Background
For women, self-harm is associated with up to 50 times higher risk of suicide.Reference Cooper, Kapur, Webb, Lawlor, Guthrie and Mackway-Jones1 Between 2014 and 2016, 2.9 deaths per 100 000 maternities (95% CI 2.2–3.6) (during pregnancy and up to 1-year postpartum) were suicides, representing 18% of all maternal deaths in the UK.Reference Knight, Bunch, Tuffnell, Jayakody, Shakespeare and Kotnis2 The most recent Confidential Enquiry into Maternal DeathsReference Knight, Bunch, Tuffnell, Shakespeare, Kotnis and Kenyon3 recommended that women who self-harm during pregnancy should be prioritised and targeted for intervention. Such targeting requires detailed, high-quality information about the risks associated with pregnancy: better understanding of self-harm risk might lead to strategies that identify the most vulnerable women and reduce the number of preventable maternal deaths.
A recent systematic review provided some evidence that the percentage of women who self-harm is higher postpartum: (six studies, n = 11 400 women, median 1.03%; interquartile range (IQR) = 0.2–1.6%) than in pregnancy (six studies, n = 12 200 women, median 0.5%, IQR = 0–1.7%).Reference Ayre, Gordon, Dutta, Hodsoll and Howard4 Pooled prevalence estimates from hospital admissions data were inconclusive, however, only a minority of women who self-harm will seek help in hospital. In addition, the heterogeneous definitions of ‘perinatal’ and ‘self-harm’ make these pooled estimates difficult to interpret. None of these studies quantified the effect of pregnancy on self-harm relative to a background risk in matched, non-pregnant women. Such analyses are particularly important to address the effect of pregnancy in at-risk groups, including adolescents and women with a history of mental illness.
Using a primary care database, we have previously demonstrated that the number of children exposed to maternal mental illness has been increasing over the past two decades.Reference Abel, Hope, Swift, Parisi, Ashcroft and Kosidou5 This was noted for maternal depression, anxiety, bipolar disorder and alcohol misuse disorders, all of which are associated with increased rates of self-harm.Reference Abel, Hope, Swift, Parisi, Ashcroft and Kosidou5 There is evidence that self-harm among young women in the UK is also increasingReference Morgan, Webb, Carr, Kontopantelis, Green and Chew-Graham6 and there are renewed clinical concerns that self-harm during pregnancy may also be on the rise,Reference Ayre, Gordon, Dutta, Hodsoll and Howard4 particularly among young women,Reference Swift, Pierce, Hope, Osam and Abel7 in whom mental illness increases their likelihood of pregnancy. Unless we understand the level of risk faced by these women, providing services appropriate to their needs is unfeasible.
Aims
Clarifying risk is an important step towards meeting the needs of vulnerable mothers.Reference Abel and Rees8 Our aim, therefore, was to quantify rates of self-harm among non-pregnant women and compare these with rates in pregnant women and women in the first postpartum year. We asked if:
(1) pregnancy would reduce risk of self-harm;
(2) pregnancy effects depend on a history of mental illness;
(3) pregnancy effects are age-dependent; with older women being more likely to benefit from any protective effects of pregnancy; and
(4) self-harm risk postpartum varies by birth outcome.
Method
Design and data sources
In the UK primary care, equivalent to US family practice, is free at the point of access and 98% of the UK population is registered with a primary care practice.Reference Herrett, Gallagher, Bhaskaran, Forbes, Mathur and van Staa9 Importantly, primary care is typically the first health setting where illness is diagnosed and treated; if required primary care practitioners refer patients to specialist services or admit them to hospital.
To understand self-harm risk in pregnancy compared with other times we conducted a recurrent-event survival analysis using a retrospective cohort collected from a primary care patient database: the UK Clinical Practice Research Datalink (CPRD) GOLD. The CPRD contains individual-linked data on over 15 million patients, including data on clinical consultations, treatments, referrals and tests, in addition to patient demographics and practice data.Reference Herrett, Gallagher, Bhaskaran, Forbes, Mathur and van Staa9 The CPRD Pregnancy Register is a validated algorithm that links women to their pregnancies, using information from antenatal and delivery records of women and children.Reference Minassian, Williams, Meeraus, Smeeth, Campbell and Thomas10 Women were also linked to the Index of Multiple Deprivation (IMD) data-set that measures the relative social economic status of a particular area of England in 2010, based on the geographical area of the general practice, and is currently available for approximately 75% of registered English practices.Reference Herrett, Gallagher, Bhaskaran, Forbes, Mathur and van Staa9
Study population
The cohort was drawn from 3 624 708 women aged 15–45 years registered at an up-to-standard CPRD GOLD-participating practice from 1 January 1990 to 31 December 2017, where ‘up-to-standard’ provides a minimum date from when the data is of sufficient quality.Reference Herrett, Gallagher, Bhaskaran, Forbes, Mathur and van Staa9 Eligible women (2 666 088) included those registered for at least 2 years at a general practice, to establish prior exposure to mental illness and self-harm. Follow-up began on the latest date of their: 15th birthday; registration at a practice; ‘up-to-standard’ date. Censoring occurred at the earliest date of their: 45th birthday; study end date; transfer out date; clinical practice left CPRD; 6th pregnancy or 15th self-harm event.
Consent and ethics
It was not possible or appropriate to obtain written informed consent because this is observational research of anonymised patient data. Ethical approval for observational research using CPRD patient data reviewed by the Independent Scientific Advisory Committee (ISAC) was granted by a Health Research Authority Research Ethics Committee (East Midlands-Derby, REC reference number 05/MRE04/87), and this study was approved by ISAC (protocol number: 17_187).
We assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Outcome
Self-harm included ‘any act of self-poisoning or self-injury, irrespective of motivation’.11 A clinical recording of self-harm includes any record of self-harm or attempted suicide, the methods recorded in primary care include: drug overdose; cutting; suicide attempt (suicide attempt or para-suicide); self-poisoning (ingestion of toxic substances); other means (asphyxiation, drowning, jumping from a height or into danger and crashing a vehicle); and non-specific self-harm. The specific clinical codes used are available at clinicalcodes.org.Reference Morgan, Webb, Carr, Kontopantelis, Green and Cew-Graham12 We grouped self-harm events less than 21 days apart together. Analyses were restricted to the first 15 events, which accounted for 99.8% of self-harm events and reduced the size of the data-set and computation time.
Exposure
The main exposure was periods of pregnancy and postpartum. Periods of follow-up were divided into the following: non-perinatal; pregnant; and three postpartum periods (0–3, 3–6 and 6–12 months). Where a postpartum period and subsequent pregnancy overlapped, we right truncated the postpartum period to end 1 day before the subsequent pregnancy start date. Using the Pregnancy Register we identified birth outcomes, classed as either live birth, loss or termination. Pregnancy loss included miscarriage, ectopic pregnancy and stillbirth. The analysis was restricted to the first five pregnancies over follow-up.
Time-varying covariates
Mental illness
Follow-up was split into periods when women were exposed and unexposed to mental illness. Mental illness was defined using events for: serious (affective or non-affective psychosis); common (depression or anxiety); addiction (substance misuse and alcohol misuse); and other mental illness (eating and personality disorders). These events were identified using prescriptions, diagnoses and symptoms using previously published codes and methodology.Reference Abel, Hope, Swift, Parisi, Ashcroft and Kosidou5
Women were considered exposed to serious, addiction and other mental illnesses from the earliest event over follow-up until they were censored. Common mental illness was considered to be time-varying and episodic in nature therefore events less than 2 years apart were grouped together as a single episode. In this analysis, women experienced up to seven episodes of common mental illness.
Other time-varying covariates
In addition, follow-up was split by women's age (5-year age periods 15–45 years) and by calendar year (4-year periods from 1990 to 2017).
Time stable covariates
Data was extracted from the general practice data-set on the general practice's region of the UK (Scotland, Wales and Northern Ireland) and England (North East, North West, Yorkshire & The Humber, East Midlands, West Midlands, East of England, South West, South Central, London and South East Coast). The IMD quintile was used to measure deprivation. The IMD score linked to women's GP practice is ranked from lowest to highest and divided into quintiles, where the fifth quintile represents the most socioeconomically deprived. For this analysis, 561 731 (21.1%) of the women in this analysis were from practices outside England and were not assigned a rank.
Analyses
Using a gap-time approach and a stratified Cox model with 14 strata, representing the number of previous self-harm events we modelled the time-dependent risk of recurrent self-harm. To manage the non-independence of self-harm events, we calculated a baseline hazard function for each stratum. An important assumption underlying this approach is that women's risk of a second self-harm event occurred after their first self-harm event, meaning the number at risk reduced with each event.
To investigate the effect of pregnancy and postpartum periods on the risk of self-harm, we estimated hazard ratios (HRs) using periods outside of the perinatal period as the reference group. The main analysis involved two adjustments: (a) age group, year group, region and mental illness and (b) a fully adjusted model that included IMD and therefore excluded non-English practices, all confidence intervals (CIs) used Huber–White sandwich estimated standard errors. Schoenfeld residuals and Kaplan–Meier plots tested that the pregnancy exposure met the proportional hazards assumption. All analyses were conducted using Stata Version 16 and graphs were constructed using ggplot in R.
To investigate if the effect of pregnancy varied by age, mental illness and birth outcome three separate Cox regression models were fitted that included interactions between the covariate of interest (age, mental illness, birth outcome) and perinatal exposure (pregnancy, postpartum and non-perinatal period) to get covariate-specific estimates. Because the birth outcome is not known at pregnancy start, only the postpartum period was stratified in this interaction model. All models adjusted for region and year. Birth outcome adjusted for age, mental illness, region and year.
Sensitivity analyses
We conducted two sensitivity analyses to address the intersection of fertility, mental illness and age on risk of self-harm.
Women with serious mental illness are less fertileReference Hope, Parisi, Ashcroft, Williams, Coton and Kosidou13 therefore women who are never pregnant might raise the background risk and inflate the effect of pregnancy on self-harm. Therefore, we repeated the main analysis with those women who experienced pregnancy during follow-up (n = 1 298 256).
In adolescence, women with mental illness are more likely to become pregnant and to self-harm than women without mental illness, therefore arguably mental illness is both on the causal pathway or a confounder of any age-dependent effect of pregnancy on self-harm, to investigate this we conducted a sensitivity analysis that adjusted for mental illness.
Results
The cohort included 2 666 088 women aged 15–45 years who contributed 1 102 040 pregnancies, 57 791 self-harm events, and 14 712 319 person-years of follow-up time (Table 1). The median and longest follow-up was 4.03 and 27.9 years, respectively.
Table 1 Description of study and sample characteristics

a. Asphyxiation, drowning, jumping from a height or into danger and crashing a vehicle.
b. Eating and personality disorders.
Table 2 The unadjusted and adjusted risk of self-harm in pregnancy and post pregnancy periods for women aged 15–45 years

a. 1000 person-years.
b. Adjusted for age, year, region and mental illness variables.
c. Model adjusted as Model 1 plus Index of Multiple Deprivation quintile.
The baseline self-harm rate (per thousand person-years) was 3.90 (95% CI 3.87–3.93). The most common method of self-harm recorded was overdose (47 547, 82.3% of self-harm events).
All covariates considered in this study contributed to women's risk of self-harm. In particular, there was an increased risk associated with mental illness, living outside of London or in the most deprived areas of England and being younger (Supplementary Table 1 available at https://doi.org/10.1192/bjp.2022.31). The rate of self-harm doubled from 2.50 in 1990–1994 to 4.43 in 2014–2017 (HR = 1.97, 95% CI 1.85–2.10).
Effect of pregnancy
The self-harm hazard halved during pregnancy compared with any time outside the perinatal period (2.07 v. 4.01 events/1000 person-years, HR = 0.50, 95% CI 0.47–0.53). This halving remained after adjustment for region, calendar year and maternal age (adjHR = 0.53, 95% CI 0.49–0.58; Table 1). Postpartum, self-harm rates at 0–3 months (HR = 0.94, 95% CI 0.88–1.01) and 3–6 months (HR = 0.97 95% CI 0.92–1.02) were comparable with the reference period, women were at highest risk of self-harm at 6–12 months postpartum (HR = 1.09, 95% CI 1.04–1.14) (Table 1). The evidence for an increased risk of self-harm at 6–12 months postpartum weakened after adjustment for mental illness (model 1, adjHR = 1.02, 95% CI 0.97–1.07), and strengthened after adjustment for IMD quintile (model 2, adjHR = 1.08, 95% CI 1.02–1.15).
Is the risk of perinatal self-harm independent of mental illness?
In pregnancy, the risk of self-harm reduced by 60% for women with mental illness compared with outside the perinatal period (9.67 v. 21.6 events/1000 person-years, adjHR = 0.40, 95% CI 0.36–0.44, Fig. 1). Postpartum, a self-harm risk decreased at 0–3 months (adjHR = 0.77, 95% CI 0.71–0.85), 3–6 months (adjHR = 0.87, 95% CI 0.81–0.92) and 6–12 (adjHR = 0.92, 95% CI 0.87–0.98) months. Women with common, serious, addiction and other mental illnesses experienced similar risk decrements, most notable among women with a prior record of self-harm (see Supplementary Table 2 for values). In contrast, women without mental illness were at increased risk of self-harm postpartum (0–3 months, adjHR = 1.27, 95% CI 1.15–1.40, 3–6 months, adjHR = 1.13, 95% CI 1.0–1.23, 6–12 months, adjHR = 1.24, 95% CI 1.14–1.35).
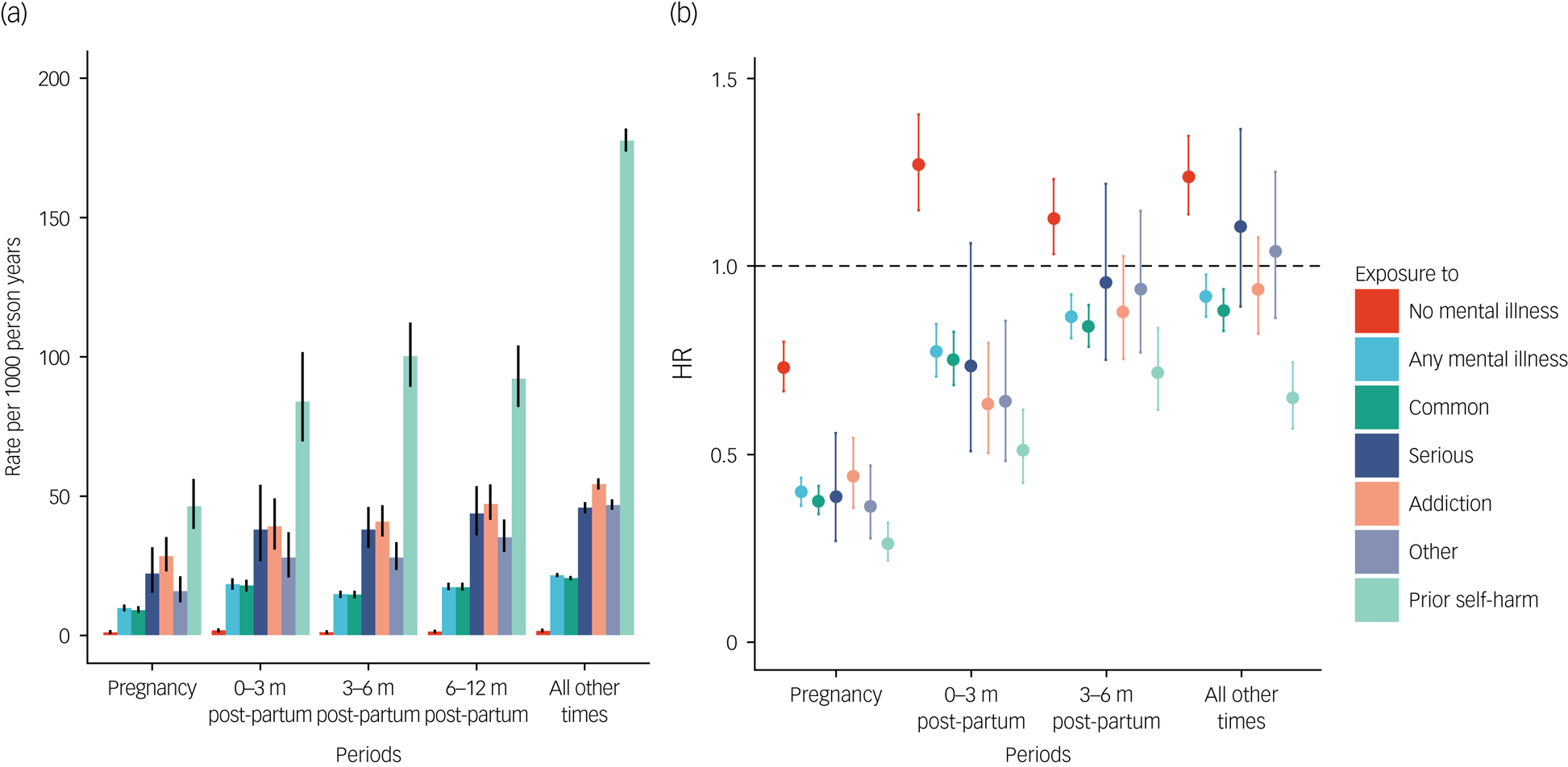
Fig. 1 The risk of self-harm in pregnancy and postpartum periods compared with any other time for women with and without mental illness. (a) Rate per 1000 person-years; (b) Hazard ratio. Whiskers indicate 95% CIs Adjusted for age, calendar year and region.
Is the risk of perinatal self-harm age-dependent?
For women aged 15–19 years, there was little evidence of a change in risk associated with pregnancy (7.56 v. 8.81 events per 1000 person-years, adjHR = 0.95, 95% CI 0.84–1.07). Women aged 30–34 years experienced the largest reduction in risk associated with pregnancy (0.86 v. 3.13 events per 1000 person-years, adjHR = 0.28, 95% CI 0.23–0.34) (Fig. 2). Postpartum, women aged 15–29 were at the highest risk of self-harm (for example at 3–6 months women aged 15–19 adjHR = 1.66, 95% CI 1.46–1.89, women aged 25–29 adjHR = 1.15, 95% CI = 1.02–1.28). There was little evidence of a postpartum increase in risk for women aged 35–39 and 40–45 years (see Supplementary Table 3 for values). Once mental illness was adjusted for, women aged 15–19 were less likely to self-harm in pregnancy (adjHR = 0.69, 95% CI 0.61–0.77). Sensitivity analyses revealed adjustment for mental illness had a less marked effect upon pregnancy risk of self-harm for women 25 years and older (see Supplementary Table 3).

Fig. 2 The risk of self-harm in pregnancy and postpartum periods compared with any other time for women by age of woman. (a) Rate per 1000 person-years; (b) Hazard ratio. Whiskers indicate 95% CIs. Adjusted for age, calendar year and region.
Is the risk of self-harm during postpartum independent of birth outcome?
Postpartum, women who experienced live births were at reduced risk of self-harm compared to all other times (Fig. 3(a)). For example, at 0–3 months there was a 60% reduction in risk after adjustment for calendar year, age and mental illness (adjHR = 0.40, 95% CI 0.34–0.47) (Fig. 3). By contrast, the risk of self-harm increased for women who experienced a miscarriage (0–3 months adjHR = 1.41, 95% CI 1.21–1.65) and the risk nearly doubled for periods following a termination (0–3 months adjHR = 1.93, 95% CI 1.72–2.17) (Supplementary Table 2).

Fig. 3 The risk of self-harm postpartum by birth outcome compared with pregnant and non-pregnant women. (a) Rate per 1000 person-years; (b) Hazard ratio. Whiskers indicate 95% CIs. Adjusted for age, calendar year and region.
Sensitivity analysis
When women who were never pregnant were excluded, the self-harm rate increased at times outside the perinatal period (rate 4.22 per 1000 person-years, 95% CI 4.17–4.27). This resulted in a slightly strengthened effect of pregnancy on self-harm risk relative to other times (HR = 0.47, 95% CI 0.44–0.50) and very weak evidence of an association in the period 6–12 months postpartum (HR = 1.02, 95% CI 0.97–1.07).
Discussion
This innovative study makes several important advances in our understanding of how pregnancy and the postpartum period affect self-harm risk. First, we demonstrate that the risk of self-harm halves during pregnancy for all women, but this reduction is not evident postpartum; and at 6–12 months after birth, there is a small increased risk. Second, although women with mental illness are more likely to self-harm than women without, their reduction in risk during pregnancy is greater than for women without mental illness. Furthermore, women with mental illness, unlike women without, continue to be at decreased risk of self-harm postpartum compared with any other time. Third, younger women and women who experience miscarriage or elective termination are more vulnerable to self-harm postpartum. In contrast, older pregnant women (30–45 years), or those who experience a live birth are at reduced risk of self-harm postpartum.
Research in context
This study strengthens and extends the existing evidence synthesised by Ayre et alReference Ayre, Gordon, Dutta, Hodsoll and Howard4 that the risk of self-harm is greatest for socioeconomically disadvantaged and younger women, and the risk is higher postnatally compared with pregnancy. This study quantifies the background risk of self-harm, which highlights the risk reduction in pregnancy, consistent with earlier studies that demonstrated pregnant women are less likely to die by suicide than other women.Reference Wallace, Hoyert, Williams and Mendola14 Our finding that mental illness is associated with self-harm generally is consistent with the existing evidence baseReference Ayre, Gordon, Dutta, Hodsoll and Howard4 and the finding that women with mental illness are less likely to self-harm in pregnancy contextualises the 8% rate of self-harm among pregnant women with psychotic disorders observed by Taylor et al,Reference Taylor, van Ravesteyn, van denBerg, Stewart and Howard15 suggesting self-harm may be lower in pregnancy even among high-risk groups. Overdose was the most common method of self-harm and the highest risk of self-harm was 6–12 months postpartum, reflecting recent data on US maternal deaths where mortality, commonly opioid overdose, peaked at 6–12 months.Reference Mangla, Hoffman, Trumpff, O'Grady and Monk16 Our findings replicate other large population studies of self-harm,Reference Morgan, Webb, Carr, Kontopantelis, Green and Chew-Graham6,Reference Carr, Ashcroft, Kontopantelis, Awenat, Cooper and Chew-Graham17 which report self-harm is increasing over time.
Women with a history of mental illness may be less likely to self-harm in pregnancy and postpartum for several reasons. First, the perinatal period may represent a period of relative wellness where women observe better self-care to protect themselves and their baby, potentially underpinned by hormonal changes during pregnancy intended to promote maternal attachment and increases a sense of well-being.Reference Carter, Altemus, Chrousos, Russell, Douglas, Windle and Ingram18 Second, antenatal and postnatal care contacts create more opportunities than at any other time to signpost women with mental illness to online and community sources of support or refer to a perinatal mental health service. In addition, women during the perinatal period are likely to have more social contacts and to feel less socially isolated than at other times, all of which might mitigate self-harm. The sensitivity analysis suggests young pregnant women with mental illness are not benefiting in the same way.
Clinical implications
Online training is available to mental health practitioners to support women with mental illness to plan pregnancy and provide them with resources and skills to prepare for motherhood.19 Midwife-led continuity of carer systems where women are given a named midwife from the start of pregnancy, who builds a trusting relationship with the mother and is the bridge to other services, does have some evidence of benefit for women who are at greater risk of self-harm.Reference Sandall, Soltani, Gates, Shennan and Devane20 Interventions that screen, refer and treat women remotely with trained professionals show promise at reaching women with mental illness who may feel particularly stigmatised and do not benefit from existing perinatal mental healthcare pathways.Reference Guille, Maldonado, Simpson, Newman, King and Cortese21 Such services might not only be of therapeutic value to the mother but may also improve the quality of parenting and health of the child. Younger women and those prescribed psychotropic medications commonly used in overdose should be monitored closely to reduce maternal deaths.
Family planning services that reduce the number of unwanted pregnancies and thus reduce miscarriages and terminations may also reduce self-harm risk, particularly among young women with mental illness. Women who become pregnant later in life, perhaps when they are more financially and mentally prepared for motherhood and have a supportive partner, do not experience an increased risk of self-harm postpartum.Reference Swift, Pierce, Hope, Osam and Abel7 This is not the case for young women; many of whom may lack important psychosocial advantages and are less likely to plan pregnancy.
Unplanned pregnancy may also be associated with other risks: Jackson et al recently reported that requests for emergency contraception were more likely in women with a history of domestic violence.Reference Jackson, Lewis, Feder, Whiting, Jones and Macleod22 Although we report an increased risk of self-harm in women with pregnancy loss after adjustment for mental illness, we do not recommend limiting women's access to termination. Women wanting termination reported that continuing with an unwanted pregnancy was worse for their mental health overall than having a termination.Reference Biggs, Upadhyay, McCulloch and Foster23 Easier access to psychological support may reduce the dual stigma associated with mental illness and termination that exacerbate some women's distress and increase self-harm risk.
Strengths and limitations
This represents the largest study using UK data to examine self-harm risk in pregnancy. A recurrent-event survival model holds several advantages over other approaches. The survival analysis framework and the use of the Cox model allowed for the non-parametric adjustment of time and for flexible splitting of study time (for example, into different postpartum periods). Incorporating repeated events in the survival model was considered optimal over analyses of the first event because the relationship between pregnancy and self-harm may evolve over repeated self-harm events. Stratification by the number of prior events accounted for non-independence, but this reduces sample size in each strata. Post hoc, we repeated the analyses using a frailty survival model that accounted for non-independence by including a random effect representing self-harm risk for each woman and results were similar (not presented). Unfortunately, we were unable to include ethnicity, because of the proportion of missing (~60%) data. Black and minority ethnic (BME) women are at higher risk of infertility, poorer pregnancy outcomes and maternal mortalityReference Knight, Bunch, Tuffnell, Jayakody, Shakespeare and Kotnis2 and self-harm, particularly Black British women aged 16–34 years.Reference Cooper, Murphy, Webb, Hawton, Bergen and Waters24 Future research needs to address if the increased self-harm risk postpartum is greater for BME women.
The potential underreporting of self-harm in primary care is a second limitation. If the general practice is not the first healthcare contact the acute service provider needs to share this information. A prior analysis from 2013 indicated that only 68.4% of self-harm events recorded in hospital settings are also recorded in primary care,Reference Thomas, Davies, Metcalfe, Windmeijer, Martin and Gunnell25 although this may have improved. Although hospital and emergency department presentations for self-harm represent a minority of events seen in primary care,Reference Ayre, Gordon, Dutta, Hodsoll and Howard4 these admissions might be more severe and, as a consequence, less likely to be underreported in pregnancy because they are harder to conceal.
Future research that scrutinises health records to identify indicators of unwanted pregnancy and challenging social circumstances as well as mental illness may provide better awareness about this vulnerable group and identify those most at risk who require targeted support.
In conclusion, women appear to be significantly less likely to self-harm during pregnancy, especially women with mental illness. Notably, adolescent pregnant women continue to self-harm in pregnancy and women aged 15–29 experience their highest risk of self-harm postpartum. Resources that support young mothers and their families need to be protected in the longer term.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1192/bjp.2022.31.
Data availability
Read codes used are published on Clinicalcodes.org. Electronic health records are, by definition, considered ‘sensitive’ data in the UK by the Data Protection Act and cannot be shared via public deposition because of information governance restriction in place to protect patient confidentiality. Access to data are available only once approval has been obtained through the individual constituent entities controlling access to the data. The primary care data can be requested via application to the Clinical Practice Research Datalink (www.cprd.com/researcher), secondary care data can be requested via application to the hospital episode statistics from the UK Health and Social Care Information Centre (www.hscic.gov.uk/hesdata).
Author contributions
H.H. and K.M.A. conceived of the study, M.P., K.M.A. and H.H. contributed to the acquisition of the data. H.H. designed the analysis, with input from all other authors. H.H. carried out the analysis and interpreted the data with contributions from all other authors. C.S.O. visualised the data. H.H. wrote the initial draft of the manuscript with input from K.M.A. All authors contributed to the final version, revising it for critically important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This project has received funding from the European Research Council under the European Union's Horizon 2020 research and innovation programme (grant agreement No GA682741), and the National Institute for Health Research (ref: 111905).
The funders had no role in the design, analysis or reporting of the study.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.