The war in Ukraine has been going on for more than 10 years, with intense escalation after a large-scale invasion in February 2022. Ukraine is the first state in the world to face such a phenomenon as the occupation of civilian nuclear facilities. In the period from February 24-March 31, 2022, the Exclusion Zone and the Zone of Unconditional (Mandatory) Resettlement of the Chornobyl Nuclear Power Plant (NPP) were occupied, incorporating many enterprises whose activities were being related to the management of spent nuclear fuel, radioactive waste, and sources of ionizing radiation. The elimination of the consequences of the occupation of the Exclusion Zone and the Chornobyl NPP continues to this day. Ukraine’s NPPs, like other nuclear power plants in the world, were not designed for operation in conditions of shelling, bombing, and other military operations. On March 4, 2022, Zaporizhzhia NPP was captured. The nuclear subcritical installation “Neutron Source,” located in Kharkiv, was destroyed.Reference Ruschak, Ivanko and Potapchuk1 On June 6, 2023, the destruction of the Kakhovka hydroelectric dam was committed by the Russian army, a war crime and potentially an act of ecocide. Thus, Ukraine’s health sector’s preparedness to respond to a nuclear disaster needs estimation.
Methods
In relation to the persisting unstable situation around Zaporizhzhia NPP located in the armed conflict zone and increasing concerns about the potential risk of use of nuclear weapons by Russian forces, the Ministry of Health (MOH) of Ukraine requested WHO’s assistance in strengthening national preparedness for a mass-casualty type of event related to a radio-nuclear hazard.
In addition, UN staff working in the field expressed concerns about their safety. While the UN Office for the Coordination of Humanitarian Affairs (OCHA) has distributed potassium iodide (KI) tablets to the staff, there was no technical expert on the ground to answer the staff’s questions on KI use and other protective measures. Prior to this deployment, on-line briefing sessions were held in August 2022 with the WHO Country Office (CO) and EURO staff to provide basic information on radiation risks and protective measures applied in radiation emergencies.
To address the concerns mentioned above, a 10-day mission of the WHO Head Quarter (HQ) specialist from the Radiation and Health Unit, Department of Environment, Climate Change, and Health, took place from September 20-30, 2022 with the following purpose:
-
- to review the current state of preparedness of the national health sector for a nuclear emergency;
-
- to identify areas of improvement and provide recommendations for strengthening the health sector’s capacity to respond to a nuclear emergency;
-
- to review the UN Department of Safety and Security (DSS) contingency plan for the safety of UN staff in the field and provide briefings for the staff in the field on matters related to radiation risk and radiation protection in case of a nuclear emergency.
Results
After the discussions during meetings with various stakeholders in Ukraine, the following findings were presented.
Duty of Care for WHO Staff
This included a UN DSS contingency plan (as reviewed and discussed with UN DSS, UN OCHA, and World Food Program (WFP) colleagues), a brief guide for radiation emergencies put together with short instructions for the WHO CO staff in the field.
National Preparedness Arrangements
Civil Protection Code2 guides the system of radiation emergency response; however, the relevant duties and responsibilities of various sectors/national agencies/stakeholders seem to be fragmented, overlapping, and without clear demarcation of roles and communication lines.
MOH has put in place 3 relevant orders: from April 6, 2022 No. 585 “On Approval of Methodological Recommendations for Actions in Nuclear Destruction Zones;” from April 11, 2022 No. 607 “On Approval of Methodological Recommendations for Organizing the Provision of Emergency Medical Assistance by Healthcare Institutions to Those Affected by the Action of Chemical, Biological, and Radiological Agents (Weapons of Mass Destruction);” and from March 9, 2021 No. 408 “Approved the Regulation on Iodine Prophylaxis in the Event of a Radiation Accident.” The overall national radiation emergency response plan was not available at the time of the mission.
The leading national response agency for radiation emergency response is the State Emergency Service of Ukraine (SESU), with its civil protection units and hydro-meteorological service. Special hazard units/teams within Civil Protection Service structures in all regions were said to have trained personnel and special equipment required for first response to radiation emergencies.
State Nuclear Regulatory Inspectorate of Ukraine (SNRIU) works with the national operator, Energoatom, on emergency response arrangements in the areas surrounding all NPPs in Ukraine within 30 km distance. These arrangements include off-site automatic monitoring of radiation levels in 30 km zones, air survey capabilities (with helicopters), provision on KI tablets, and sheltering and evacuation of residents of the nearest settlements. Specialized medical-sanitary facilities are also available at each NPP for nuclear workers and their families. These arrangements, so far, do not include environmental monitoring for areas outside the 30 km zones.
No formal agreements between health and other sectors were demonstrated, if they exist. Nevertheless, nuclear emergency exercises took place recently around Zaporizhzhia NPP with participation of relevant sectors/stakeholders. Routine monitoring of environmental radiation exposure and of planned exposures (workers, patients) is under the responsibility of regional Centers of Public Health under the Departments of Public Health (rDOH), which will collect information from 29 radiation monitoring laboratories at their Centers for Disease Control (rCDC) spread throughout the nation. These laboratories throughput capacities appear insufficient for providing systematic radiation monitoring (environmental and individual) in case of a nuclear emergency – both in terms of outdated and limited equipment and manpower.
All rDOH also include in their structure regional Centers for Disaster Medicine, which include special Units for Radiological Intelligence and Response. Nation-wide, more than 100 of such teams were set up, but only a small proportion of those underwent special training and received necessary equipment.
The responsibility for monitoring food and drinking water safety is with the Ministry of Consumer Protection and Trade, which was also told to have a very limited capacity for measuring radioactivity in samples (if any at all); no meetings were arranged with this sector.
In case of an accident not involving existing nuclear installation, SESU will be the first responder. They should be able to measure and identify the radiation type/isotope and map the perimeter of the affected area. SESU teams include paramedics and are reported to be equipped and trained to conduct rescue operations and bring out the wounded.
At the sorting area set up jointly by SESU and local law-enforcement staff, radiological and medical triage will be conducted. Radioactively contaminated persons will be directed to the mobile decontamination units and provided first aid, if needed. Those who need to be hospitalized will be taken to the designated hospital with an ambulance (emergency medical service, EMS). Those with life-threatening conditions may need to be stabilized and transported without decontamination.
It is not clear whether SESU teams will be able to identify life-threatening conditions at the point of the initial radiological and medical triage. Such conditions take priority over decontamination and would have to be transported immediately to a designated health facility. Therefore, health facilities will have to perform decontamination as well. In addition, patients self-presenting at hospitals would also need to be surveilled for radiation contamination and to be decontaminated. Arrangements for such activities are limited in hospitals which may be responding to a large-scale emergency.
The International Committee of the Red Cross (ICRC) informed that it has provided several mobile decontamination facilities to SESU and to some hospitals in the conflict-affected areas, but the number is very limited (no information on exact hospitals was provided).
After decontamination, a set of clean clothes and shoes should be provided. It is not clear who will be in charge of supplying these items in case of a mass casualty event, especially in wintertime; this must be addressed.
It is unclear whether there is a national stockpile for specific medical products for managing radiation injuries, as well as clinical protocols for diagnosis and clinical management of such patients.
The WHO Collaborating Center, the National Research Centre for Radiation Medicine, Hematology, and Oncology of the National Academy of Medical Sciences (NRCRM), has all the required technical expertise to support the development of national plans, procedures, and protocols for public health and medical response arrangements and provision of trainings, as well as accept up to 200 patients with radiation injuries. However, the role of the NRCRM does not seem to be incorporated into national response arrangements (possibly due to its belonging to the National Academy of Medical Sciences); the facilities and equipment of NRCRM are outdated and urgently need financial support.
In case national capacity is overwhelmed by the number of casualties, there are no arrangements for evacuating such patients abroad or getting foreign assistance.
There is ongoing work by WHO with the First Lady’s initiative on mental health and psychosocial support (MHPSS) in health emergencies. However, this work is not linked to the scenario of potential nuclear emergencies. It is not clear whether there are any arrangements for managing MHPSS in case of a nuclear emergency.
Recommendations
An overall, joint national plan for nuclear emergency response must be put in place (either revised or developed). We recommend setting up a technical advisory committee/council that will include representatives of national specialized institutions and organizations. This advisory body can provide technical support in devising a national response plan. According to the plan, clear roles and communication channels, as well as a cross-sector coordination role, should be established, including a crisis management center and public communications function.
Inventory and mapping of existing environmental and individual radiation monitoring, detecting, measuring, and dosimetry capacities of the health sector are needed. A decision-making tool/matrix/flowchart should be defined for the equipment use (where and when it is required) and arrangements put in place for transporting such equipment from unaffected to affected areas. These arrangements should be in line with and based on the national response plan. A detailed list of required equipment should be compiled and submitted to donors for procurement. Based on the result of such inventory and according to the roles in response, radiation monitoring and dosimetry devices are to be upgraded and provided to such designated facilities (rCDC, designated hospitals, and EMSs).
The responsibilities for emergency environmental monitoring and testing of food and drinking water must be clearly defined and assigned. Necessary equipment should be provided by the government to meet the systematic and high-throughput needs of such services, and staff should be trained to use such equipment. EMS staff/ambulances should be provided with standard operating procedures (SOPs) for the transportation of contaminated patients. Staff should be equipped with personal protective equipment (PPE), radiation detection devices, and large plastic sheets/covers to enable the transport of contaminated patients with life-threatening injuries. EMS staff should be provided training on handling contaminated patients. In each region, a secondary/tertiary health care facility can be designated to provide clinical management to persons with radiation injuries. Decontamination units should be provided to designated health facilities for patients self-presenting at the hospitals who may be contaminated. Emergency SOPs must be clearly defined for designated facilities, and staff should be trained in the use of such SOPs. Formal arrangements for the provision of clean clothes and shoes must be discussed with relevant actors and put in place in advance. Protocols can be provided for pre-hospital management of radiation injuries for EMS staff and hospital response, including clinical management. Training must be provided to the staff of EMS and designated hospitals on pre-clinical and clinical management of radiation injuries, radiation detection and decontamination procedures (including decontamination of wounds), and treatment of internal contamination with radionuclides. Access to pharmaceuticals is required for clinical management of radiation injuries (including cytokines, such as Filgrastim, and other medical products).
Automatic blood-cell counters should be available at all designed health care facilities (acute radiation syndrome patients require this several times per day to monitor bone marrow suppression evolution and adjust treatment). Intensive care/life support equipment and pharmaceutical supplies must be provided to designated tertiary hospitals. Arrangements must be made to access clinical care abroad for severe radiation injuries (MedEvac or other routes to be identified) in case national capacity is overwhelmed.
Linkages should be established with ongoing WHO CO work on managing the mental health impact of health emergencies and to ensure the use of preexisting resources and arrangements for nuclear emergencies. Simulation exercises for health authorities at regional levels should be planned and conducted, involving representatives of relevant authorities (SESU with meteorology and civil protection services, SNRIU, police, consumer protection, rCDCs, hospitals, and EMS) and WHO. The NRCRM should be incorporated into emergency response plans/arrangements, and its dosimetry and biodosimetry capacities should be upgraded and constitute a reference and resource center with unique expertise. Support for the NRCRM building renovation and heating problem should be provided. A donor for the NRCRM’s dosimetry laboratories should be identified, as these laboritories urgently require equipment upgrades.
Discussion
Based on joint discussion with WHO experts, the provision of radiation control equipment for units of 3 levels of medical response was considered: for Ambulance Teams (electronic personal dosimeters, passive dosimeters, portable dosimeters-radiometers); for Admissions Departments/Emergency Departments in designated hospitals and tertiary level hospitals (electronic personal dosimeters, passive dosimeters, portable dosimeters-radiometers, monitors for radioactive contamination of the surface of the human body with alpha and beta emitters, whole body counters); and for National and Regional Public Health Laboratories (electronic personal dosimeters, passive dosimeters, portable dosimeters-radiometers, multifunctional dosimeters-radiometers, devices for the identification of radionuclides, spectrometers). For the decontamination process and its organization in case of a mass casualty, the WHO procured 20 decontamination tents for the country.
During 2023 and at the beginning of 2024, the WHO purchased radiation control devices for medical institutions in Ukraine. In May 2024, this equipment was distributed under the WHO and the MOH recommendations. The needs analysis, procurement, and distribution of radiation detection and monitoring equipment are still being done in cooperation with the WHO Country Office.
At the same time, the NRCRM launched training courses for specialists of medical institutions of Ukraine located near the NPPs. These courses were aimed to improve the awareness of the health care sector of the nature of ionizing radiation, types of exposure, and health effects; Chornobyl lessons for the system of preparedness and response to a nuclear emergency; medical triage, prehospital, and hospital response; diagnosis and treatment of acute radiation syndrome; communication issues in radiation emergencies; and national and international recommendations for minimizing psychological impact in radiation emergencies.
The key international and national regulatory documents and guidelines were considered: the response to malevolent use of radiation,3 a checklist of hospital preparedness to radiation emergency,4 national stockpiles for radiological and nuclear emergencies,5 and management of radioactivity in drinking water.6
The lectures presented the experience of the NRCRM in organizing a system of individual dosimetric control and a sanitary pass in the Laboratory of Whole-Body Counters in the NRCRM. They outlined the basic principles, stages, and sequence of decontamination of contaminated persons. Personal experience in the work of the sanitary pass was presented as an example of the prompt response to emergencies and the effective operation of the system of individual monitoring of internal exposure of the personnel of the State Emergency Service of Ukraine, who had been involved in the elimination of a forest fire in the exclusion zone of the Chornobyl Nuclear Power Plant in April-May 2020 (480 persons). This experience proved that it was possible to monitor large groups of people affected by dangerous radiation situations and/or involved in their elimination, and to assess the value of the received individual effective dose of internal radiation from such a situation.
These lectures arouse the keen interest of the listeners, and many questions about the organization of the sanitary pass. During the practical study of the sanitary pass, the trainees go through all the stages of the examination. They have the opportunity to undergo an examination for surface contamination with radionuclides, organize rooms to accommodate contaminated clothes and stocks of clean clothes, and decontamination shower rooms. Finally, they familiarize themselves with and pass whole-body examinations on operational and expert control devices.
The largest number of questions were related to quite practical issues: the number of stocks of clean clothes, detergents for washing body and hair, where and how to transfer contaminated clothes, how to organize the collection of dirty water after decontamination, and so on.
Since the end of 2023, practical classes on methods of recording external and internal exposure have expanded significantly due to the need to acquire practical skills in working with devices that WHO purchased for medical institutions of the Ministry of Health of Ukraine (Figure 1).

Figure 1. Practice in individual dosimetry. Written consent was received for the publication of the identifiable images.
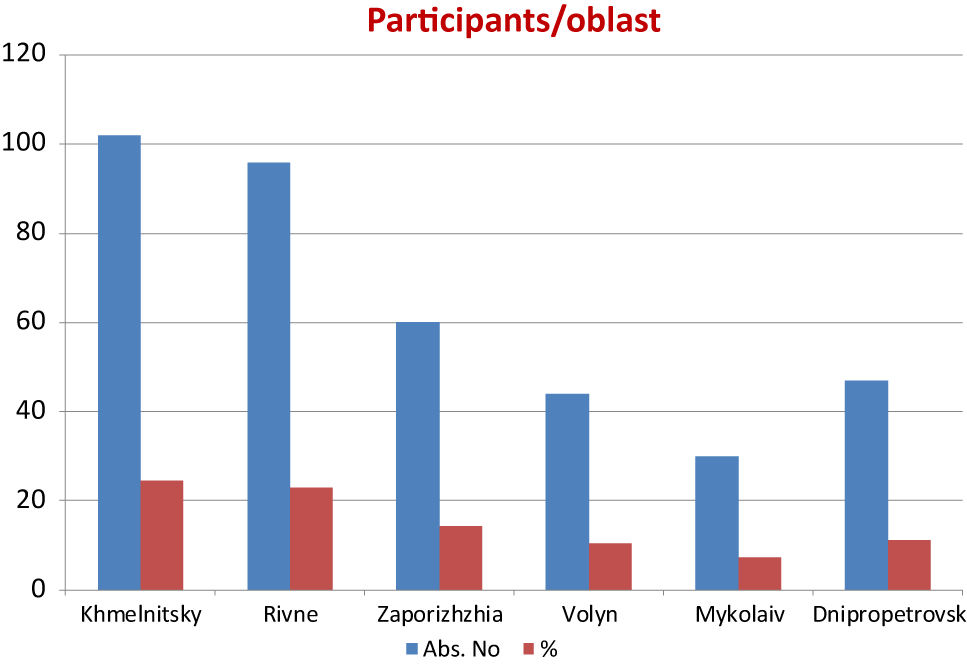
The WHO purchasing policy was oriented to domestic devices being in the register of measuring instruments of Ukraine, which means they will not have problems with metrological verification. The presence of a manufacturing company in the country guarantees quick maintenance and repair, if necessary. Foreign devices must go through the certification procedure, which takes time and significantly increases the already high prices of the really valuable devices. Thermo, Mirion, and Traserko were also purchased by WHO. In total, 377 health workers were trained in 2023-2024 (Figure 2).

Figure 2. Volumes of specialists of the Ministry of Health of Ukraine, who were trained at the National Research Center for Radiation Medicine, Hematology, and Oncology in 2023-2024.
Conclusions
-
1. The WHO mission was crucial in assessing the overall state of preparedness for CBRN threats and directing forces and resources to improve it.
-
2. Donor assistance in the form of equipment for dosimetric monitoring and diagnostics of emergency-related disorders contributes to improving the preparedness of the health system of Ukraine to an adequate response to the threats of radiation and nuclear emergencies
Competing interests
The authors do not declare any conflicts of interest.