I Introduction
On June 2, 2016, the Center for Strategic and International Studies Global Health Policy Center in Washington, DC hosted a conversation with Jim Yong Kim, then president of the World Bank Group. Kim’s talk was entitled “Preventing the Next Pandemic.” Framed by the Ebola crisis that was just winding down in West Africa, pandemics in 2016 were presented as primarily a problem for developing countries. In his introductory remarks, the Center for Strategic and International Studies moderator, J. Stephen Morrison, even felt it necessary to remind the audience that understanding pandemics “mattered” for “US national interests.”Footnote 2 The primary pandemic-prevention mechanism proposed by the World Bank was emergency pandemic financing and insurance. In his remarks, however, Jim Yong Kim also argued that health was central to more than just national well-being: it was a key driver of economic growth and development. He cited findings from the Lancet Commission Report that, between 2000 and 2011, about 24 percent of income growth in developing countries resulted from improvements in health.Footnote 3
Kim’s position reflected what is sometimes called the “Post-Washington Consensus,” or the conclusion that development strategies should emphasize a broad array of social policies beyond what had been originally emphasized by the “Washington Consensus” of the 1980s and 1990s. The originator of the Washington Consensus, John Williamson, suggested that public expenditure priorities be redirected toward “neglected fields” such as “primary health and education, and infrastructure.”Footnote 4 Nevertheless, scholars generally agree that the Washington Consensus was characterized by a dominant orthodoxy that countries should “stabilize, privatize, and liberalize.”Footnote 5 When the Post-Washington Consensus was proposed in the mid-2000s, health again emerged as an area scholars saw as key for development,Footnote 6 though, as evidenced by Kim’s suggestions regarding pandemic insurance and financing, market-forward solutions are still seen as central, reflecting an international trend toward leveraging financial markets for development that some have dubbed the “Wall Street Consensus.”Footnote 7
Health will undoubtedly be central to any emerging global development consensus, but as the COVID-19 pandemic has made clear, a broader global consensus on public health, including the vision of society informing the concept of “the public,” is needed. In this chapter, we use data from the World Bank and other (Post-)Washington Consensus institutions to create a snapshot of global public health on the eve of the COVID-19 pandemic. We find that (Post-)Washington Consensus institutions saw the world as having varying levels of public-health-related development and social priorities. We then examine how countries from different clusters in this space fared in the early stages of the COVID-19 pandemic (in other words, before vaccinations became available in at least a few countries). We find that the countries supposedly best prepared for a public health emergency had no systematic advantage and even lagged behind countries that were supposedly not as well prepared in the early stages of the pandemic. Similarly, other classifications of public health preparedness from the pre-COVID-19 period, such as the World Health Organization’s Joint External Evaluation Tool or the Global Health Security Index, which did not adequately predict detection time and mortality in the early months of the COVID-19 pandemic, also fell short.Footnote 8 From our data and case studies, we are concerned that a tradeoff between democracy and government effectiveness may be a lesson taken from experiences in the early stages of the COVID-19 pandemic and suggest instead that a social democratic perspective on public health that links justice and efficacy is needed.
II Creating a Typology of Public Health Regimes
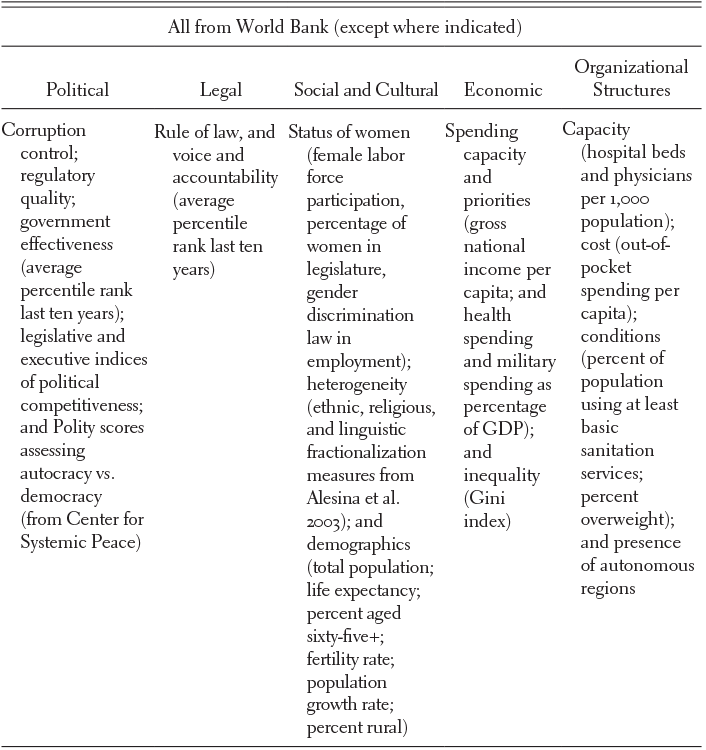
To create a typology of public health regimes that characterizes the variation in national public health on the eve of the COVID-19 pandemic from the perspective of institutions such as the World Bank, we group countries by similarity in “political, legal, social, cultural, economic, and organizational structures” related to public health.Footnote 9 While Asthana and Halliday emphasize that scholars can tailor public health regimes to study particular areas, such as nutritional inequalities or anti-smoking campaigns, we look broadly to see whether grouping countries by general indicators of public health can help us understand performance in response to the early stages of the COVID-19 pandemic. Our indicators of public health-related factors come primarily from World Bank and United Nations data, with two additional indicators of democracy, using the 2018 POLITY5 scores,Footnote 10 and ethnic and linguistic fractionalization, from measures developed by Alesina et al. in 2003.Footnote 11 Table 22.1 below shows the full set of indicators.
Table 22.1 Global indicators of public health
| All from World Bank (except where indicated) | ||||
|---|---|---|---|---|
| Political | Legal | Social and Cultural | Economic | Organizational Structures |
| Corruption control; regulatory quality; government effectiveness (average percentile rank last ten years); legislative and executive indices of political competitiveness; and Polity scores assessing autocracy vs. democracy (from Center for Systemic Peace) | Rule of law, and voice and accountability (average percentile rank last ten years) | Status of women (female labor force participation, percentage of women in legislature, gender discrimination law in employment); heterogeneity (ethnic, religious, and linguistic fractionalization measures from Alesina et al. 2003); and demographics (total population; life expectancy; percent aged sixty-five+; fertility rate; population growth rate; percent rural) | Spending capacity and priorities (gross national income per capita; and health spending and military spending as percentage of GDP); and inequality (Gini index) | Capacity (hospital beds and physicians per 1,000 population); cost (out-of-pocket spending per capita); conditions (percent of population using at least basic sanitation services; percent overweight); and presence of autonomous regions |
When conducting a global analysis, choices of indicators are limited to what is widely available and reliably measured. This limits what we can choose to explore and has theoretical implications because existing data do not come into existence by chance. Our analysis relies primarily on World Bank data, which, we argue, are indicators of a weak “Post-Washington Consensus” in public health.
These indicators arise from a contested paradigm. The Washington Consensus of the 1980s and 1990s on effective development strategies was associated with Washington-based policy institutions with strong international influence – such as the International Monetary Fund, the World Bank, and the US Treasury – which were proponents of neoliberal development policy.Footnote 12 Before the mid-2000s, when a spate of studies called its effectiveness into question, the Washington Consensus represented the dominant ideology in the area of development.Footnote 13 Though there have been numerous efforts to move beyond the Washington Consensus, such as the Post-Washington Consensus, no new dominant ideology has taken hold.Footnote 14 As Joseph E. Stiglitz put it in 2008, “If there is a consensus today about what strategies are most likely to promote the development of the poorest countries in the world, it is this: there is no consensus except that the Washington Consensus did not provide the answer.”Footnote 15 Despite being a contested consensus, the (Post-)Washington Consensus still looms large in contemporary indicators such as those we draw upon in this chapter, understandings of concepts such as “governance,” and global targets such as the Sustainable Development Goals.Footnote 16
A Principal Component Analysis
Principal Component Analysis (PCA) is a statistical method used to project high-dimensional data into a lower-dimensional space while preserving as much variation as possible. The “principal components” uncovered by PCA are linear combinations of the indicators that define orthogonal axes of variation. Running PCA on our 116-country dataset reveals two main components (see the Methodological Appendix in this chapter for the methodological details). Figure 22.1 shows how countries map onto them.

Figure 22.1 PCA results
1 A Primary Component of “Development”
Countries’ scores on the primary component, accounting for 40.9 percent of the overall variance, are graphed along the x-axis in Figure 22.1. We interpret these scores as broad indicators of public health-related development in the context of a weak Post-Washington Consensus.
The primary component distinguishes between, on the one hand, nations with good governance, high levels of health infrastructure, a more elderly and urban population, higher income levels, and longer life expectancy, and, on the other hand, nations with lower indicators of good governance, lower levels of health infrastructure, a younger and more rural population, lower income levels, and shorter life expectancy. We describe this component in more detail in the Methodological Appendix.
2 A Secondary Component of “Social Priorities”
The second component, explaining 10.4 percent of the variation in the data, is characterized by political distinctions that, in linear combination, explain variation orthogonal to (independent of) the first component. Countries’ scores on the second component are graphed on the y-axis of Figure 22.1. We describe the secondary component as a measure of “social priorities” related to public health. The social priorities component is characterized by women’s position in society, military spending, and democracy. Countries that score low on social priorities, and cluster at the center bottom of Figure 22.1, have lower levels of women in the workforce, higher military spending, and lower levels of democracy compared to countries with higher scores. Again, we describe this component in more detail in the Methodological Appendix.
B K-Means Clustering to Identify Public Health Regimes
We apply a second statistical method, k-means clustering, to group the countries based on their similarities within our statistical space to define groups that we call public health regimes.
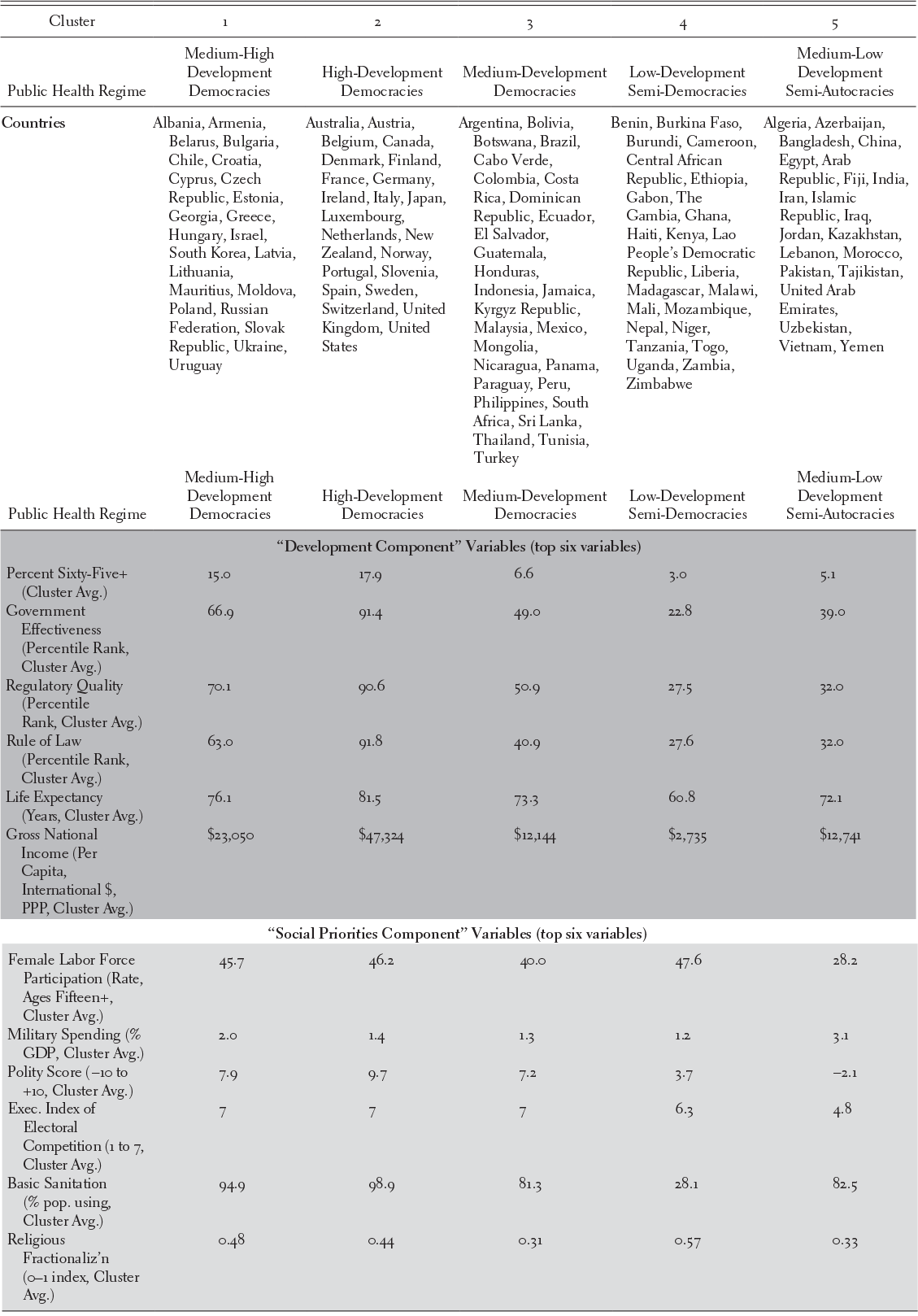
Theoretical motivation, certain statistical indicators, and face validity suggest that five clusters are optimal (see the Methodological Appendix). Figure 22.2 shows our clusters graphed over the first two components from the PCA. Table 22.2 summarizes the public health regimes that we find using five-cluster k-means.
Table 22.2 Public health regimes and key characteristics
| Cluster | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Public Health Regime | Medium-High Development Democracies | High-Development Democracies | Medium-Development Democracies | Low-Development Semi-Democracies | Medium-Low Development Semi-Autocracies |
| Countries | Albania, Armenia, Belarus, Bulgaria, Chile, Croatia, Cyprus, Czech Republic, Estonia, Georgia, Greece, Hungary, Israel, South Korea, Latvia, Lithuania, Mauritius, Moldova, Poland, Russian Federation, Slovak Republic, Ukraine, Uruguay | Australia, Austria, Belgium, Canada, Denmark, Finland, France, Germany, Ireland, Italy, Japan, Luxembourg, Netherlands, New Zealand, Norway, Portugal, Slovenia, Spain, Sweden, Switzerland, United Kingdom, United States | Argentina, Bolivia, Botswana, Brazil, Cabo Verde, Colombia, Costa Rica, Dominican Republic, Ecuador, El Salvador, Guatemala, Honduras, Indonesia, Jamaica, Kyrgyz Republic, Malaysia, Mexico, Mongolia, Nicaragua, Panama, Paraguay, Peru, Philippines, South Africa, Sri Lanka, Thailand, Tunisia, Turkey | Benin, Burkina Faso, Burundi, Cameroon, Central African Republic, Ethiopia, Gabon, The Gambia, Ghana, Haiti, Kenya, Lao People’s Democratic Republic, Liberia, Madagascar, Malawi, Mali, Mozambique, Nepal, Niger, Tanzania, Togo, Uganda, Zambia, Zimbabwe | Algeria, Azerbaijan, Bangladesh, China, Egypt, Arab Republic, Fiji, India, Iran, Islamic Republic, Iraq, Jordan, Kazakhstan, Lebanon, Morocco, Pakistan, Tajikistan, United Arab Emirates, Uzbekistan, Vietnam, Yemen |
| “Development Component” Variables (top six variables) | |||||
| Percent Sixty-Five+ (Cluster Avg.) | 15.0 | 17.9 | 6.6 | 3.0 | 5.1 |
| Government Effectiveness (Percentile Rank, Cluster Avg.) | 66.9 | 91.4 | 49.0 | 22.8 | 39.0 |
| Regulatory Quality (Percentile Rank, Cluster Avg.) | 70.1 | 90.6 | 50.9 | 27.5 | 32.0 |
| Rule of Law (Percentile Rank, Cluster Avg.) | 63.0 | 91.8 | 40.9 | 27.6 | 32.0 |
| Life Expectancy (Years, Cluster Avg.) | 76.1 | 81.5 | 73.3 | 60.8 | 72.1 |
| Gross National Income (Per Capita, International $, PPP, Cluster Avg.) | $23,050 | $47,324 | $12,144 | $2,735 | $12,741 |
| “Social Priorities Component” Variables (top six variables) | |||||
| Female Labor Force Participation (Rate, Ages Fifteen+, Cluster Avg.) | 45.7 | 46.2 | 40.0 | 47.6 | 28.2 |
| Military Spending (% GDP, Cluster Avg.) | 2.0 | 1.4 | 1.3 | 1.2 | 3.1 |
| Polity Score (−10 to +10, Cluster Avg.) | 7.9 | 9.7 | 7.2 | 3.7 | −2.1 |
| Exec. Index of Electoral Competition (1 to 7, Cluster Avg.) | 7 | 7 | 7 | 6.3 | 4.8 |
| Basic Sanitation (% pop. using, Cluster Avg.) | 94.9 | 98.9 | 81.3 | 28.1 | 82.5 |
| Religious Fractionaliz’n (0–1 index, Cluster Avg.) | 0.48 | 0.44 | 0.31 | 0.57 | 0.33 |

Figure 22.2 Five clusters – our selected grouping
III How Have Different Public Health Regimes Fared in the Context of COVID-19
We now examine how different public health regimes fared in the COVID-19 pandemic. We draw on data from the University of Oxford’s COVID-19 Government Response Tracker (OxCGRT),Footnote 17 for government response outcomes, and from Johns Hopkins University, for cases and deaths.Footnote 18 These datasets, while the most comprehensive data available at the time of writing, are not infallible. For example, in low- and middle-income countries, even during non-pandemic times, most deaths occur outside of the hospital system and are unlikely to have a cause-of-death certified by a physician.Footnote 19 Noh and Danuser find that in half of the fifty countries they explored, actual cumulative COVID-19 cases were estimated to be five to twenty times greater than the confirmed cases.Footnote 20
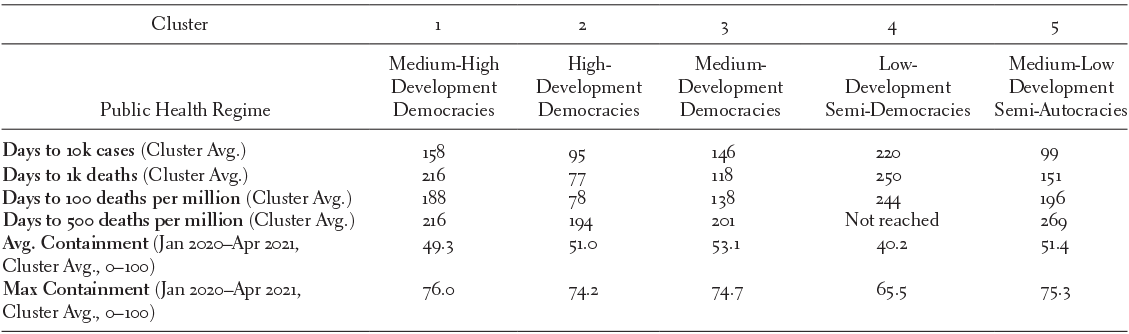
The first set of outcomes we examine is how fast COVID-19 spread and how comprehensive the government response was. We might expect a comprehensive response to slow the spread and variation in response and speed to vary across public health regimes we established in the previous section. Interestingly, neither pattern is borne out in the data.
In Figure 22.3, the x-axis indicates the number of days between the first and the 10,000th reported case in each country. The y-axis displays the maximum government containment score (0 to 100) over the period from January 1, 2020, and April 10, 2021, the maximum data window allowed at the time of analysis.Footnote 21 Maximum government containment comes from OxCGRT and includes the sum of fourteen indices from the areas of containment and closure policies (e.g., closing schools) and health system policies (e.g., public information campaigns) scaled to vary between 0 and 100. Taking a government’s maximum score on this metric produces a somewhat blunt measure of the initial COVID-19 response, but one that reflects the broad contours of important variation in government responses. In the Methodological Appendix, we show an alternative measure using the average government containment, which does not change the substantive results. The shape of the marker indicates the country’s cluster (public health regime).

Figure 22.3 Max government containment vs. speed of spread
Figure 22.3 and Table 22.3 indicate that none of the public health regimes we identified had a distinct advantage against COVID-19 in slowing the spread during the early phases of the pandemic. The High-Development Democracies (Cluster 2), which we would expect to be the best prepared, actually had the fastest spread, with only 95 days on average to reach 10,000 cases and 77 days on average to reach 1,000 deaths. While we might attribute the seemingly outstanding performance of the Low-Development Semi-Democracies (Cluster 4) to poor data quality, the fact that the High-Development Democracies did worse than Medium- and Medium-High-Development Democracies (Clusters 1 and 3), and even worse than Medium-Low-Development Semi-Autocracies (Cluster 5), is harder to attribute to data quality issues. This pattern persists even after accounting for population and examining the number of days to reach 100, then 500, deaths per million. Levels of containment were similar across all public health regimes, except for Low-Development Semi-Democracies (Cluster 4), which had somewhat lower average and maximum containment than other public health regimes.
Table 22.3 Public health regimes, speed of spread, government response
| Cluster | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Public Health Regime | Medium-High Development Democracies | High- Development Democracies | Medium- Development Democracies | Low- Development Semi-Democracies | Medium-Low Development Semi-Autocracies |
| Days to 10k cases (Cluster Avg.) | 158 | 95 | 146 | 220 | 99 |
| Days to 1k deaths (Cluster Avg.) | 216 | 77 | 118 | 250 | 151 |
| Days to 100 deaths per million (Cluster Avg.) | 188 | 78 | 138 | 244 | 196 |
| Days to 500 deaths per million (Cluster Avg.) | 216 | 194 | 201 | Not reached | 269 |
| Avg. Containment (Jan 2020–Apr 2021, Cluster Avg., 0 –100) | 49.3 | 51.0 | 53.1 | 40.2 | 51.4 |
| Max Containment (Jan 2020–Apr 2021, Cluster Avg., 0 –100) | 76.0 | 74.2 | 74.7 | 65.5 | 75.3 |
In sum, the High-Development Democracies of Cluster 2, those we expect would be best prepared, were likely to see a faster spread than countries with any other public health regime.
We might attribute some of this rapid spread to location, data quality, and demographics. However, examples from across the world highlight that these factors alone were not enough to determine a country’s destiny. For example, in Figure 22.3, Thailand stands out as a country that managed to slow the spread significantly despite geographical proximity to, and a close trade relationship with, China.
Figure 22.4 examines another factor that may have increased the challenge of containing COVID-19: the percentage of a country’s population aged sixty-five and older. For this analysis, we examine the number of days it took to reach the threshold of ten deaths per million. We see a negative relationship – countries with younger populations took somewhat longer to reach ten deaths per million – but there are some notable outliers, particularly South Korea, which has an older population, but was one of the slowest to reach the ten deaths per million threshold (260 days).

Figure 22.4 Percent sixty-five plus vs. days to reach 10 COVID-19 deaths per million population
In general, there is no strong correlation between what we identify as a country’s prior public health regime and its performance in the early stages of the COVID-19 pandemic. If anything, countries we might have expected to perform the best, those with the most consolidated democracies and higher levels of governance, income, and state capacity (the high-development democracies of Cluster 2), did worse in slowing the spread and lowering the death rate than countries in other clusters. In the face of the COVID-19 pandemic, the weak (Post-)Washington Consensus in public health is not indicative of less devastation even among its best students, just as the (Post-)Washington Consensus did little to stop the Great Recession of 2007–2009 from affecting wealthy countries around the globe.Footnote 22 Explaining this underperformance will take further analysis, but contributing factors may be demographics (as Cluster 2 countries tend to be older) and difficulty implementing non-pharmaceutical social interventions. We now conduct brief case studies to produce suggestions for key factors that we should be incorporating into our understanding of good public health.
IV Case Studies
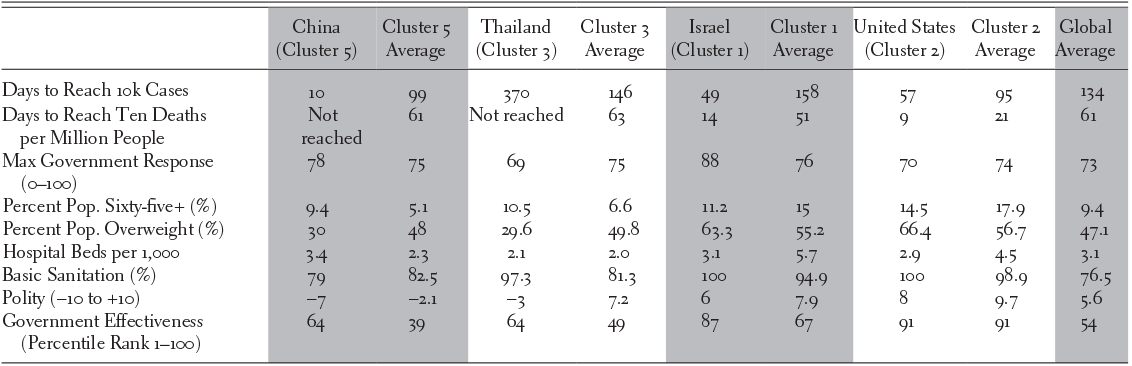
We chose to investigate China, Thailand, and Israel through brief case studies. China is unique on a global scale because of its large population and experience of coping with an emerging virus first. China is a Cluster 5 country (medium-low development semi-autocracy). Thailand is a Cluster 3 country (medium-development democracy), though it bucks the dominant trend of its group by being an autocracy with a Polity score of -3. Finally, Israel is a Cluster 1 country (medium-high-development democracy).Footnote 23 Table 22.4 shows comparative pandemic outcomes and selected background characteristics for each country relative to its cluster. The performances of these countries stand out in comparison to the poor performance of the United States and the other high-development countries of Cluster 2.
Table 22.4 China, Thailand, Israel, and United States pandemic outcomes
| China (Cluster 5) | Cluster 5 Average | Thailand (Cluster 3) | Cluster 3 Average | Israel (Cluster 1) | Cluster 1 Average | United States (Cluster 2) | Cluster 2 Average | Global Average | |
|---|---|---|---|---|---|---|---|---|---|
| Days to Reach 10k Cases | 10 | 99 | 370 | 146 | 49 | 158 | 57 | 95 | 134 |
| Days to Reach Ten Deaths per Million People | Not reached | 61 | Not reached | 63 | 14 | 51 | 9 | 21 | 61 |
| Max Government Response (0–100) | 78 | 75 | 69 | 75 | 88 | 76 | 70 | 74 | 73 |
| Percent Pop. Sixty-five+ (%) | 9.4 | 5.1 | 10.5 | 6.6 | 11.2 | 15 | 14.5 | 17.9 | 9.4 |
| Percent Pop. Overweight (%) | 30 | 48 | 29.6 | 49.8 | 63.3 | 55.2 | 66.4 | 56.7 | 47.1 |
| Hospital Beds per 1,000 | 3.4 | 2.3 | 2.1 | 2.0 | 3.1 | 5.7 | 2.9 | 4.5 | 3.1 |
| Basic Sanitation (%) | 79 | 82.5 | 97.3 | 81.3 | 100 | 94.9 | 100 | 98.9 | 76.5 |
| Polity (−10 to +10) | −7 | −2.1 | −3 | 7.2 | 6 | 7.9 | 8 | 9.7 | 5.6 |
| Government Effectiveness (Percentile Rank 1–100) | 64 | 39 | 64 | 49 | 87 | 67 | 91 | 91 | 54 |
A China
China, where the novel coronavirus originated, experienced rapid spread to 10,000 cases, but quickly controlled the disease, ultimately performing better than the rich democracies of Cluster 2. The effective Chinese response was facilitated by public health and industrial capacity, and by governmental and cultural factors.
After the first cases were reported in Wuhan in December 2019, lockdowns, school closures, and transport suspensions quickly followed. Coordination among government offices, extensive testing, and a national system of contact tracing facilitated the response, as did the early use of Fangcang hospitals to isolate mild-to-moderate cases from both homes and conventional hospitals. Although China has a large elderly population, only 3 percent live in nursing homes, minimizing one major source of infection experienced in some Western countries. Testing and quarantine measures for travelers aimed at preventing imported cases. China’s status as the world’s largest manufacturer of personal protective equipment also facilitated its reaction.Footnote 24
Among the public, “fresh memories” of the SARS-CoV outbreak hastened the response, as did ready compliance with mask wearing.Footnote 25 In general, the pandemic countermeasures were less fettered by concerns with civil liberties. “In China, you have a population that takes respiratory infections seriously and is willing to adopt non-pharmaceutical interventions, with a government that can put bigger constraints on individual freedoms than would be considered acceptable in most Western countries,” noted Gregory Poland, director of the Vaccine Research Group at the Mayo Clinic, adding that the response in the United States has been hampered by “hyper-individualism” and a “raucous anti-vaccine, anti-science movement that is trying to derail the fight against COVID-19.”Footnote 26 At the same time, the pace of vaccination was relatively slow because the country’s inactive-virus-based vaccine candidates took longer to manufacture, because millions of doses were donated to other nations to bolster foreign relations, and because, ironically, the effective response undercut urgency among the population, in contrast to the United States and United Kingdom, where raging infection rates spurred desperation over getting vaccinated.Footnote 27
B Thailand
Thailand illustrates the phenomenon of good governance without democracy, and its success in containing the pandemic is likely to reinforce calls for an emphasis on governance over democracy in the emerging public health consensus.Footnote 28
In March 2019, Thailand held elections for the first time since 2014, when a military coup overthrew its democratically elected government. Unfortunately, the 2019 election was widely considered to have been designed to prolong and legitimize the military’s dominant role in Thailand’s governance.Footnote 29 Between 1996 and 2018, Thailand’s ranking on the World Bank’s Worldwide Governance Indicators fell. Between 2002 and 2018, Thailand’s global rank decreased from the 65th percentile to below the 20th percentile for political stability, and from the 60th percentile to the 20th percentile for voice and accountability. However, government effectiveness remained relatively stable (around the 65th percentile). Kantamaturapoj et al. report that public services remain functioning with adequate quality, “reflecting a degree of independence from political pressure and a capacity to formulate and implement policies among bureaucrats.”Footnote 30
Since 2002, Thailand has provided comprehensive health benefits to its entire population through a universal coverage scheme with a high level of financial risk protection, as well as voice and accountability provided through legislative provisions and a deliberative process.Footnote 31 This health system was put to the test when, on January 13, 2020, Thailand was the first country to detect a case of COVID-19 outside of China.Footnote 32 After an initial spike in cases, Thailand went 102 days between May and September without any reported local transmission of COVID-19.Footnote 33
Thailand’s public health response to COVID-19 was swift and comprehensive. The Thai government quickly recommended the use of face masks and this was met with 95 percent compliance from the Thai population.Footnote 34 Tracing and quarantining were set up by rapid response teams, who isolated cases in facilities rather than in homes. When demand for N95 face masks spiked amid a global shortage, a new factory was constructed in a month, supplying free N95 masks to health facilities.Footnote 35 By the end of July 2020, a laboratory network for diagnosing COVID-19 using PCR (polymerase chain reaction) tests was active in 78 percent of Thailand’s seventy-seven provinces.Footnote 36
Although Thailand was successful in the initial stages of its response to the COVID-19 pandemic, Marome and Shaw raise concerns over the Thai government’s handling of the social and economic fallout from declining tourism revenue.Footnote 37
C Israel
Israel is one of the medium-high-development democracies that showed moderate success at COVID-19 containment during the initial months of the pandemic by utilizing centralized leadership. Inspired in part by a shortage of surge intensive care unit capacity, the Israeli Ministry of Health took control of hospital referrals and admissions and pioneered a containment strategy that included significant early travel restrictions and quarantine of travelers.Footnote 38 The Ministry of Health also took advantage of Israel’s strong digital health and surveillance capabilities to implement digital tracking, although this initiative was eventually struck down by the Israeli High Court of Justice as requiring legislative authorization rather than executive action.Footnote 39
There were also favorable demographic factors at play. Israel tends to be younger than other industrialized countries, such as those in Cluster 2, due to relatively high fertility rates.Footnote 40 Ethnic segregation may have also served as a protective factor for some communities, such as the Israeli Arab population, in the first wave of infection.Footnote 41
Interestingly, Israel’s strong centralized response to the pandemic and its emphasis on technology, including digital health, may ultimately allow it to be a COVID-19 “success story.” Then-Prime Minister Benjamin Netanyahu was able to secure a significant number of COVID-19 vaccine doses by, in part, promising a significant amount of data to manufacturers.Footnote 42 This promise was feasible because Israel had already created a national database that included the health information of 98 percent of its citizens. As a result, Israel may be the first country to immunize virtually all of its citizens over the age of sixteen and, therefore, potentially the first to control the pandemic via vaccination. Therefore, Israel may serve as a good reminder that this analysis considers the initial response and first wave of the pandemic, rather than the full life cycle of COVID-19.
V Discussion
The relative failure of the United States to slow the spread of COVID-19, along with the mediocre performance of high-development democracies in general, is continued evidence of the failure of the (Post-)Washington consensus in public health. As we look forward toward a still-hazy emerging public health paradigm, countries such as Thailand, South Korea, and Israel will likely become models that others will hope to emulate. For Israel and other similar success stories, we see a noteworthy pattern of above-average government effectiveness combined with below-average levels of democracy relative to their cluster peers.
The assumption that development and democracy are the sole predictors of pandemic preparedness and responsiveness has been challenged as agreement is emerging that Western countries have fared poorly. In an essay in the Intelligencer, “How the West Lost COVID-19,” David Wallace-Wells identifies slowness of response in the early stages of the pandemic amidst fear of how citizens might perceive rapid shutdowns as one major factor.Footnote 43 In the United States, for example, the first instinct of governments was to downplay the severity of the virus, while in East Asia, countries acted quickly and decisively despite incomplete information about the nature of the virus. This may in part be due to an arrogance that Western countries’ perceived development would shield them from the consequences of a pandemic. However, identifying precisely “how the West lost COVID-19” has been difficult. Multiple factors, including chance, contact with Italy, climate, and air conditioners, may all be at play. This is consistent with our analysis – no one set of indicators emerged as a reliable explanation for successes or failures in the early stages of the pandemic.
In noticing a tension between government effectiveness and democracy, we see a need for the future global consensus in public health to transition from a neoliberal vision of society to a social democratic one, in which the risks and costs associated with sickness are shared by the whole society, not only sick individuals, emphasizing that justice and efficiency must be linked together.Footnote 44 This linkage is desirable to avoid a world in which government effectiveness and democracy appear as tradeoffs, as they seem to be in our data, which arise from the neoliberal tradition embodied in the (Post-)Washington Consensus. In imagining the evolution of the Post-Washington Consensus in public health following COVID-19, we should cast off the centering on Washington and the neoliberal tradition that, in our analysis, fails to predict success in early pandemic responses. Instead, to prepare for the next global pandemic, we should focus more strongly on the connection between public health and democratic institutions, rather than government effectiveness in the abstract.