Introduction
Despite being introduced years ago in animal Reference Peuster, Fink and Klima1 and clinical studies, Reference Hausdorf, Schneider and Konertz2,Reference Galantowicz and Cheatham3 the percutaneous creation of a total cavopulmonary connection has yet to gain widespread adoption as the preferred approach for completing the staged palliation of univentricular hearts. However, the evident advantages of this approach—such as avoidance of open-heart surgery with cardiopulmonary bypass, elimination of intubation and positive-pressure mechanical ventilation, shorter ICU stays and reduced atrial scarring and associated arrhythmias—should not be underestimated. We report on a patient with tricuspid atresia in whom, after minimal surgical preparation, a percutaneous completion of a Fontan circulation was successfully performed.
Case report
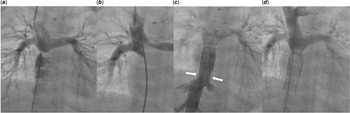
After approval of the local ethics committee, a non-restrictive, dilatable banding of the inferior vena cava with a diameter of 12 mm was placed during the operation for the superior cavopulmonary connection. At the age of 2 years, the patient (weight 12.7 kg) was scheduled for the intervention of Fontan. The mean pulmonary artery pressure was 9 mmHg, and the transpulmonary gradient was 2 mmHg, indicating favourable haemodynamic conditions for total cavopulmonary connection completion. The procedure was performed under real-time guidance of a biplane fluoroscopy system. The right pulmonary artery was punctured with a transseptal needle from the right groin through the roof of the right atrium (Figure 1a,b). Subsequently, a long sheath (12F) was introduced without the need for balloon dilatation. A 0.035’ Amplatz Ultra Stiff ™ (Boston Scientific, Marlborough, MA, USA) guidewire was used to establish and maintain the circuit throughout the procedure, ensuring adequate support for stent delivery and deployment. A Fontan circulation was established (Figure 1c, d), using two overlapping covered stents (Optimus, AndraTech GmbH, Koblenz, Germany) on 14 mm balloons (BiB, NuMed, Hopkinton, NY, USA) anchored in the banded inferior vena cava and in the puncture site of the pulmonary artery, respectively. The first stent, measuring 33 mm, was deployed in the inferior vena cava. The second stent, 38 mm in length, was positioned to bridge the connection toward the pulmonary arteries. Both stents were post-dilated to achieve full expansion and optimal sealing. During the implantation, repeated contrast injections were used to identify the proximal and distal landing zones, ensuring avoidance of the hepatic veins and unobstructed flow to the pulmonary arteries. During the whole procedure, the patient was spontaneously breathing and haemodynamically stable. She was monitored in the ICU for one night. The postinterventional recovery was uneventful under 0,3 mg/kg/min milrinone and gentle volume substitution. Lifelong anticoagulation with warfarin was initiated, following the standard approach for all Fontan patients in our clinic. The patient was discharged home after 7 days. The follow-up period was 17.1 months. During this time, the child remained in a very good clinical condition. The next catheterisation is planned 48 months after the intervention to re-dilate the 14 mm stents to a larger size.

Figure 1. ( a ) Initial anatomy showing the proximity of the roof, the right atrium and the lower part of the right pulmonary artery. ( b ) The right atrium and pulmonary artery are connected by a puncture with a transseptal needle. ( c ) Creation of an intracardiac conduit using two covered stents between the banded IVC and the right pulmonary artery. ( d ) Injection into the superior caval vein showing unobstructed flow into both pulmonary arteries.
Discussion
Since the publication of the clinical study by Hausdorf et al. in 1996, in which interventional total cavopulmonary connection was performed in 8 patients, Reference Hausdorf, Schneider and Konertz2 there has been an ongoing debate as to whether this approach could serve as an alternative to surgical total cavopulmonary connection as the final stage of univentricular palliation. However, this treatment option has not been adopted into routine clinical practice for nearly 30 years. Cheatham et al. reported on five patients who successfully underwent percutaneous Fontan completion. In their approach, no inferior vena cava banding was performed during the Glenn procedure. This resulted in dilation of the inferior vena cava during follow-up and cyanosis due to a right-to-left shunt around the inferior margin of the stent into the right atrium. For that reason, these patients required re-catheterisation with redilatation or re-stenting shortly after the initial procedure. Based on their experience, our patient received inferior vena cava-banding to avoid this complication.
The limited availability of published data, the absence of long-term follow-up, and the innovative—even visionary—nature of this pioneering approach contribute to a degree of hesitation among interventional cardiologists. A growing database on this intervention will likely support the adoption of this less-invasive treatment modality by centres worldwide. It is important to emphasise that this approach overcomes several limitations of surgery, such as the need for intubation and positive-pressure mechanical ventilation, longer stays in the ICU and atrial scarring with associated arrhythmias.
Atrial scarring resulting from surgical total cavopulmonary connection procedures may lead to sick sinus syndrome, and in many patients, a junctional rhythm is observed on ECG. While this may be well tolerated in otherwise healthy patients with biventricular circulation, it can pose a significant challenge in those with single-ventricle physiology. Reference Alnoor, Burch, Armsby, Batra and Balaji4 Atrioventricular synchrony is an important factor in preventing the development of Fontan failure and may constitute an indication for pacemaker implantation in patients with univentricular circulation. Reference Alnoor, Burch, Armsby, Batra and Balaji4 In the percutaneous approach, atrial scarring can be minimised, and the risk of rhythm disorders is reduced.
In contrast to others Reference Prabhu, Maiya and Shetty5 , in our case, the non-restrictive inferior vena cava banding is only a concomitant procedure to the superior cavopulmonary connection performed without prolongation of cardiopulmonary bypass time. The interventional Fontan completion is based on a technique for vascular anastomoses using needle puncture and implantation of covered stents Reference Ewert, Eicken and Tanase6 and is performed without positive pressure ventilation. Reference Georgiev, Balling and Ruf7 The stents and the dilatable banding allow an adjustment of the conduit size with to the patient’s growth.
Conclusion
The presented technique allows successful percutaneous completion of the Fontan circulation after minimal surgical preparation during the Glenn operation.
Competing interests
The authors have no conflict of interest.