Introduction
Radiotherapy contributes to cure or palliation in more than half of cancer patients. Despite this central role, Italian radiation oncology (RO) residency programmes have struggled to fill available positions since 2023. Reference Petrianni, Fiore and Onorati1 Recent yAIRO data show that in 2022, 79% of residency posts were unassigned or abandoned, and the situation has only partially improved: in 2025, 65% of the advertised positions remained unfilled, with 92 out of 141 posts left vacant 2 and many schools having no first-year residents. This severe and persistent shortage highlights the urgent need for strategies to attract, motivate and retain future radiation oncologists.
Limited undergraduate exposure is a recognised barrier to recruitment worldwide Reference Ingledew, Lalani, Daly and Campbell3,Reference Wu, McCloskey, Wallner, Steinberg and Raldow4 yet Italian-specific evidence remains scarce. Reference Nardone, Boldrini and Salvestrini5 We therefore measured the immediate educational impact of a very brief RO rotation on fourth-year students—when specialty preferences begin to crystallise—and explored which factors weigh most in their career decisions.
Innovation
Setting and participants
Between November and December 2024, 50 consecutive fourth-year students from Università Cattolica del Sacro Cuore completed a six-hour rotation in the Radiation Oncology Department of Fondazione Policlinico Universitario A. Gemelli IRCCS. The programme combined a concise overview of indications and technology, a guided tour of external-beam and brachytherapy units, access to the treatment-planning suite and observation of at least one outpatient consultation.
Survey tool
An anonymised paired questionnaire was administered immediately before and after the rotation. It covered three domains: (1) importance (Likert 1–5) of predefined factors in specialty selection; (2) knowledge and perceptions of RO; and (3) current intention to pursue RO as a career. Categorical variables were compared with McNemar tests (SPSS v28).
What drives specialty choice?
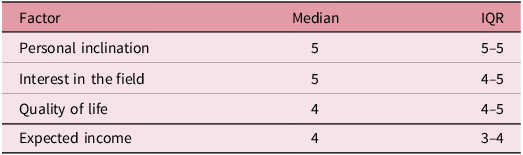
Personal inclination and genuine interest topped the list (median 5, IQR 5–5), followed by quality of life and expected income (both median 4), consistent with earlier research. Reference Schroeder, Brown and Stone6 Rankings are summarised in Table 1.
Table 1. Importance of factors influencing specialty choice (median rating, IQR)

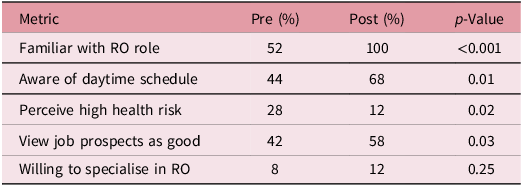
Knowledge before and after the rotation
Before the rotation, 52% of students felt able to describe a radiation oncologist’s daily work; 28% considered occupational radiation exposure a major health risk. Afterwards, every student reported a clear understanding of the specialty and the perceived hazard fell to 12% (p = 0.02). Confidence in future job opportunities rose from 42 to 58% (p = 0.03). Comparable gains have been seen in other academic settings. Reference Teles, Whitehouse and Kapoor7 Detailed results appear in Table 2.
Table 2. Pre- versus post-rotation knowledge and attitudes towards radiation oncology (n = 50)

Impact on career intentions
Initially, 8% of students were interested in RO. This rose to 12% post-rotation; the undecided group grew from 40 to 42%, and those excluding RO dropped from 40 to 36%. The main reason for disinterest was commitment to another specialty, echoing findings by Wu et al. Reference Wu, McCloskey, Wallner, Steinberg and Raldow4
Discussion
A single, structured morning in an RO department can erase major knowledge gaps and safety misconceptions among medical students. Reference Teles, Whitehouse and Kapoor7 Although the shift in career intent was modest, it moved in the right direction and suggests that early exposure at least keeps the door open.
As previous Italian surveys have shown, Reference Nardone, Boldrini and Salvestrini5 personality fit and subject passion outweigh lifestyle issues in specialty choice; however, recent data from yAIRO indicate that radiotherapy is still poorly covered during medical school, with most residents reporting limited exposure and knowledge of the specialty before enrolling in residency.
Evidence from the literature and our findings suggests that lasting change in recruitment will likely require longer rotations, mentorship programmes and clearer information on private-practice opportunities. Earlier and more structured exposure would help students appreciate both the clinical and technological scope of RO, while mentorship and brief shadowing experiences could offer a more realistic understanding of daily practice. Providing transparent career information and highlighting the field’s technological appeal may further support engagement. Coordinated initiatives across medical schools could also ensure more consistent exposure. Together, these measures would complement brief clinical encounters and help sustain interest in the specialty over time. Reference Petrianni, Fiore and Onorati1,Reference Smith and Jones8
Study limitations include single-centre design, small sample size and lack of long-term follow-up. Multi-centre studies with longitudinal exposure and tracking of actual residency applications are warranted.
Recommendations
Even minimal clinical exposure substantially improves students’ understanding of RO and tempers unfounded fears, but deeper and sustained initiatives are needed to convert heightened awareness into a stronger workforce.
Acknowledgement
The authors thank all the students participating in the survey for their contribution.
Financial support
The authors declare that no funds, grants or other support were received during the preparation of this manuscript.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics standards
Not required.
Author contributions
Massaccesi M conceived the presented idea.
Autorino R, Massaccesi M and Rinaldi RM developed the theory.
Rinaldi RM collected the data and performed the statistical analysis.
Massaccesi M and Rinaldi RM wrote the paper.
Autorino R, Dinapoli N and Gambacorta MA supervised the findings of this work.
All authors discussed the results and contributed to the final manuscript.