Introduction
The Mental Health Commission (MHC) is the independent statutory regulator of mental health services in Ireland with a duty to promote high standards and good practices in the delivery of inpatient mental health services in approved centres (ACs) in Ireland. Registered proprietors of ACs are obliged to respond to MHC regulations and to any revisions to the Rules and Code of Practice regarding restrictive practices (RPs), by taking positive steps to ensure centres are in compliance. The Rules and Code form part of the inspection and monitoring framework and are inspected against at least annually.
This paper describes the continuing decline in RP use in ACs in Ireland and the acceleration of this trend in 2023 and 2024 following the revision by the MHC of its Rules and Code. The authors describe measures taken by the regulator and the registered proprietors of ACs to sustain this progress in inpatient mental health services in Ireland.
Methods
We examined anonymised data on RP within all ACs in 26 counties of Ireland as reported to the MHC via its revised Comprehensive Information System (CIS) over a two-year period 2023 and 2024. RP data are presented here for all 65 ACs combined and compared with those reported previously to the MHC between 2018 and 2022 inclusive. We describe total RP numbers and calculate RP rates per 1000 occupied bed days and per 100,000 members of the population. We then describe the actions taken by providers and the regulator to sustain this progress.
Results
Seclusion in ACs in Ireland in 2023 and 2024
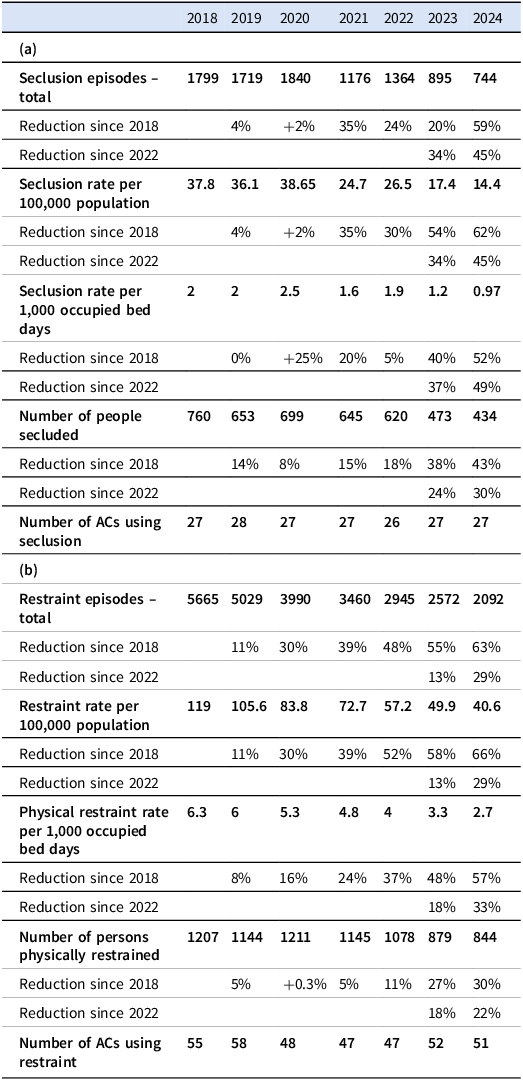
Twenty-seven ACs reported on their use of seclusion in 2023 and in 2024. The number of people secluded fell from 473 people in 2023, to 434 people secluded in 2024. Comparing these numbers to pre-2023 (the first year where the revised Rules were applicable), 2022 saw 620 people secluded (Table 1a). This equates to a 30% reduction in the number of people secluded in the period 2022 to 2024 and represents an acceleration of trends reported in the 5-year period 2018 to 2022 (when there was an 18% decrease in the number of people secluded; see Table 2).
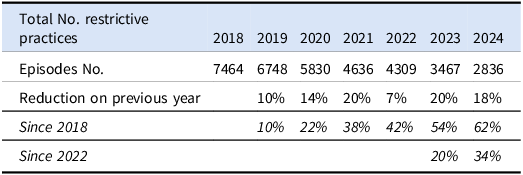
Table 1. Restrictive practice in approved centres (ACs) in Ireland 2018–2024. (a) Seclusion in ACs in Ireland – 2018–2024. (b) Physical restraint in ACs in Ireland – 2018–2024

Table 2. Restrictive practice (seclusion and physical restraint) in ACs in Ireland – 2018–2024

The total number of seclusion episodes also declined. In 2022, there were 1,364 episodes of seclusion in ACs in Ireland. In 2023, there were 895 seclusion episodes, and this fell to 744 seclusion episodes in 2024. This represents a 45% decrease in the number of seclusion episodes since the revised Rules came into effect.
The seclusion rate per 100,000 population declined from a rate of 26.5 per 100,000 population in 2022 to 17.4 in 2023 and to 14.4 in 2024 (Table 3a).
Table 3. (a) Seclusion and physical restraint in ACs in Ireland – RATE per 100,000 population. (b) Seclusion and physical restraint in ACs in Ireland – Rate per 1000 occupied bed days

The seclusion rate per 1,000 occupied bed days declined by 5% between 2018 and 2022 and by 49% between 2022 and 2024. For the first time, the seclusion rate per 1,000 occupied bed days was less than 1.
The profile of persons secluded did not change in 2023 and 2024. Figures for 2023 and 2024 reveal that males were more likely to be secluded (69.4%) than females (30.6%). The mean (± SD) age of those secluded was 36 (± 1) for both males and females. In 2023 and 2024 ethnicity was described as ‘White Irish’ in 76% of seclusion episodes. This is consistent with the profile of the inpatient hospital population in Ireland (Health Research Board 2024).
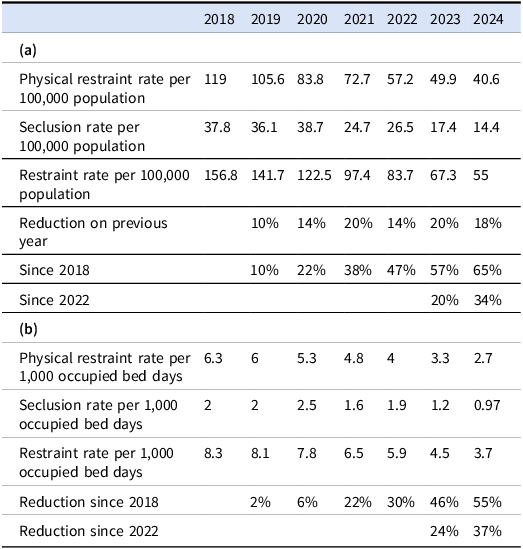
The majority of those secluded in 2023 and 2024 were involuntarily detained under the Mental Health Acts 2001–2018 (the “Act”) (64.4% and 77.7% respectively: Table 4a). It is permissible in Irish law (under the Act) to apply RPs to admitted persons who have not been detained under the legislation. The balance were patients admitted voluntarily, wards of court, and children held under Section 25 of the Act.
Table 4. (a) Legal status of persons at initiation of seclusion episode. (b) Legal status of persons at initiation of physical restraint episode

Physical Restraint (PR) in ACs in Ireland in 2023 and 2024
Fifty-two ACs reported on their use of physical restraint (PR) in 2023 and 51 did so in 2024.
In 2022 (the final year where the original Code was still applicable), there were 2,945 PR episodes involving 1,078 persons (Table 1b). The following year in 2023 there were 2,572 PR episodes (involving 879 persons). This fell to 2,092 episodes in 2024 (involving 844 persons).
PR episodes fell by 29% between 2022 and 2024. The number of people restrained in ACs in Ireland has fallen by 22% since 2022 and by 30% since 2018.
The PR rate per 100,000 population declined from 57.2 in 2022 to 49.9 in 2023, and to 40.6 in 2024. This demonstrates a fall of 29% in the rate per 100,000 population between 2022 and 2024, and a decrease of 66% since 2018.
The restraint rate per 1,000 occupied bed days fell by 57%, from a rate of 6.3 events per 1,000 occupied bed days in 2018 to 2.7 events per 1,000 occupied bed days in 2024 (i.e. for every 1,000 days a bed was occupied in 2024, PR was used 2.7 times: see Table 3b).
Five types of PR were reported (upright, supine, side, prone and other). Upright restraint fell from 1,090 episodes in 2023 to 882 episodes in 2024. Supine restraints fell from 428 episodes in 2023 to 269 episodes in 2024. Prone restraint (restraint with face down) fell from 411 episodes in 2023 to 194 episodes in 2024. This represents a reduction of 53% between 2023 and 2024. This decrease can be explained in part due to the MHC having the information in near real time to allow it to follow up with services with high rates of prone restraint.
Side restraints rose from 495 episodes in 2023 to 538 in 2024 and restraints described as ‘other’ also rose from 149 in 2023 to 209 in 2024.
The profile of persons restrained did not change in the years 2023 and 2024. Males were slightly more likely to be restrained than females in 2024 (M: F, 53.4%: 46.4%). The mean (± SD) age of persons restrained was 40 (±) 1 years and the ethnicity of 79.6% of people restrained in 2024 was described as ‘White Irish’.
Most individuals restrained in 2024 were involuntarily detained under the Act (68.3%: Table 4b). Others restrained included people admitted voluntarily (23.8%), people described as wards of court (2.2%), and children held under Section 25 of the Act (5.7%). The proportion of people with a voluntary legal status who were restrained between 2023 and 2024 was 33% and 23.8% respectively.
Duration of PR fell in the years 2023 and 2024. Most PR episodes (97.4% and 97.9%) were of a duration of ten minutes or less, and over three quarters (75.54% and 80.8% respectively) were for five minutes or less. The number of restraints lasting over 15 minutes has fallen from 271 restraints in 2022 to 31 in 2024. The total duration of PR across all ACs fell from 189 hours and 30 minutes in 2023 to 141 hours and 10 minutes in 2024. In both years, the median duration of PR was three minutes.
Physical Restraint (PR) and seclusion on children in ACs in Ireland in 2023 and 2024
Episodes of PR in child and adolescent (CAMHS) ACs fell by 53% between 2023 and 2024, with an 80% decrease in seclusion episodes between the same years. Since 2018 there has been a 91% reduction in the use of seclusion and physical restraint in CAMHS services, from 2,608 episodes in 2018 to 238 in 2024.
Discussion
There is increasing evidence that restrictive practices are counterproductive (Mental Health Commission 2022c). The MHC’s function is to promote, encourage and foster the establishment and maintenance of high standards and good practices in the delivery of mental health services and to take steps to protect the interests of persons detained under the Act.
The data presented here are indicative of substantial change in clinical practice in ACs in Ireland. Progress in human rights-based and trauma-informed care is manifest on inspection in adult ACs and in centres for the care of children with a mental health difficulty. It is appropriate at this stage to detail the steps taken by providers and by the MHC to sustain this progress.
Steps taken by the MHC and by service providers through the adoption of a human rights-based approach
The MHC commenced its review of RP Rules and Code in 2022 prompted by international developments in the understanding of human rights, advances in person-centred care, and evidence (Mental Health Commission 2022c) demonstrating harmful physical and psychological consequences of RPs. The MHC engaged in a process of consultation involving public surveys, focus groups, interviews with key stakeholders and an Expert Advisory Group which included experts by experience and staff working in ACs (Mental Health Commission 2022d).
The project team considered an in-depth evidence review commissioned by the MHC and undertaken by the Royal College of Surgeons Ireland following a tender process (Mental Health Commission 2022c). This review found compelling international evidence to show that seclusion and restraint have no therapeutic value and that they are not treatments. It found that RPs can be deleterious both physically and psychologically and concluded that their use increases the risk of trauma and may trigger symptoms of previous experiences of trauma and should only be used in rare and exceptional circumstances as an emergency measure.
Implementation of the revised rules and code
The MHC’s revised Rules and Code regarding restrictive interventions came into effect on 1 January 2023. These stipulate that ACs must recognise the inherent rights of each person to personal dignity and freedom in accordance with national and international human rights instruments and legislation. A human rights-based approach is one in which the principles of equality, respect and freedom from discrimination are central. Such an approach prioritises the dignity, autonomy and well-being of every service user.
Those who are restrained or secluded must be treated with dignity and respect at all times before, during, and after the episode of restraint/seclusion (Mental Health Commission 2022a; Mental Health Commission 2022b). Not all services users restricted are detained under the mental health acts. More than one fifth are voluntary but the principles of human rights and trauma-informed care underpin all care under the revised Rules and Code regardless of legal status.
The MHC introduced near real time reporting of RPs via the revised CIS. This enabled the MHC to follow up with centres with high RP rates. Whenever concerning trends are identified, services are contacted by the regulator to request assurances about their arrangements for compliance with the revised Rules and Code.
MHC regulatory interventions such as unannounced inspections, regulatory notices and compliance meetings continued as before throughout this period.
Restrictive practices on children
In 2023, the MHC decided to introduce an absolute prohibition on the use of mechanical restraint in children (for example the use of handcuffs). Children are particularly vulnerable to trauma and any harm resulting from restrictive interventions. Physical restraint of children and young people may only be used with extreme caution because in most cases their musculoskeletal systems are immature, and this elevates the risk of injury. Seclusion and physical restraint can have adverse implications for the emotional development of a child (Mental Health Commission 2022c).
Any AC considering the use of seclusion or physical restraint on a child must document a risk assessment on admission. This must be carried out by a registered medical practitioner or registered nurse and must show that careful consideration has been given to the potential effects of secluding or restraining a child, having regard to the physical status and emotional development of the child, and their particular vulnerability to trauma and harm as a result of restrictive interventions. The outcome of the risk assessment determines if seclusion or physical restraint can be safely used or not.
Response from ACs to the revised MHC rules and code
ACs throughout Ireland responded positively to these revisions in Rule and Code by amending their policies, introducing post incident reviews and enhancing staff training to support necessary changes in clinical practice. Centres maintain a Seclusion Register and a Physical Restraint Clinical Practice Form is completed after each event with a declaration as to why the person was restricted and a statement as to whether the person who was secluded or restrained was injured during the episode.
Policy development within ACs
New policies intended to reduce or, where possible, eliminate RPs were introduced by all ACs. RP reduction policies address leadership, the use of data to inform best practice, the use of specific reduction tools, the development of workforce competency, and the use of positive behavioural supports as means of reducing or, where possible eliminating, the use of RPs in the service.
Post incident reviews
Three distinct categories of post-incident review were adopted by ACs to inform on-going clinical practice. Firstly, a debrief with the person who has been secluded or restrained takes place following every episode. Secondly, the episode of seclusion or restraint is reviewed by members of the multidisciplinary team involved in the person’s care and treatment and thirdly, each AC is required to establish a multidisciplinary review and oversight committee to analyse in detail every episode of seclusion or restraint.
Each AC publishes non-identifiable aggregate data annually on their use of seclusion and restraint and places this on the registered proprietor’s website within six months of the end of the calendar year.
Training
ACs in Ireland ensure that all staff who participate, or may participate, in the use of seclusion or restraint receive the appropriate training. This includes training in trauma-informed care, human rights and in related policies and procedures. A record of attendance at training is maintained in the AC.
Strengths and limitations of this study
There are several possible explanations for reductions in restrictive practice. This study was not a randomised controlled study and did not have an experimental design. Consequently it is difficult to be certain as to the reasons for this welcome progress. On the other hand, the data were collected in near real time electronic fashion and they are consistent. The reductions cannot be dismissed as an artefact of admission rates or a consequence of differences in use of the Mental Health Acts. These factors and other regulatory practices mandated by the Mental Health Acts remained consistent and unchanged throughout the study period. Trends towards reduced restriction go back at least as far as 2018 and accelerated following changes described above.
It is reasonable to conclude that this demonstrable progress accelerated as a result of increased collaboration between regulator and providers. Extensive measures taken by regulator and provider are described above. These steps have delivered better training and improved therapeutic services and so restriction has become less frequent.
Other factors require study. Staffing numbers have fluctuated during this period (and they remain challenged) and the influence of substance misuse at a population level remains poorly understood. Overall use of psychotropic medications within ACs does not appear to have changed but greater consideration of prescribed medication is necessary to fully understand this progress.
Conclusion
The downward trend in the use of RPs, already noted in ACs in 2022 accelerated in 2023 and 2024 following the introduction of the revised Rules and Code and after the implementation of a timely notification system. The momentum of change towards less restrictive forms of care has increased. The rate of fall in seclusion episodes in 2023 and 2024 is almost twice that seen in the preceding four years. The rate of reduction in the number of people physically restrained is twice that seen in the preceding four years.
The number of people subject to RPs and the number of RP episodes has fallen. The duration of episodes has also reduced.
The MHC published previously on the declining use of RPs in ACs in Ireland over the period from 2018 to 2022 (Lucey et al. Reference Lucey, Kiernan, Farrelly, Downey and Stepala2024). Those data were collected before the revised Rules and Code came into force and before the requirement to notify the MHC using the CIS system within three working days. The data presented here confirm and extend these earlier findings.
The results presented here could not have been achieved without the enthusiastic participation of the leadership and staff in ACs throughout Ireland. RP reduction progressed following the successful introduction of policy initiatives in ACs and the reform of services offered to acutely distressed patients.
For the MHC, the task of standard setting and monitoring compliance is only a start. The continued delivery of high-quality care consistent with these standards depends on those at the care face and it is a credit to them. It is the MHC’s intention that this human rights approach will be applied more broadly to include all areas of mental healthcare.
The MHC acknowledges that restrictive practices take many forms, other than those which are covered by the Rules and Code addressed in this paper. The MHC considers the use of ‘pharmacological restraint’, (the use of medication, which is prescribed and administered for the specific and exclusive purpose of controlling or subduing acute or episodic aggressive, disturbed, or violent behaviour) to be a restrictive practice. The much-anticipated new Mental Health Act will, it is hoped, include Rules to govern the use of ‘pharmacological restraint’ in services. The MHC looks forward to consulting on ways to address this area in the not-too-distant future.
The MHC will remain focused on standards of care as part of its ongoing inspection and monitoring activities. We will continue to emphasise the benefits of a human rights-based approach to care and continue to highlight the need for collaboration, working towards the reduction and, where possible, elimination of restrictive practices in mental health services.
This accelerated reduction in the use of RPs in approved centres has been described as the greatest advance in human rights-based mental healthcare in Ireland since the closure of the asylums. An advance of this scale needs further evaluation to better understand how it was achieved.
For now, these data represent an achievement many thought impossible. Success has many parents. Failure, as they say, is an orphan. Leadership, collaboration, education and training have all played a role in delivery of human rights-based standards of care in ACs in Ireland. Many people have contributed to this positive story. This report is intended to recognise and celebrate their good work. The MHC wishes to congratulate all who have contributed so meaningfully. We highlight these data out of respect for all those delivering our mental health services and with due regard for all those using them.
Glossary
The definitions of seclusion and physical restraint, as defined by the MHC in its revised Rules governing the use of seclusion and Code of Practice on the use of physical restraint, are as follows:
Seclusion
Seclusion is defined in the revised Rules Governing the Use of Seclusion as “the placing or leaving of a person in any room, at any time, day or night, such that the person is prevented from leaving the room by any means”. Each episode of seclusion must be notified on CIS within three working days of its commencement, including the start date and time and the end date and time. Seclusion may only be used when there is an immediate threat of serious harm to self or to others.
Physical restraint
Physical restraint is defined in the revised Code of Practice on the Use of Physical Restraint as “the use of physical force (by one or more persons) for the purpose of preventing the free movement of a person’s body when the person poses an immediate threat of serious harm to self or others”. Each restraint episode must be reported to the MHC on CIS including the start date and time and the end date and time, within three working days of the commencement of the episode. Five types of physical restraint are reported (upright, supine, side, prone and other).
Acknowledgements
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The authors assert that the local ethics committee has determined that ethical approval for publication of this analysis was not required by their local Ethics Committee.
Funding statement
This research received no specific grant from any funding agency, commercial, or not for profit sector.
Competing interests
The authors are all current employees of the Mental Health Commission.