Introduction
Pediatric subspecialist shortages in the United States challenge health systems’ ability to provide timely access to care (Children’s Hospital Association, 2012; Ray et al., Reference Ray, Bogen, Bertolet, Forrest and Mehrotra2014). The primary care physician (PCP) coordinates clinical care and resource utilization (Donohoe et al., Reference Donohoe, Kravitz, Wheeler, Chandra, Chen and Humphries1999; Weeks and Wallace, Reference Weeks and Wallace2003), identifies conditions and complaints outside the scope of primary care, and refers to subspecialists or hospitalists (Fernandez et al., Reference Fernandez, Grumbach, Goitein, Vranizan, Osmond and Bindman2000; Rappaport et al., Reference Rappaport, Adelizzi-Delany, Rogers, Jones, Petrini, Chaplinski, Ostasewski, Sharif and Pressel2013). The pediatric subspecialist is a pediatrician who seeks additional fellowship training and specializes in care of more complex patients with a more specific organ-system focus. Due to large regional shortages of fellowship-trained pediatric subspecialists (Children’s Hospital Association, 2012), patients experience long wait times for new appointments. In addition, pediatric subspecialists have high volumes of referred patients without complex issues; rather, with common organ-system specific pediatric concerns. Often, PCPs are faced with managing high volumes of low-complexity patients but with limited time to address some organ-system specific health needs.
Improving access to care is a focus of significant efforts in today’s changing health system (Green et al., Reference Green, Savin and Murray2007; Berwick et al., Reference Berwick, Nolan and Whittington2008). Our children’s hospital’s approach to improving access arose through input of clinicians (subspecialists and generalists), administrators, family advisory council members, and referring PCPs (Sharif et al., Reference Sharif, Gartner, Plesnick and Greenspan2012). Access Clinics combine an ‘Access Pediatrician’ (AP), a board-certified general pediatrician embedded within subspecialty divisions who functions as a ‘generalist-as-specialist’, with specific nurse navigation for patient triage of patients with low-complexity complaints (Di Guglielmo et al., Reference Di Guglielmo, Plesnick, Greenspan and Sharif2013). Side-by-side practice within the subspecialty’s clinical space and real-time availability of consultation with subspecialists enhance the AP’s expertise. At scheduling, patients or PCPs may request to not see the AP, and these patients are scheduled directly with the subspecialist. However, use of APs can increase access and provide timelier visits while removing barriers to evaluation for patients; as a result, subspecialists are free to see more complex and acutely ill patients.
Evaluating the sustainability of Access Clinics as care delivery transformation requires analysis of the factors driving referrals and assessment of referring physician perceptions (Fernandez et al., Reference Fernandez, Grumbach, Vranizan, Osmond and Bindman2001; Pletcher et al., Reference Pletcher, Rimsza, Cull, Shipman, Shugerman and O’Connor2010). Sustainable transformation relies on understanding practice culture and its effect on practice change, PCP perceptions and needs (Dempster et al., Reference Dempster, Wildman and Duby2015), and the ‘buy-in’ of referring PCPs (Abatemarco et al., Reference Abatemarco, Kairys, Gubernick and Kairys2008; Reference Abatemarco, Kairys, Gubernick and Hurley2012). The present study aims to determine the referring PCPs’ most prevalent perceptions about the AP/Access Clinics as well as to characterize the influence of external factors.
Methods
Study period, data
Access Clinic encounters between September 2011 and April 2014 were reviewed; PCP office ZIP code and number of patients referred were recorded. The Institutional Review Board waived approval of the research study, #306671.
Survey
Eligible PCPs (referred at least three patients) were individually and anonymously surveyed with online questionnaires (eight questions) using REDCap software (Harris et al., Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde2009). Results were collected over 100 days beginning in April 2014. The survey queried perceptions of communication with the Access Clinic, satisfaction with patient care, knowledge about the Access Clinic, and reasons for referral. The survey solicited open-ended comments (‘Please provide any feedback, comments, or questions’). We coded qualitative data by major themes (Crabtree et al., Reference Crabtree, Miller, Aita, Flocke and Stange1998).
Geographic and economic data collection
Distance between ZIP codes and the Access Clinic were obtained from www.googlemaps.com. Census data on population, households with children <18, median income, and number of health practitioners per ZIP code were obtained from www.factfinder2.census.gov. ZIP code data for referring PCP offices were stratified into quartiles by ranking the number of patients referred per PCP. We reported the top quartile.
Statistical analysis
Descriptive statistics were calculated. In the analysis of ZIP code data, linear regression represented ZIP code rank against each dependent variable, using the best fit trend line (R 2).
Results
Patient characteristics
Patients were majority female; aged <1–17 years distributed in quintiles of four-year increments above age 1 (Table 1). A total of 62.3% of families were privately insured. Of the 2139 new outpatients, 1438 (67.2%) were referred by their PCP.
Table 1 Demographics; frequency of referrals
Referring PCP characteristics
PCPs were employed by either the children’s hospital’s primary care network of practices or were unaffiliated and working in community practices. Three hundred twenty PCPs were eligible (patients referred: range 3–85, median 6.5, IQR 8) including 47 hospital-affiliated PCPs (14.7%) and 273 non-affiliated PCPs (85.3%). Of note, 21 hospital-affiliated PCPs and 49 non-affiliated PCPs referred 12 or more patients (top quartile). Surveys were emailed to 41 hospital-affiliated PCPs (six had left the hospital network at the time of the survey) and 103 non-affiliated PCPs. Of the remaining 170 non-affiliated PCPs, 151 were successfully contacted by fax.
Survey response
Thirty-three hospital-affiliated PCPs and 42 non-affiliated PCPs responded to the emailed survey; five non-affiliated PCPs responded to the faxed survey invitation. Email response rate was 52.1% (75/144); overall response rate was 27.1% (80/295). The PCPs in the top quartile responded to the survey at a rate of 51.4% (36/70). PCPs were somewhat [23%] or definitely [70%] satisfied, viewed patients having had somewhat [29%] or very [63%] positive experiences, and knew the type of patients appropriate for Access Clinic evaluation (PCPs somewhat [24%] or definitely [65%] understood). Reasons for referral were varied, focusing on patient needs and practice limitations, but also family preference, shortened wait times, and prior unsuccessful management. The most common reasons for referral were: ‘I felt patient needed appointment sooner than subspecialty could accommodate’ (61%) and ‘family requested referral’ (58%). Forty-six percent and 44%, respectively, responded that the reasons for referral were: ‘Unsuccessful in managing patient with these symptoms’ and ‘Beyond scope of practice.’ PCPs responses indicated they found follow-up communication from the AP to be helpful (23% somewhat, 74% definitely) and 80% would like to be able to communicate more with the AP, although only 44% reported contacting the AP after their patient’s visit. PCPs indicated direct phone call (35%), Electronic Medical Record message (21%), or email (21%) as top communications preferences.
Qualitative comments
Of the 80 survey responses, 24 PCPs provided comments (30.0%, Table 2): positive experiences about efficient and appropriate care; constructive comments about communication; and critical comments expressing dissatisfaction due to preference for subspecialist care.
Table 2 Qualitative comments from referring PCP survey
PCP=primary care physician.
Geographic and economic trends
The study area included 11 urban clusters and three urbanized areas with the remaining regions predominantly rural. PCPs were located in a variety of geographic areas throughout the state (the hospital’s primary service area) and region. The top quartile of ZIP codes, ranked by patients per referring PCP (range 3–31, median 5.9, IQR 4.85), contained 21 ZIP codes, with all but one within the state (Table 3). One ZIP code (19902) had unavailable census data.
Table 3 Top quartile of most referrals to the access clinic (by patients referred/PCP): ZIP code data
PCP=primary care physician.
The five ZIP codes with the most patients referred corresponded to suburban population centers (Table 3, column 3). The ZIP code where the Access Clinic is located, 19803, represented 25.7% of patients. Examining the next five ZIP codes with the most patients referred, the average distance traveled was 25 miles (range 11–54 miles, median 20 miles, and IQR 10 miles). The five ZIP codes with the most referrals per PCP corresponded to five different urban and suburban population centers (average 21 patients/PCP, range 14–31, median 20.5, IQR 4.6; Table 3, columns 3–5). The average distance traveled from the five ZIP codes was 44.8 miles (range 14–90 miles, median 47 miles, IQR 33 miles; Table 3, column 6).
For the top quartile of PCPs, the PCPs that referred the most patients were no farther away than the PCPs that referred the least patients (Figure 1a, R 2=0.0007). The lack of correlation extended to the entire cohort of PCPs (data not shown).
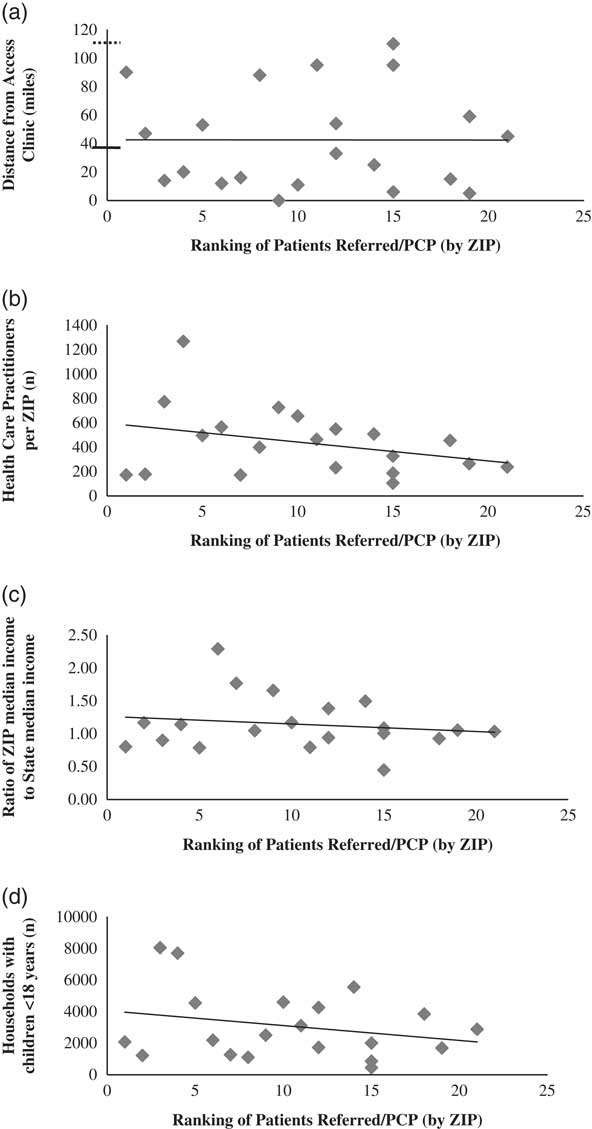
Figure 1 Rank of patients referred per primary care physician (PCP) by ZIP against (a) distance (in miles) of each PCP in Table 3. Y-axis solid line: distance cut-off between hospital’s primary and secondary service areas; stippled line: between secondary and tertiary. (b) Ratio of ZIP to State median income; (c) number of health care practitioners from each ZIP; (d) number of households with children under 18 for each ZIP. Linear regressions: (a) R 2=2×10−6, (b) R 2=0.0267, (c) R 2=0.1053, (d) R 2=0.0652.
ZIP codes with the most frequently referring PCPs had varied median incomes (range $26 955-$137 617; median $63 154.50; IQR $18 240), and slightly higher ratios of median income to state median income ($60 119, Figure 1b). The same ZIP codes had higher numbers of health care practitioners (range 105–1266; median 427; IQR 331; Figure 1c) and higher proportions of children to adults (range 13–33%; median 27%; IQR 6%, Figure 1d).
Discussion
The Access Clinic transforms outpatient subspecialty care delivery at the children’s hospital studied. The intent of the Access Clinic is (a) to provide appropriate and comprehensive care when the patient wants it and needs it, and (b) to direct the patient back to the PCP, or on to the subspecialist, as clinically warranted. The referring PCP is essential to the Access Clinic model as co-manager of the patient. Continuous improvement of the innovative care delivery system requires the PCP perspectives identified in the survey to be integrated with other stakeholder input, patient experiences, health outcomes, and cost effectiveness data (Kleinman and Dougherty, Reference Kleinman and Dougherty2013).
The primary aim of the study is to examine stakeholder perceptions. Referring PCPs are satisfied with the Access Clinic due to shorter wait times and high quality care. The PCP is referring to a ‘generalist-as-specialist,’ not another PCP (Sharif et al., Reference Sharif, Gartner, Plesnick and Greenspan2012). PCPs are comfortable with which patients to refer and are satisfied with the Access Clinic. Many PCP comments and survey responses (Table 2) regarding the care their patients experienced provide constructive feedback with themes of family preference, AP expertise, timely care delivery, and bi-directional communication.
Another aim of the study is to understand the influence of external factors on referrals. PCPs refer to the Access Clinic from different population centers and areas with varied PCP densities and diverse demography. Overall, patients came from an average of 25 miles away, but patients referred by the PCPs with the highest referral rate traveled an average of almost 45 miles. Distance was no barrier to these referrals (Figure 1a). Regional factors such as economic characteristics, pediatric population, and distance from the clinic do not appear to affect referral rate. Regression shows regions with higher median income (Figure 1b) and with larger populations of households with children <age 18 (Figure 1c) correlate with greater referrals/PCP. Distance, income, and population did not deter referrals. Other factors, such as quality of care, ease of making appointments, and short wait times may be more likely to influence referral decisions. We conclude that demand for immediate subspecialty care supersedes geographic, population, or economic factors (Figure 1), family demands are paramount to PCP referral patterns, and routine ‘in office’ subspecialty care by the PCP may be limited by resources or interest.
The demand for subspecialty evaluation in place of, or to complement, PCP evaluation is not unique (Anderson et al., Reference Anderson, Marks, Downs, Buckel, Adams, Enterline and Miller2007; Martin et al., Reference Martin, Currie and Finn2009; Hsu et al., Reference Hsu, Schwend and Julia2012). For the Access Clinic, the involvement of local referring PCPs and subspecialists in the planning stages has been critical to aligning service delivery with demand. In other health care systems, the PCP or generalist nurse may serve as the ‘gatekeeper’ for subspecialty care (Ramritu et al., 2002; Wilkie, Reference Wilkie2013), with more time or resources to see patients with routine complaints, only referring to subspecialists for more complex patient evaluations. International models using general pediatricians with specialty interest, or ‘GPSIs’ (Salisbury and Rosen, Reference Salisbury and Rosen2007; Martin et al., Reference Martin, Currie and Finn2009), if well-designed, show improved access and increased bi-directional communication. In the United States, health care delivery systems that ‘train up’ community pediatricians to provide subspecialty care in the primary care medical home setting have been proposed (Ray Tsai MD, 2014, personal communication).
Limitations of our study include recall bias (surveys), low response rate, and applicability. PCPs with high referrals are more likely to be affiliated thus more familiar with the Access Clinic, introducing potential favorability bias. Non-affiliated PCPs referred more patients but had a poor response rate. Survey participation was not incentivized (Delnevo et al., Reference Delnevo, Abatemarco and Steinberg2004), affecting response rate. Access Clinics have not been widely implemented or described nationally, so while applicability may be affected by studying one institution, critical information about evaluation of the model will inform academic centers about novel ways of delivering appropriate subspecialty care.
Pediatric subspecialty shortages continue to plague the effective and timely delivery of health care to children (Pletcher et al., Reference Pletcher, Rimsza, Cull, Shipman, Shugerman and O’Connor2010; Ray et al., Reference Ray, Bogen, Bertolet, Forrest and Mehrotra2014). Successful solutions demand identification of key drivers of referrals, understanding of PCP attitudes (Twamley et al., Reference Twamley, Craig, Kelly, Hollowell, Mendoza and Bluebond-Langner2014), and consensus among referring PCPs. Access Clinics can reinforce the ‘generalist-as-specialist’ paradigm for appropriate patients, improve care quality, and connect subspecialty and primary care practices.
Acknowledgements
The authors would like to acknowledge J. Fernando del Rosario MD, Christine Chisholm MBA, Joanne Plesnick MBA, J. Carlton Gartner MD, and Iman Sharif MD MPH for their support of the work for this paper.
Funding source
Work supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number U54-GM104941 (PI: Binder-Macleod).
Conflicts of Interest & Financial Disclosure
The authors have no relevant financial relationships to disclose. The authors have no conflicts of interest to disclose.






