Introduction
Diabetes mellitus is one of the leading causes of mortality and causes severe complications, including stroke, myocardial infarction, chronic kidney disease and amputation due to diabetes foot (Stratton et al., Reference Stratton, Adler, Neil, Matthews, Manley, Cull, Hadden, Turner and Holman2000). Depression is also associated with increased mortality (Walker et al., Reference Walker, McGee and Druss2015) and medical complications (Katon, Reference Katon2003). Previous studies have demonstrated bidirectional associations between the incidence of depression and diabetes mellitus (Pan et al., Reference Pan, Lucas, Sun, van Dam, Franco, Manson, Willett, Ascherio and Hu2010; Chen et al., Reference Chen, Chan, Chen, Ko and Li2013). Depressive disorders increase the risk of new-onset diabetes mellitus. However, patients with diabetes mellitus also have higher likelihood of developing depressive symptoms. Furthermore, depression is associated with poor prognosis of cardiovascular diseases, cancer and surgical procedures (Pinquart and Duberstein, Reference Pinquart and Duberstein2010; Hare et al., Reference Hare, Toukhsati, Johansson and Jaarsma2013; Ghoneim and O'Hara, Reference Ghoneim and O'Hara2016).
Several studies have demonstrated that in patients with diabetes, depressive disorders are associated with poor glycemic control, although with a small effect size (Lustman et al., Reference Lustman, Anderson, Freedland, De Groot, Carney and Clouse2000). One meta-analysis demonstrated an association between depression and diabetes complications (De Groot et al., Reference De Groot, Anderson, Freedland, Clouse and Lustman2001); however, most included studies were cross-sectional, small-scale studies. Recently, several prospective studies have focused on the effects of depression on the risk of diabetes complications (Black et al., Reference Black, Markides and Ray2003; Orchard et al., Reference Orchard, Olson, Erbey, Williams, Forrest, Kinder, Ellis and Becker2003; Bruce et al., Reference Bruce, Davis, Starkstein and Davis2005; Egede et al., Reference Egede, Nietert and Zheng2005; Katon et al., Reference Katon, Rutter, Simon, Lin, Ludman, Ciechanowski, Kinder, Young and Von Korff2005; Richardson et al., Reference Richardson, Egede and Mueller2008; Lin et al., Reference Lin, Rutter, Katon, Heckbert, Ciechanowski, Oliver, Ludman, Young, Williams and McCulloch2010; Mai et al., Reference Mai, Holman, Sanfilippo, Emery and Preen2011; Pan et al., Reference Pan, Lucas, Sun, van Dam, Franco, Willett, Manson, Rexrode, Ascherio and Hu2011; Scherrer et al., Reference Scherrer, Garfield, Chrusciel, Hauptman, Carney, Freedland, Owen, True and Lustman2011; Sullivan et al., Reference Sullivan, O'connor, Feeney, Hire, Simmons, Raisch, Fine, Narayan, Ali and Katon2012; Ting et al., Reference Ting, Lau, Ozaki, Lau, Kong, Luk, Chow, Ma, Wing and Chan2013; Ismail et al., Reference Ismail, Moulton, Winkley, Pickup, Thomas, Sherwood, Stahl and Amiel2017). The results have been inconsistent. Most studies showed that baseline depressive symptoms or disorders were associated with increased risk of diabetes complications (Black et al., Reference Black, Markides and Ray2003; Orchard et al., Reference Orchard, Olson, Erbey, Williams, Forrest, Kinder, Ellis and Becker2003; Lin et al., Reference Lin, Rutter, Katon, Heckbert, Ciechanowski, Oliver, Ludman, Young, Williams and McCulloch2010; Mai et al., Reference Mai, Holman, Sanfilippo, Emery and Preen2011; Scherrer et al., Reference Scherrer, Garfield, Chrusciel, Hauptman, Carney, Freedland, Owen, True and Lustman2011; Ting et al., Reference Ting, Lau, Ozaki, Lau, Kong, Luk, Chow, Ma, Wing and Chan2013) or mortality (Egede et al., Reference Egede, Nietert and Zheng2005; Katon et al., Reference Katon, Rutter, Simon, Lin, Ludman, Ciechanowski, Kinder, Young and Von Korff2005; Mai et al., Reference Mai, Holman, Sanfilippo, Emery and Preen2011; Pan et al., Reference Pan, Lucas, Sun, van Dam, Franco, Willett, Manson, Rexrode, Ascherio and Hu2011; Scherrer et al., Reference Scherrer, Garfield, Chrusciel, Hauptman, Carney, Freedland, Owen, True and Lustman2011). Nevertheless, some studies showed a null association between depression and advanced microvascular complications (Sullivan et al., Reference Sullivan, O'connor, Feeney, Hire, Simmons, Raisch, Fine, Narayan, Ali and Katon2012; Ismail et al., Reference Ismail, Moulton, Winkley, Pickup, Thomas, Sherwood, Stahl and Amiel2017). Another study found that the association of depression with mortality might be confounded by underlying diabetes complications (Bruce et al., Reference Bruce, Davis, Starkstein and Davis2005). It should be noted that patients with depression have a longer duration of diabetes (Egede and Zheng, Reference Egede and Zheng2003) and a greater number of diabetes complications (Deschênes et al., Reference Deschênes, Burns, Pouwer and Schmitz2017). Most studies have included prevalent patients with diabetes; therefore, the temporal relationship between depression and diabetes complications is unclear. A recent review showed that a substantial proportion of studies failed to demonstrate that the outcome of interest was not present at baseline (Nouwen et al., Reference Nouwen, Adriaanse, van Dam, Iversen, Viechtbauer, Peyrot, Caramlau, Kokoszka, Kanc and de Groot2019). Only one study enrolled patients recently diagnosed with diabetes (Ismail et al., Reference Ismail, Moulton, Winkley, Pickup, Thomas, Sherwood, Stahl and Amiel2017); the findings showed that depression was only associated with macrovascular complications but not with worse glycemic control or increased risk of microvascular complications. However, the sample size in that study was moderate and the follow-up period was only 2 years.
In the present study, we used a nationally representative claims database to conduct a prospective matched cohort analysis to explore the association of depressive disorders with diabetes complications and related mortality. To eliminate confounding by the duration of illness and baseline complications, we only included incident patients with diabetes.
Method
Data source
In this study, we used Taiwan's National Health Insurance Research Database (NHIRD) (Bellows et al., Reference Bellows, LaFleur, Kamauu, Ginter, Forbush, Agbor, Supina, Hodgkins and DuVall2014). Taiwan launched its universal National Health Insurance (NHI) program on March 1, 1995, which covers 99% of the Taiwanese population. The NHIRD is derived from the original reimbursement claims and all identifiable personal information is anonymized. The database includes patients' demographic variables, clinical diagnoses, medical procedures and prescription records in outpatient, emergency department and inpatient settings. The accuracy of clinical diagnoses, such as depression, diabetes, stroke and acute coronary syndrome, has been well established (Lin et al., Reference Lin, Lai, Syu, Chang and Tseng2005; Wu et al., Reference Wu, Chan, Wu, Kuo, Wang, Tsao and Lin2010; Reference Wu, Kuo, Su, Wang and Dai2020; Cheng et al., Reference Cheng, Kao, Lin, Lee and Lai2011). The NHIRD has been widely used in psychiatric epidemiological studies and diabetes outcome research. This study was approved by the Internal Review Board of Human Studies of China Medical University Hospital.
Study population
Using the NHIRD, we identified incident patients with diabetes aged 20 years or more who were firstly prescribed antidiabetic agents and had at least a diagnosis of diabetes mellitus (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code: 250.x) between 2001 and 2014 (n = 1 864 089). Patients with type 1 diabetes mellitus were identified if their ICD-9 diagnostic code was 250.x1 or 250.x3 and they never used oral antidiabetic drug; the patients who remained were categorised into type 2 diabetes mellitus. The first date of antidiabetic prescription was defined as the cohort entry date. Given that some patients delayed treatment and had complications when diabetes was diagnosed, we excluded those with macro- or microvascular complications before or on the cohort entry date (n = 758 041). We did not include patients with a diagnosis of schizophrenia or bipolar disorders (n = 5664). In addition, those with information errors regarding sex, age or mortality date were also excluded (n = 13 259). The study population included 1 087 125 incident patients with diabetes.
Cohort of patients with diabetes who had depressive disorders
Incident patients with depressive disorder were those with at least two or more records with diagnosis of depressive disorders before the cohort entry date. The diagnostic code included major depressive disorder, recurrent episode (ICD-9 code: 296.3x); major depressive disorder, single episode (ICD-9 code: 296.2x); dysthymic disorder (ICD-9 code: 300.4) or depressive disorder not otherwise specified (ICD-9 code: 311). If a patient has two or more different diagnostic codes of depression, the types of depression were categorised based on the above-mentioned hierarchy. Finally, we identified a total of 38 537 patients with diabetes who had depressive disorders.
Comparison cohort of patients who had diabetes with no depressive disorders
We identified 154 148 eligible comparison participants with diabetes mellitus, who had no preexisting complications and no diagnosis of severe mental illnesses. For each patient with diabetes who had a depressive disorder, we randomly selected four comparison participants matched by age (year of birth), sex and the cohort entry year. The comparison participants were censored if they were diagnosed with a depressive disorder after the cohort entry date. The details of the selection procedure are shown in Fig. 1.
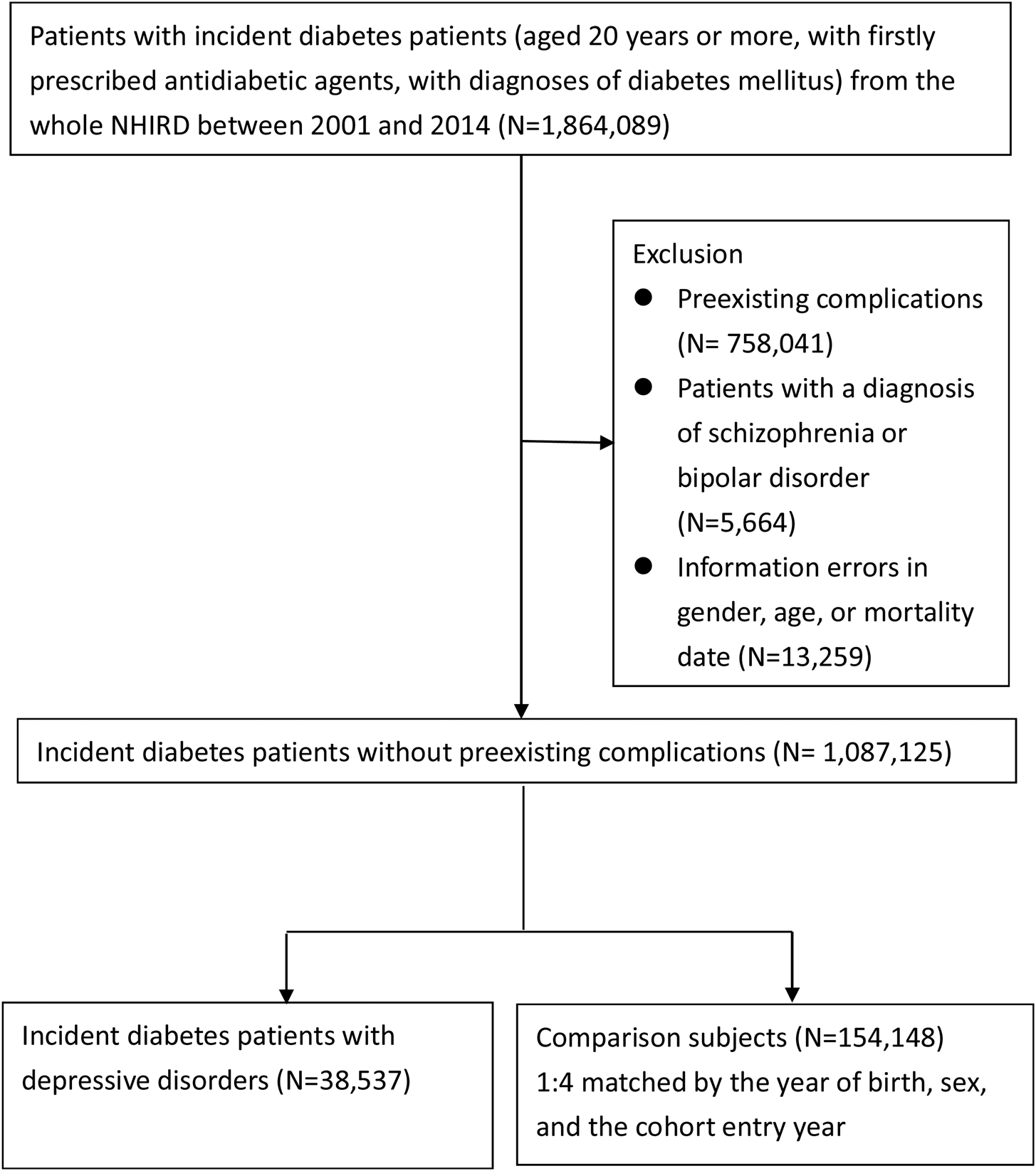
Fig. 1. Flow chart of selection of study population.
Main outcome measures
The study outcomes included macro- and microvascular diabetes complications, which were identified based on ICD-9-CM diagnostic and procedural codes and the NHI procedural codes from outpatient and inpatient claims records. Macrovascular complications included hospitalisation for acute coronary syndrome (ICD-9-CM: 410.x-411.x) and stroke (ICD-9-CM: 430.x-438.x). Validation of the inpatient diagnosis of the acute coronary syndrome and stroke has been well documented (Wu et al., Reference Wu, Chan, Wu, Kuo, Wang, Tsao and Lin2010; Cheng et al., Reference Cheng, Kao, Lin, Lee and Lai2011). Nevertheless, the accuracy of the diagnostic codes of microvascular complications remains unclear. Thus, we used a restricted definition, combining ambulatory diagnostic claims with procedural codes, or we used inpatient claims only, to ensure the accuracy of the diagnosis of microvascular complications. Microvascular complication was defined as the composite of diabetic retinopathy (ICD-9-CM: 250.5x, 362.01 or 362.02) with laser photocoagulation (NHI procedural code: 86 206B or 86207B) or vitrectomy (NHI procedural code: 60003C or 60004C), blindness (ICD-9-CM: 369.x), end-stage chronic kidney disease (ICD-9-CM: 585.5- 585.6 or 586) with dialysis, vessel operations for hemodialysis or kidney transplantation (ICD-9-CM: 39.27, 39.42, 39.43, 39.49, 39.50, 39.53, 39.93, 39.94, 39.95, 54.98 or 55.6x), hospitalisation for diabetic foot infection (ICD-9-CM: 681.1x, 682.6 or 682.7) or lower extremity amputation (ICD-9-CM procedural code: 84.1x).
Mortality information was obtained using Taiwan's National Death Registry. The cause-specific mortality included mortality due to cardiovascular disease (ICD-9: 390–459, ICD Tenth Revision (ICD-10): I00–I99) or diabetes (ICD-9: 250, ICD-10: E10-E14). To test the sensitivity of our methods, we included unnatural death (ICD-9: E800-E969, ICD-10: V, W, X or Y) and suicide (ICD-9: E950-E959, ICD-10: X60-X84 or Y87.0).
Covariate assessment
Patients' demographic variables included age, sex and the year of cohort entry. The duration between the first diagnosis of diabetes and the initiation of pharmacotherapy was also measured and categorised into <1 and ⩾1 year. Potential confounders, which were associated with both diabetes complications and depressive disorders, were assessed in the year preceding the cohort entry date, which included comorbid conditions of hypertension (ICD-9 code: 401.x-405.x), dyslipidemia (ICD-9 code: 272.x), chronic pulmonary disease (ICD-9 code: 491.x-494.x, 496.x), chronic liver disease (ICD-9 code: 517.2x, 517.5x, 517.6x, 517.8x, 517.9x, A347.x, 572.2x, 572.3x, 572.4x, 456.0x, 456.1x or 456.2x) and alcohol- and substance-related disorders (ICD-9 code: 291.x, 292.x, 303.x, 304.x, 305.x (except 305.1). In addition, medication use that reflected underlying medical conditions was assessed, including angiotensin-converting enzyme inhibitor (ACEI) and angiotensin receptor blocker (ARB) (ATC code: C09), beta blockers (ATC code: C07), calcium channel blockers (ATC code: C08), lipid-lowering agents (ATC code: C10) and nonsteroidal anti-inflammatory drugs (ATC code: M10).
Statistical analysis
We calculated the incidence of macro- and microvascular diabetes complications and mortality rates based on the event number divided by follow-up person-years. Multivariate Cox proportional hazards models were used with adjustment for the abovementioned confounders, to estimate the hazard ratios (HRs) of depressive disorders for the study outcomes. Subgroup analyses were conducted to evaluate whether the risks of depression for diabetes complications and mortality were modified by types of depression, age, sex and duration between diabetes diagnosis and initiation of pharmacotherapy.
The quality of diabetes care might be a mediator in the association of depression with diabetes complications and mortality; therefore, we did not include these variables in our model. We used post-hoc analyses to evaluate whether there were differences in the quality of diabetes care during the follow-up period between patients who had diabetes, with and without depressive disorder. Indicators of care quality included medication adherence for antidiabetic drugs, frequency of receiving blood sugar testing (HbA1c or fasting blood sugar), lipid profiles, serum creatinine, retina examinations and electrocardiograms during the follow-up period. Antidiabetic drug adherence was measured using the medication possession ratio (MPR), which was defined as the total days of prescribed antidiabetic medication supply divided by the follow-up period. Antidiabetic drug adherence was categorised as poor, irregular and good, based on the MPR (<0.2, 0.2–0.8 and ⩾0.8, respectively).
All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). The statistical significance of relationships was assessed using 95% confidence intervals (CI) or p values <0.05.
Results
There were 38 537 patients with diabetes who had depressive disorders and 154 148 patients with diabetes with no depressive disorders, as comparison participants. The average follow-up period was 5.5 years (ranging from 0 to 14 years). The mean (±SD) age of participants was 52.61 (±12.45) years, and 39.63% were male. Most of the patients have type 2 diabetes mellitus 99.4%. Among patients with depressive disorders, 26.21% had major depressive disorder, recurrent episode, 15.96% had major depressive disorder, single episode; 48.11% had dysthymia and 9.72% had depressive disorder, not otherwhere classified. Patients with diabetes who had depressive disorders had a higher proportion of comorbid conditions and medication use, except for ACEI/ARB use. The percentage of duration between diabetes diagnosis and initiation of pharmacotherapy ⩾1 year was 17% for patients with diabetes and depression and 24% for comparison subjects (see Table 1).
Table 1. Baseline characteristics (the year before entry)
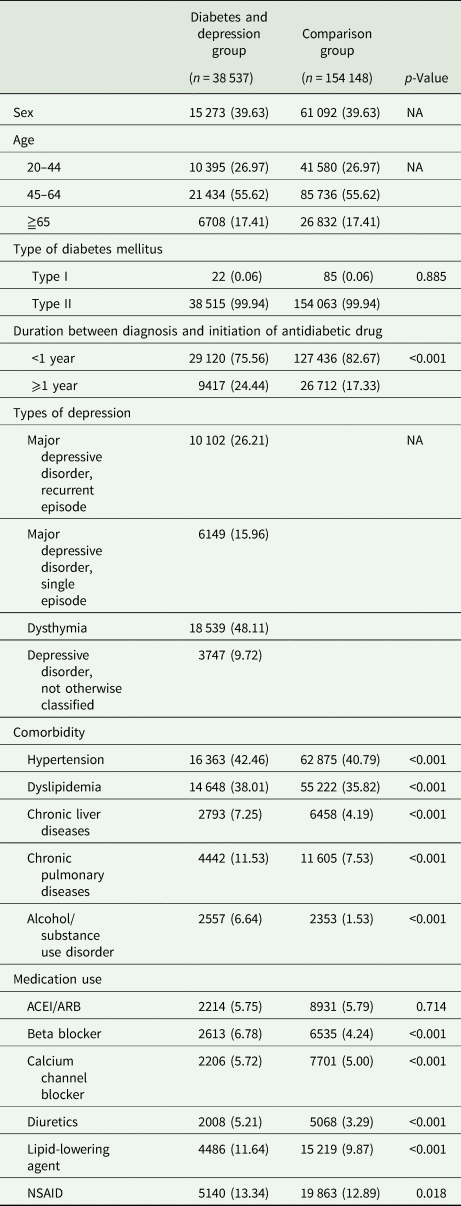
ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; NSAID, nonsteroidal anti-inflammatory drugs.
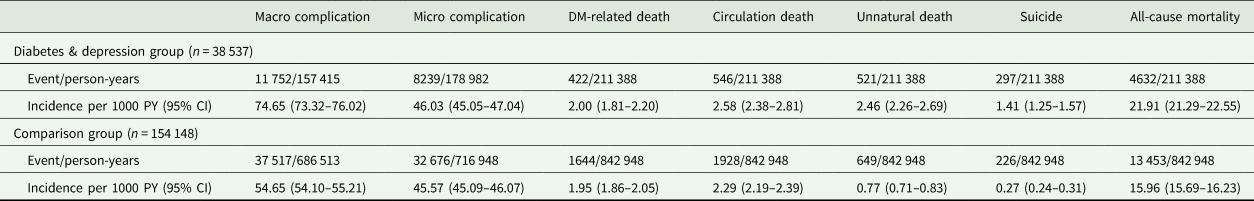
The crude incidence of macrovascular complications was 74.65 per 1000 person-years for patients with diabetes and depressive disorders; this was higher than the incidence (54.65 per 1000 person-years) for comparison participants. The same was true for the crude incidence of mortality due to cardiovascular diseases (2.58 v. 2.29 per 1000 person-years), unnatural mortality (2.46 v. 0.77 per 1000 person-years), suicide (1.41 v. 0.27 per 1000 persona-years) and all-cause mortality (21.91 v. 15.96 per 1000 person-years) between patients who had diabetes, with and without depressive disorders. However, there was no difference with respect to microvascular complications and mortality due to diabetes mellitus (see Table 2).
Table 2. Incidence of macro, micro, diabetes-related, circulation and all-cause mortality of the diabetes & depression group and comparison group
After adjusting for abovementioned covariates, we found that patients with diabetes who had depressive disorders had higher HRs for developing macrovascular complications (HR = 1.35; 95% CI 1.32–1.37), unnatural mortality (HR = 2.59; 95% CI 2.30–2.91), suicide (HR = 5.64; 95% CI 4.70–6.77) and all-cause mortality (HR = 1.08; 95% CI 1.04–1.12) than comparison participants. However, there was no statistically significant difference in microvascular complications and death owing to cardiovascular diseases. We found that depression was associated with a reduced risk of death owing to diabetes (Table 3).
Table 3. HRs for diabetes complications and mortality of the diabetes patients with and without depressive disorder, total and stratified by types of depression, gender, age and duration between diagnosis and initiation of pharmacotherapy

MDD, major depressive disorder; NOS, not otherwise specified.
In subgroup analyses, we found that the magnitude of associations with developing macrovascular complications, unnatural death, suicide and all-cause mortality was higher among those with major depression with recurrent episode than those with dysthymia or depressive disorder, not otherwise specified (the 95% CIs were not overlapping). In terms of the modifying effect of sex, we found that the associations between depression and developing macrovascular complications and unnatural mortality were stronger among women than among men. Otherwise, sex did not have a modifying effect on the incidence of microvascular complications and all-cause and other cause-specific mortality. In terms of age, there were effect modifications on diabetes complications and mortality. HRs in young adults (aged 20–44 years) with depressive disorders for all diabetes complications, all-cause mortality and all cause-specific mortality were higher than those among middle-aged (aged 45–64 years) and older (aged 65 years or more) adults. Furthermore, we found that duration between diabetes diagnosis and initiation of pharmacotherapy had a significant modifying effect on the associations with microvascular complications, diabetes-related death and all cause-mortality; the associations were stronger among patients with duration ⩾1 year than those with duration >1 year.
Assessment of the quality of diabetes care showed that patients with diabetes who had depressive disorders had slightly higher proportions of good antidiabetic compliance and higher rates of undergoing screening tests; however, the difference was quite small (Table 4).
Table 4. The quality of diabetes care among the diabetes patients with and without major depressive disorder

MPR, medication possession ratio.
Discussion
Main findings
In this study, we found that depression was associated with an increased risk of macrovascular complications, unnatural mortality, suicide and all-cause mortality among patients with incident diabetes mellitus. In contrast, there was no association between microvascular complications and mortality owing to diabetes mellitus and cardiovascular diseases. We found that age had a multiplicative effect modification on such associations. The magnitude of association was higher among young adults than middle-aged and older adults. Regarding the quality of care, we found that patients with diabetes who had depressive disorders had slightly better antidiabetic medication compliance and a slightly higher proportion of undergoing screening tests.
Comparison with other studies
The findings of a positive association between depression and macrovascular complications were consistent with those of several previous studies (Black et al., Reference Black, Markides and Ray2003; Lin et al., Reference Lin, Rutter, Katon, Heckbert, Ciechanowski, Oliver, Ludman, Young, Williams and McCulloch2010; Mai et al., Reference Mai, Holman, Sanfilippo, Emery and Preen2011; Scherrer et al., Reference Scherrer, Garfield, Chrusciel, Hauptman, Carney, Freedland, Owen, True and Lustman2011; Ting et al., Reference Ting, Lau, Ozaki, Lau, Kong, Luk, Chow, Ma, Wing and Chan2013; Ismail et al., Reference Ismail, Moulton, Winkley, Pickup, Thomas, Sherwood, Stahl and Amiel2017; Nouwen et al., Reference Nouwen, Adriaanse, van Dam, Iversen, Viechtbauer, Peyrot, Caramlau, Kokoszka, Kanc and de Groot2019). The underlying mechanism might be multifactorial. In patients with depressive disorder, associations were found between unhealthy lifestyle behaviours, such as tobacco smoking, physical inactivity or unhealthy diet (Deschênes et al., Reference Deschênes, Burns, Pouwer and Schmitz2017). Although we could not directly measure lifestyle behaviours in this study, we found that patients with depression had a higher prevalence of dyslipidemia, alcohol- or substance-related disorders and chronic pulmonary diseases, which are highly related to an unhealthy lifestyle. These unhealthy lifestyle behaviours are important contributors to macrovascular complications in patients with diabetes who have depression. In addition, depression itself might directly increase the risk of cardiovascular diseases (Joynt et al., Reference Joynt, Whellan and O'connor2003). Depression is linked to dysregulation of the hypothalamic–pituitary–adrenal axis, cardiac rhythm disturbances and systemic inflammation, which are also related to cardiovascular diseases (Joynt et al., Reference Joynt, Whellan and O'connor2003; Pariante, Reference Pariante2003).
We also found that depression was related to an increased all-cause mortality rate; however, the magnitude was smaller than that found in previous studies (Black et al., Reference Black, Markides and Ray2003; Egede et al., Reference Egede, Nietert and Zheng2005; Katon et al., Reference Katon, Rutter, Simon, Lin, Ludman, Ciechanowski, Kinder, Young and Von Korff2005; Mai et al., Reference Mai, Holman, Sanfilippo, Emery and Preen2011; Pan et al., Reference Pan, Lucas, Sun, van Dam, Franco, Willett, Manson, Rexrode, Ascherio and Hu2011; Scherrer et al., Reference Scherrer, Garfield, Chrusciel, Hauptman, Carney, Freedland, Owen, True and Lustman2011; Winkley et al., Reference Winkley, Sallis, Kariyawasam, Leelarathna, Chalder, Edmonds, Stahl and Ismail2012). In addition, we did not find an association of depression with death owing to cardiovascular diseases or diabetes mellitus. This finding was in contrast to those of earlier studies (Mai et al., Reference Mai, Holman, Sanfilippo, Emery and Preen2011; Pan et al., Reference Pan, Lucas, Sun, van Dam, Franco, Willett, Manson, Rexrode, Ascherio and Hu2011). Most previous studies included prevalent patients with diabetes who had a duration of illness of 5 years or more (Orchard et al., Reference Orchard, Olson, Erbey, Williams, Forrest, Kinder, Ellis and Becker2003; Egede et al., Reference Egede, Nietert and Zheng2005; Richardson et al., Reference Richardson, Egede and Mueller2008; Lin et al., Reference Lin, Rutter, Katon, Heckbert, Ciechanowski, Oliver, Ludman, Young, Williams and McCulloch2010; Pan et al., Reference Pan, Lucas, Sun, van Dam, Franco, Willett, Manson, Rexrode, Ascherio and Hu2011; Sullivan et al., Reference Sullivan, O'connor, Feeney, Hire, Simmons, Raisch, Fine, Narayan, Ali and Katon2012; Ting et al., Reference Ting, Lau, Ozaki, Lau, Kong, Luk, Chow, Ma, Wing and Chan2013); patients with depression might have had a longer duration of illness and more diabetes complications at baseline (Egede and Zheng, Reference Egede and Zheng2003). The associations between depression and mortality among patients with diabetes might be confounded by the duration of illness and pre-existing complications. One prospective study found that the effect of depression on mortality was no longer statistically significant after adjusting for macro- and microvascular complications (Bruce et al., Reference Bruce, Davis, Starkstein and Davis2005). In the present study, we included patients with incident diabetes mellitus and we excluded those who had diabetes complications. In addition, our study design eliminated confounding by the duration of illness and underlying complications. Furthermore, the average duration of diabetes was 5.5 years; therefore, the case number of death owing to cardiovascular diseases or diabetes mellitus might be small to have enough statistical power. Moreover, patients with untreated depression would be misclassified into comparison groups. It would introduce a bias towards the null. However, the bias would be small due to the low prevalence of depression (<2%) in Taiwan (Liao et al., Reference Liao, Chen, Lee, Lung, Lai, Liu, Lin, Yang and Chen2012).
We found there was no association between depression and microvascular complications. This finding was against several studies (Black et al., Reference Black, Markides and Ray2003; Lin et al., Reference Lin, Rutter, Katon, Heckbert, Ciechanowski, Oliver, Ludman, Young, Williams and McCulloch2010) and the recent meta-analysis (Nouwen et al., Reference Nouwen, Adriaanse, van Dam, Iversen, Viechtbauer, Peyrot, Caramlau, Kokoszka, Kanc and de Groot2019). Our result was compatible with that in a study conducted in the United Kingdom, which only included patients with a recent (<6 months) diagnosis of diabetes mellitus (Ismail et al., Reference Ismail, Moulton, Winkley, Pickup, Thomas, Sherwood, Stahl and Amiel2017); in that study, depression was not found to be associated with microvascular complications during the first 2 years of follow-up. Our study findings, with an average 5.5-year follow-up period (ranging from 0 to 14 years), further support the previous results. Glycemic control is a key factor related to the development of microvascular complications (UK Prospective Diabetes Study (UKPDS) Group, 1998). Whether patients with depressive disorders have poorer glycemic control remains inconclusive. One meta-analysis demonstrated that patients with diabetes and depression have poor glycemic control; nevertheless, the effect size was small (<0.2) (Lustman et al., Reference Lustman, Anderson, Freedland, De Groot, Carney and Clouse2000). Several recent prospective studies have shown that patients with diabetes and depression have sugar levels that are comparable to those without depression (Bruce et al., Reference Bruce, Davis, Starkstein and Davis2005; Ismail et al., Reference Ismail, Moulton, Winkley, Pickup, Thomas, Sherwood, Stahl and Amiel2017). Although the status of glycemic control was not available in our study database, the indicators for quality of diabetes care, including medication adherence for antidiabetic agents and frequency of screening tests, were approximately equal between patients with and without depression. Thus, we believe that there is no marked difference in glycemic control, and therefore, in the risk of microvascular complications between these patient groups. The role of glycemic control is less influential in macrovascular complications (Skyler et al., Reference Skyler, Bergenstal, Bonow, Buse, Deedwania, Gale, Howard, Kirkman, Kosiborod, Reaven and Sherwin2009). Unhealthy lifestyle, hypertension, dyslipidemia and smoking play major roles in the development of cardiovascular diseases (American Diabetes Association, 2016). Therefore, the impact of depression on macrovascular complications might be more obvious than that on microvascular complications.
In the subgroup analysis, major depression with recurrent episodes had greater associations with macrovascular complications and all-cause mortality than mild depression. These severity-response relationships further support the hypothesis between depression and diabetes complications. In addition, we found that women had a greater risk for mortality and macrovascular complications associated with depression than men. Previous studies have shown that the effect of diabetes on the risk of coronary disease is significantly greater for women than men (Lee et al., Reference Lee, Cheung, Cape and Zinman2000). Thus, there might be a synergistic effect of depression, female sex and cardiometabolic factors on the risk of diabetes. We found that age carried a multiplicative effect modification. The risk of depression for diabetes complications and mortality was higher among young adults than among middle-aged and older adults. A possible explanation for these findings is that middle-aged or older adults have multiple risk factors for developing complications and mortality; therefore, the effect of depression was not as obvious as that for other risk factors. In contrast, depression might be one of the few risk factors among young adults; depression showed an obvious impact on the development of complications and mortality in our study. The longer duration between diabetes diagnosis and initiation of pharmacotherapy was associated with higher risks for microvascular complications, diabetes-related death and all-cause mortality among patients with depression. Patients with depression have poor lifestyle and difficulty to get benefit from non-pharmacotherapy of diabetes only. These findings might indicate antidiabetic treatment should start early if patients have depressive disorder.
Strengths and limitations
Several limitations should be considered in this study. First, we identified patients with depressive disorders based on claims records. However, some patients with depression were not diagnosed or treated and could be misclassified into the comparison group; therefore, it would introduce bias towards the null. The effect of depression on diabetes complications and mortality might be underestimated. The duration between the diagnosis of depression and diabetes mellitus was unknown; therefore, we could not explore the effect of duration of depression on the study association. Second, only a few patients with type 1 diabetes mellitus were included because the age of onset was generally before 20 years. Our findings could not be concluded for those with type 1 diabetes mellitus due to the limited statistical power. Third, the accuracy of the diagnosis of microvascular complications of diabetes was not yet validated in the NHIRD; however, we used procedural claims data to confirm ambulatory diagnostic codes, or we only used inpatient claims data to minimise the possibility of misclassification. Fourth, several important factors, such as smoking, body weight, exercise, diet control and family history of depression and/or diabetes are not available in the NHIRD. Although we tried to use chronic pulmonary disease, dyslipidemia, hypertension and alcohol or substance use disorders as proxy measures for smoking, obesity and unhealthy lifestyle behaviours, there were still residual confounding effects. Especially, the lifestyle behaviours are time-variant and would be influenced by depression; therefore, these factors need to be adjusted by advanced methodology (Fewell et al., Reference Fewell, Hernán, Wolfe, Tilling, Choi and Sterne2004). There is a genetic overlap between depression and type 2 diabetes (Kan et al., Reference Kan, Pedersen, Christensen, Bornstein, Licinio, MacCabe, Ismail and Rijsdijk2016). The role of the shared genetic architecture on the associations between depression and diabetes complications needs further exploration. Finally, we did not investigate the treatment of depression. The antidepressant exposure might vary and interact with depression severity over the follow-up period; therefore, the association between antidepressant and diabetes complications could not be explored accurately using the current study design. The effect of antidepressant treatment on diabetes complications and mortality warrants further investigations.
The strengths of this study are the novelty of analysing the associations between depression and diabetes complications among incident patients with diabetes, the elimination of confounding by duration of illness and pre-existing complications, the use of a nationwide representative cohort with clear temporal relationships, a very large sample and a well-defined method for identifying complications of diabetes.
Conclusions
In conclusions, we found that patients with diabetes mellitus had a higher rate of macrovascular complications and all-cause mortality when they had comorbid depressive disorders. However, we found a lower adverse effect of depression than the findings of previous studies. This might be owing to the inclusion in our study sample of only incident patients with diabetes, thereby eliminating confounding owing to the duration of illness and preexisting complications. Depression is a modifiable risk factor of diabetes outcome. Further research should focus on evaluating the effect of depression treatment on advanced complications and mortality among patients with diabetes mellitus.
Availability of data and materials
The NHIRD used in this study is held by the Taiwan Ministry of Health and Welfare. Any researcher interested in accessing the data set can submit an application form to the Ministry of Health and Welfare requesting access, and we are not permitted to share the data.
Acknowledgements
None
Author contributions
Conception and design of the study: CSW and SHW. Analysis and interpretation of study data: CSW, LYH and SHW. Wrote first draft of the paper: CSW. Critiqued the output for important intellectual content: CSW and SHW. Approved the final article: CSW, LYH and SHW.
Financial support
This study was supported by research grants from the Ministry of Science and Technology (MOST 104-2321-B-039-007-MY3 to S.-H.W.; MOST 107-2314-B-002-216 to C.-S.W.). The funding agency had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflicts of interest
None.






