis groups.
A sensitivity analysis was conducted in which we focused solely on the subset of women who had conceived within 1 month of the initial interview. The aim was to assess whether the findings from the full 3-month period were influenced by those who had taken longer to conceive and who might have been more likely to change their weight between interview and conception.
As many studies recruit participants at the end of the first trimester of pregnancy or later, an additional analysis considered only the women whose early pregnancy visit had occurred at or after 12 weeks’ gestation in order to assess whether the accuracy of measured early pregnancy weight as a proxy for pre-pregnancy weight was dependent on gestational age at the early pregnancy visit.
In research, both recalled weights and early pregnancy measures have been used as proxies for pre-pregnancy weights, but these have rarely been compared. We used the cohort of all SWS women who became pregnant and had both an early and late pregnancy weight measure and a recalled weight (see right-hand side of Fig. 1), to compare the three proxy weight measures with each other and then to compare the resulting allocations of the women into pre-pregnancy BMI and GWG categories.
All phases of the SWS were approved by Southampton and South West Hampshire Local Research Ethics Committee, and written consent was obtained from all participants.
Statistical methods for the comparison of estimates with the measured pre-pregnancy weight
The measured weight before pregnancy was regarded as the gold standard measurement of pre-pregnancy weight. The three proxy weights, namely the recalled pre-pregnancy weight, the measured early pregnancy weight and the estimated weight using the Thomas method, were each compared with the gold standard measurement. The assessment of differences was performed using the methods described by Bland and Altman, Reference Bland and Altman32 with the results being presented as plots of the differences between the two measurements against their mean, the limits of agreement and 95% confidence intervals (95% CIs) around those limits. Further analyses examined the trend in differences in relation to the mean of the measurements, to assess whether the differences varied by pre-pregnancy weight. The trend was assessed by regressing the differences on their average. Analyses were performed using Stata 14.0 (StataCorp).
Statistical methods for the comparison of pre-pregnancy weight estimates in the full SWS cohort
For the full cohort of SWS women who became pregnant, we used the three proxy measures: recalled weight, early pregnancy measured weight and the Thomas estimate. We took account of the mean over- or under-estimation identified in the work on the small cohort of women who conceived within 3 months. Thus, we added or subtracted the mean difference between these weight estimates and the ‘gold standard’ pre-pregnancy weight. We compared these adjusted weights with each other and used them to derive the estimated pre-pregnancy BMI category (underweight (BMI < 18.5 kg/m2), normal (BMI between 18.5 and 25 kg/m2), overweight (BMI between 25 and 30 kg/m2) or obesity (BMI ≥ 30 kg/m2)) for each woman.
Using the weight measurement made in the SWS at around 34 weeks’ gestation, we derived estimated weight gain from before pregnancy to this gestational age, and, using the IOM classification, 21,Reference Rasmussen and Yaktine22 classified the women into the three weight gain categories of ‘inadequate’, ‘adequate’ and ‘excessive’. The resulting categories of BMI and GWG derived using the three proxy measures of pre-pregnancy weight were then compared.
Results
Among the participants in the SWS pregnancy follow-up study, 2028 had measures of pre-pregnancy measured weight (the ‘gold standard’), pre-pregnancy weight recalled in early pregnancy and measured weight at the early pregnancy visit at around 11 weeks’ gestation. Among these women, 198 had an estimated date of conception within 3 months of their recruitment interview, and these women form the sample for the first part of this analysis (see Fig. 1). Details of the included women are given in Table 1 along with those of the other 1830 SWS participants who became pregnant and had all 3 recorded measurements but had an estimated date of conception more than 3 months after their recruitment interview.
Table 1. Characteristics of 198 Southampton Women’s Survey participants who conceived within 3 months of the pre-pregnancy interview compared with 1830 participants who conceived later

The 198 included participants were on average slightly older and more likely to be of non-White ethnicity and multiparous than the other SWS women. There were no important differences in educational attainment or in the anthropometric measurements between the two groups. The 198 participants had a wide range of pre-pregnancy weights (40–119 kg), and the BMI range was 16.4–43.6 kg/m2, with 6 (3%) women being affected by underweight (BMI < 18.5 kg/m2), 43 (22%) by overweight (BMI between 25 and 30 kg/m2) and a further 37 (19%) by obesity, (BMI greater than 30 kg/m2). In terms of BMI categories, the included participants were more likely to be affected by obesity than those not included but less likely to be affected by overweight. The early pregnancy interview was targeted to take place at around 11 weeks’ gestation, and the actual gestational ages at this visit were similar for the 198 included participants and the remainder of the other SWS participants.
Comparison of proxy and gold standard measures
The Bland–Altman plots comparing each of the three proxy estimates of pre-pregnancy weight with the pre-pregnancy measured weight (the gold standard) are shown in Fig. 2. The mean differences are shown by the solid horizontal line, and details are given in Table 2.

Fig. 2. Bland–Altman plots comparing each proxy measure with the actual pre-pregnancy weight. (a) Recalled pre-pregnancy weight, (b) early pregnancy measured weight and (c) Thomas method weight. Solid line = mean difference, dotted lines = limits of agreement, shaded area = 95% CIs around the limits of agreement and dashed line = fitted regression line.
Table 2. Comparison of differences between ‘proxy’ weights and the pre-pregnancy measured weight (n = 198)
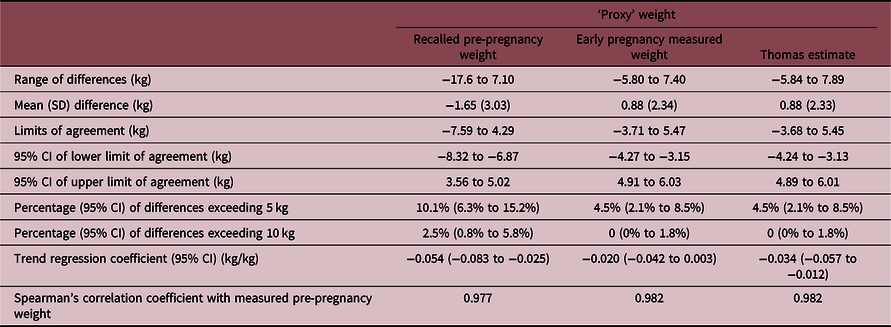
The recalled weights tended to underestimate the pre-pregnancy measured weights by a mean (standard deviation (SD)) difference of 1.65 (3.03) kg (Fig. 2a). In contrast, both the early pregnancy measured weights and the Thomas method weights overestimated the pre-pregnancy measurements by means (SDs) of 0.88 (2.34) kg and 0.88 (2.33) kg, respectively (Fig. 2b, 2c). The limits of agreement were wider apart for the recalled weights (a width of 11.88 kg) than for the early pregnancy measured weights (9.18 kg width) and the Thomas weights (9.13 kg width), as can be seen in Fig. 2 and Table 2. Notably, 10.1% of the recalled weights differed by more than 5 kg from the gold standard measured pre-pregnancy weights, and 2.5% differed by more than 10 kg. The corresponding percentages for the differences between the gold standard weights and both the early pregnancy weights and the Thomas weights and were 4.5% and 0%.
The dotted lines in Fig. 2 show the trend lines for the differences between the measures regressed on their average, and Table 2 gives the regression coefficients. In Fig. 2a, which presents the comparison of the recalled weight with the gold standard measured pre-pregnancy weight, the trend is negative, with the regression coefficient being −0.054 kg (95% CI: −0.083 to −0.025) for each kilogram increase in the average measurement. Thus, women who were heavier tended to underestimate their pre-pregnancy weight more than those who were lighter. The mean difference between the recalled and measured weight in the 118 women with a pre-pregnancy BMI < 25 kg/m2 was −1.18 (95% CI: −1.59 to −0.78) kg compared with the 80 women with a BMI ≥ 25 kg/m2 for whom the difference was −2.35 (95% CI: −3.21 to −1.49) kg (P-value for difference 0.008). In Fig. 2b, which shows the comparison between the early pregnancy measured weights and the gold standard pre-pregnancy measured weights, the trend is less apparent with a regression coefficient of −0.020 kg (95% CI: −0.042 to 0.003) per kg increase in the average measurement. This suggests that women who were lighter tended to put on marginally more weight in the first trimester of pregnancy than women who were heavier. Indeed, the mean increase in weight from before to early pregnancy in women with a pre-pregnancy BMI < 25 kg/m2 was 1.11 (95% CI: 0.72 –1.49) kg compared with an increase of 0.55 (95% CI: −0.03 to 1.13) kg in women with a BMI ≥ 25 kg/m2 (P-value for difference 0.10). Finally, Fig. 2c presents the comparison of the Thomas estimates and the pre-pregnancy measured weights. The mean difference (0.88 kg) and the limits of agreement (−3.68 to 5.45 kg) are remarkably similar to those for the comparison of the early pregnancy weights with the measured pre-pregnancy weights (mean 0.88 kg, limits of agreement: −3.71 to 5.47 kg). However, the regression line has a slightly steeper negative slope, indicating a greater tendency for the Thomas method to overestimate the weights of women who were lighter and underestimate them for those who were heavier. The mean increase in weight from before to early pregnancy in women with a pre-pregnancy BMI < 25 kg/m2 was 1.20 (95% CI: 0.83–1.59) kg compared with an increase of only 0.40 (95% CI: −0.183 to 0.98) kg in women with a BMI ≥ 25 kg/m2 (P-value for difference 0.02).
Focusing on the 74 women whose early pregnancy visit took place at 12 weeks’ gestation or later (median 12.7 weeks, interquartile range 12.1–13.1 weeks) revealed similar results to those in the entire sample. The recalled weight underestimated the actual measured weight by a mean of 1.40 kg, slightly less than the underestimation in the full study sample (1.65 kg). The early pregnancy measured weight and the Thomas method overestimated the actual measured weight by mean of 1.10 and 1.05 kg, slightly more than the average using both methods for all women in the full sample (0.88 kg).
In our full analysis sample, 61 women had conceived within 1 month of the initial interview. Repetition of the analyses on this subsample gave similar findings to those for the full sample of 198 women; compared with the full sample, the width of the limits of agreement increased slightly for the recalled weights from 11.88 to 12.42 kg but reduced slightly for both the proxy early pregnancy measured weights (from 9.18 to 8.07 kg) and the Thomas method (from 9.13 to 7.85 kg).
Comparison of weight estimates in the full SWS cohort
Some 1877 women had all the necessary measures to be able to compare the proxy measures (Fig. 1), though, for 6 women, missing data on some of the variables required for the Thomas method meant that it could not be calculated. Given that the early pregnancy weights and Thomas weights tend to overestimate the pre-pregnancy weights while the recalled weights tend to be an underestimate, we adjusted each measure by its mean difference from the true pre-pregnancy measured weights obtaining the Bland–Altman analyses above. Thus, we subtracted 0.88 kg from the early pregnancy measured weights and the Thomas weights and added 1.65 kg to the recalled weights. The Bland–Altman plot comparing each pair of adjusted proxy pre-pregnancy weight measures is shown in Fig. 3 and reveals considerable differences between the recalled weights and the two other proxy estimates. The limits of agreement were wide, being 13.3 and 13.2 kg apart, respectively, for the comparisons between the recalled weights and each of the early pregnancy measured and Thomas weights. In contrast, the limits of agreement for the comparison of early pregnancy measured weights and Thomas weights were much narrower, being only 1.18 kg. The adjusted weights differed by more than 10 kg for 17 (0.9%) women between the early pregnancy measured and recalled weights, for 15 (0.8%) women between the Thomas and recalled weights, and for no women between the early pregnancy measured weights and the Thomas weights.

Fig. 3. Bland–Altman plots comparing the pairs of adjusted proxy measures with each other. (a) Adjusted recalled pre-pregnancy weight and adjusted early pregnancy weight measurement. (b) Adjusted recalled pre-pregnancy weight and adjusted Thomas method weight. (c) Adjusted early pregnancy weight and adjusted Thomas method weight. Solid line = mean difference, dotted lines = limits of agreement, shaded area = 95% CIs around the limits of agreement and dashed line = fitted regression line. Adjustments: recalled pre-pregnancy weight + 1.65 kg, early pregnancy weight – 0.88 kg, and Thomas weight – 0.88 kg.
Comparison of pre-pregnancy BMI group allocation and GWG using the two estimated pre-pregnancy weight measures
Using the adjusted proxy measures described above, for each woman, we derived her estimated pre-pregnancy BMI group and GWG category using IOM guidelines. 21,Reference Rasmussen and Yaktine22 The comparisons between the three methods for pre-pregnancy BMI are given in Table 3. In the comparisons between the recalled weight and the two other proxy measures shown in Table 3a and b, 87% of women were categorised to the same BMI group, with the remaining 13% being allocated to different but neighbouring categories; two women were allocated to groups that were two categories apart (normal weight and obesity). Table 3c shows the comparison of the early pregnancy weight and the Thomas method, and 99% of women were allocated to the same category by both methods.
Table 3. Numbers of women falling within different BMI categories when different adjusted estimates of pre-pregnancy weight were used

a Thomas weights could not be calculated for seven women: six of them had no information on gestational age at the early pregnancy measure and one had no information on parity.
The level of agreement between the methods for GWG is shown in Table 4 and was less good than for BMI category. Seventy-two per cent of women were allocated to the same group using the early pregnancy weight and recalled weight (Table 4a), and 73% for the Thomas weight and recalled weight (Table 4b). For the two comparisons, 24 (1.3%) and 27 (1.4%) women, respectively, were in the inadequate weight gain category according to one estimate and the excessive weight gain category according to the other. Concordance between GWG categories using the early pregnancy weight and Thomas weight was higher at 95%, and no women were categorised as having weight gain that was inadequate using one method and excessive by the other.
Table 4. Numbers of women falling within different gestational weight gain (GWG) categories when different adjusted estimates of pre-pregnancy weight were used

a Data on gestational age at the time of the late pregnancy weight measurement were missing for six women.
b Thomas weights could not be calculated for seven women: one of them had no information on parity and six of them had no information on gestational age at the early pregnancy measure; they also had no gestational age information in late pregnancy.
Discussion
Main findings
Weight measurements made in early pregnancy and estimates using the Thomas method were on average 0.88 kg higher than actual pre-pregnancy measured weights. Both these methods were closer on average to the measured pre-pregnancy weights than recalled weights, which underestimated the pre-pregnancy weight by a mean of 1.65 kg. The early pregnancy weights and the Thomas weights had narrower limits of agreement than the recalled weights when compared with the pre-pregnancy measured weight. While women can provide a recalled pre-pregnancy weight estimate, not all can do so precisely. Notably, women who were heavier tended to underestimate their pre-pregnancy weight more than those who were lighter. The Thomas method also showed a tendency to underestimate weights of women who were heavier, but not to such an extent. There was less evidence that the early pregnancy weights underestimated the pre-pregnancy weights as women became heavier.
Some women recall their weights with considerable error and in 2.5% of women the error exceeded 10 kg. Even when the analysis was confined to those women whose early pregnancy visit occurred later in gestation, the measurements at those early pregnancy visits or the Thomas weights were still more accurate estimates of pre-pregnancy weight than the recalled weights. The sensitivity analysis restricted to those who became pregnant within 1 month of initial interview showed similar results to the findings from the full sample. Thus, a measurement of weight during the first trimester or use of the Thomas method provides a more accurate and precise estimate of the pre-pregnancy weight than a recalled measure, though, due to the weight gain in early pregnancy, a measurement made during this time overestimates the pre-pregnancy weight by 0.88 kg on average. Despite the adjustments made for other factors in the Thomas method, the resulting estimates differed little from the early pregnancy weights.
Our comparison of the proxy weight measures in the full SWS cohort and their use in the calculation of pre-pregnancy BMI and GWG showed considerable differences between the use of recalled weights and the other two proxy weights. Some women were classified into different BMI or GWG groups depending on which weight estimate was used. The discrepancies were greater for GWG than for pre-pregnancy BMI. It is worth noting that GWG uses the pre-pregnancy weight estimate twice in its calculation, as the categorisation is based both on pre-pregnancy BMI and on the change in weight from before to late pregnancy.
Comparison with other studies
A comprehensive systematic review of the accuracy of self-reported pre-pregnancy weight found that the mean underreporting in the reviewed studies ranged between 0.29 and 2.94 kg but the variability around the means, and thus the precision of the estimates, was rarely quantified. Reference Headen, Cohen, Mujahid and Abrams24 The time between the gold standard recorded measurement and the date of conception was not often recorded, though some studies restricted the measurements to specific time periods prior to conception. Reference Han, Abrams, Sridhar, Xu and Hedderson25,Reference Mandujano, Huston-Presley, Waters and Catalano26 Some studies simply compared current reported weight, rather than a pre-pregnancy recalled weight, with an early pregnancy measured weight to check the accuracy of reported weights. Reference Mandujano, Huston-Presley, Waters and Catalano26,Reference Fattah, Farah, O’Toole, Barry, Stuart and Turner33,Reference Jeffs, Sharp, Gullam and Paterson34 The gold standard measurements in the reviewed studies that had pre-pregnancy weights were made at clinical visits prior to pregnancy, so the women in these studies were seeking healthcare at the time and may not be the representative of the general population. It is also theoretically possible that women who have been measured formally for the gold standard assessment may later recall their pre-pregnancy weight more accurately than women who have had no such measurement made, a problem that affects our study too.
Strengths and limitations
To our knowledge, no other study has measurements of pre-pregnancy weight assessed in a research setting on regularly calibrated scales and then measured in pregnancy using scales calibrated in the same way. The initial pre-pregnancy measurements were made in women aged 20–34 years drawn from the general population, rather than women seeking medical care.
The age range in this study did not extend below 20 or above 35 years nor were the women diverse in terms of ethnicity, as 94% of them were White. The data were collected around two decades ago. Since then, rates of overweight and obesity have been rising, though not as rapidly as before 2000. Reference Baker35 More than 40% of the study women were affected by overweight or obesity compared with current estimates closer to 50% for women in the same age group, Reference Conolly and Craig36 so our study population may not represent women currently entering pregnancy.
Over the past two decades, it is possible that women have become more aware of their weight and recall it more accurately. Two general population studies conducted later than ours have shown smaller differences between recalled and measured weight than we did but wider limits of agreement than we have shown here. However, these studies were not in women who were pregnant and one of these focused only on individuals with overweight. Reference Yoong, Carey, D’Este and Sanson-Fisher37,Reference Beleigoli, Andrade and de Fátima38 The most recent study we have found comparing recalled weight in pregnancy with pre-pregnancy weight Reference Bannon, Waring and Leung39 also had a smaller difference between the two measures than we did, at approximately 1 kg. Notably, though, the SD of the differences was large at 5.2 kg, compared with 3.0 kg in our study, and their range of differences from −47.0 to 45.4 kg was also wider than the range seen in our study (−17.6 to 7.1 kg). This study, conducted more than a decade after ours, albeit in the United States, indicates that women, while on average becoming more accurate, may have become less precise in recalling their pre-pregnancy weight than we found in our study. We have been unable to find other recent studies comparing recalled and actual weights over short periods of time. Generally, while the average differences between recalled and measured pre-pregnancy weights are not large and may have reduced over time, the precision is poor and, for individual women, the error can be great.
The number of women contributing to the development of the recommendations in this study is modest, but as date of conception cannot be predicted, increasing this number would be difficult. Indeed, few studies have attempted to estimate pre-pregnancy weight and compare the various estimates with actual measurements. We compared the estimates of pre-pregnancy weight from the formula derived by Thomas et al. Reference Thomas, Oken and Rifas-Shiman29 with our early pregnancy weights and found that they were remarkably similar. However, our early pregnancy measures were all around 11 weeks’ gestation (range 8.5–14.5 weeks). The Thomas formula may well provide more useful measures if the first weight assessment in pregnancy occurs at a later gestation, as it applies up to 20 weeks’ gestation. Thus, in different populations, given that the method of Thomas et al. allows adjustment for a variety of relevant factors, their method may well provide a more useful approach. However, it is noteworthy that our early pregnancy estimates and those derived from the Thomas method were almost identical, and the Thomas method also had an element of overestimation of a mean of 0.88 kg in our study. This may reflect differences in procedures between routine clinical and research weight measures.
Conclusions and recommendations
Recalled measures may be the only estimates of pre-pregnancy weight available and, if so, then they would benefit for an adjustment to account for the underestimation. However, we suggest that early pregnancy weights or use of the Thomas method provide better estimates where the data are available, particularly if an adjustment for overestimation is made. The Thomas method requires more data than the early pregnancy weights, though the information required is likely to be available for its use, but not always. That method may also be useful if the earliest weights available occur later in gestation than in our study.
Only if an actual measure of weight has been recorded in the immediate preconception period and a measured weight near the end of the first trimester is available, it does seem possible to estimate first trimester weight gain. As considerable error exists in recalled weights, estimates of first trimester weight gain using such measures should be interpreted cautiously.
Acknowledgements
The authors thank the women of Southampton and their children who gave their time to take part in the Southampton Women’s Survey and the research nurses and other staff who collected and processed the data.
Financial support
This work was supported by grants from the Medical Research Council (MC_UU_12011/4), National Institute for Health Research Southampton Biomedical Research Centre, University of Southampton and University Hospital Southampton National Health Service Foundation Trust, the European Union’s Seventh Framework Programme (FP7/2007-2013), project EarlyNutrition (grant 289346) and European Union’s Horizon 2020 research and innovation programme under grant agreement No 733206, 9.6 M€ (LifeCycle). KMG is supported by the National Institute for Health Research (NIHR Senior Investigator (NF-SI-0515-10042) and the NIHR Southampton Biomedical Research Centre) and the European Union (Erasmus+ Programme Early Nutrition eAcademy Southeast Asia-573651-EPP-1–2016-1-DE-EPPKA2-CBHE-JP). Study participants were drawn from a cohort study funded by the Medical Research Council and the Dunhill Medical Trust. The funders had no role in the conduct of the research nor in the interpretation of the results.
Conflicts of interest
In relation to the current work, none of the authors report any conflicts of interest. However, we report that CC has received fees and honoraria from Amgen, Eli Lilly, GSK, Medtronic, Merck, Novartis, Pfizer, Roche, Servier, Takeda and UCB. KMG has been reimbursed for presenting at Nestlé Nutrition Institute conferences and has received grants from Abbott Nutrition and Nestec, outside the submitted work. JB has received grants from Danone Nutricia Early Life Nutrition and is part of a collaboration with Iceland Foods Ltd. HI reports that, while not directly receiving funding from other bodies, members of her team have received funding from Danone Nutricia, Nestec and Abbott Nutrition.
Ethical standards
All phases of the SWS were approved by Southampton and South West Hampshire Local Research Ethics Committee, and written consent was obtained from all participants.
Details of contributors
HI conceived the idea, conducted the analyses, drafted the paper and is the guarantor for this work. HI, CC, KG, SR, JB and SC designed and led the Southampton Women’s Survey and oversee its data quality and use. SC assisted with the statistical analysis. JH oversaw the data collection performed by the research nurses and ensured regular calibration of the weighing scales. All authors contributed to drafts of the paper and approved the final version and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data availability
Due to ethical concerns and original agreements made with participants, supporting data cannot be made openly available. The SWS team can provide the data on request subject to appropriate approvals. Researchers wishing to use the data would need to make a formal application to the SWS Oversight Group through the cohort PI and this paper’s corresponding author (Hazel Inskip: hmi@mrc.soton.ac.uk) and ensure appropriate ethical approval is in place. Subject to approval and formal agreements being signed, the data would then be provided.









