Introduction
The overwhelming evidence for a lack of diagnostic significance of Schneider's first-rank symptoms (FRS) in schizophrenia (Tandon et al. Reference Tandon, Gaebel, Barch, Bustillo, Gur, Keckers and Carpenter2013) led DSM-5 and ICD-11 authors to eliminate the special diagnostic significance placed on these symptoms in previous versions of the manuals. However, Moscarelli (Reference Moscarelli2020) argues that the previous data on the diagnostic value of FRS are invalid because of the lack of ‘strict compliance with Schneider's criterion for their definition’. More specifically, he argues that previous studies do not fit the phenomenological method for assessing FRS and that some ratings may have included equivocal or doubtful FRS.
Although Moscarelli notes significant methodological limitations in the literature, the article does not mention studies conducted in Schneider-oriented German centers (Koehler, Guth, & Grimm, Reference Koehler, Guth and Grimm1977; Marneros, Reference Marneros1984; Marneros, Rohde, Deister, & Sakamoto, Reference Marneros, Rohde, Deister and Sakamoto1987) or with a rigorous assessment methodology (Peralta & Cuesta, Reference Peralta and Cuesta1999) that failed to demonstrate a diagnostic specificity of FRS. Furthermore, he does not refer to evidence indicating that FRS can be expressed along a continuum of severity (Klosterkötter, Reference Klosterkötter1992; Koehler, Reference Koehler1979), similar to that reported for other reality-distortion symptoms (van Os, Linscott, Myin-Germeys, Delespaul, & Krabbendam, Reference van Os, Linscott, Myin-Germeys, Delespaul and Krabbendam2009). The report by Moscarelli aligns with some other recent studies that vindicate the historical, diagnostic, etiopathological, or clinical relevance of FRS (Cutting, Reference Cutting2015; Heinz et al., Reference Heinz, Voss, Lawrie, Mishara, Bauer, Gallinat and Galderisi2016; Kendler & Mishara, Reference Kendler and Mishara2019; Malinowski et al., Reference Malinowski, Tasso, Ortiz, Higuchi, Noto, Belangero and Cordeiro2020; Picardi, Reference Picardi2019). Thus, a re-examination of the diagnostic and clinical validity of FRS in psychotic disorders appears to be in order. While the debate about the importance of FRS has been mainly focused on their diagnostic value, there is a paucity of empirical studies examining other validity indicators, and no studies have examined the comparative validity between FRS and other reality-distortion symptoms.
In this report, using a rigorously phenomenological approach to elicit FRS, we examined (a) the degree to which ‘unequivocally present’ FRS differentiated schizophrenia from other psychotic disorders in a large sample of subjects with the full range of ‘functional’ psychotic disorders, and (b) the comparative validity between FRS and other reality-distortion symptoms against 16 external validators. Relatedly, we were specifically interested in examining the extent to which FRS predicted the validators over and above other delusions and hallucinations, a question that, to the best of our knowledge, has not been addressed previously.
Methods and results
The study sample comprised 1146 subjects with psychotic disorders derived from consecutive admissions to the psychiatry ward of the Complejo Hospitalario de Navarra (Spain) due to first-episode psychosis (n = 486) (Peralta, Moreno-Izco, Calvo-Barrena, & Cuesta, Reference Peralta, Moreno-Izco, Calvo-Barrena and Cuesta2013) or multi-episode psychosis (n = 660) (Peralta & Cuesta, Reference Peralta and Cuesta1999). The latter sample had been already employed to assess the diagnostic performance of FRS. All the subjects were examined using the Comprehensive Assessment of Symptoms and History (CASH) (Andreasen, Flaum, & Arndt, Reference Andreasen, Flaum and Arndt1992) that served to evaluate symptoms, diagnosis, and most external variables. All subjects were personally interviewed by VP or MJC, and to rate reality-distortion symptoms, we used the Scale for the Assessment of Positive Symptoms (SAPS), which is embedded within the CASH. The SAPS includes 18 delusions and hallucinations rated on a 6-point Likert-type scale, 7 of which are FRS: delusions of being controlled, delusions of mind reading, thought broadcasting/audible thoughts, thought insertion, thought withdrawal, voices commenting and voices conversing.
FRS were assessed using the phenomenological method described by Jaspers (Reference Jaspers1968); thus, when exploring one of the given FRS, an affirmative answer does not suffice to rate the symptom as present and the subject is asked to describe the experience as clearly as possible. Within the SAPS, clearly present delusional FRS are typically scored 2 (mild level), although this rating also allows ‘occasional’ doubts about the experience. Thus, we defined FRS as unequivocally present using a score ⩾3, corresponding to a presence of the experience at the level of moderate or higher.
To examine the diagnostic performance of FRS for schizophrenia, we used standard psychometric indices for a diagnostic test (Jaeschke, Guyatt, & Liimer, Reference Jaeschke, Guyatt, Liimer, Guyyat and Drummond2002). To study the external validity of FRS (sum score of the 7 FRS) and non-FRS (sum score of all other 11 delusions and hallucinations), we used 16 validators including antecedents, illness characteristics, episode characteristics, and psychosocial functioning variables. We conducted a series of linear regressions with the validators as dependent variables and symptom scores as independent variables. Last, a series of hierarchical linear regressions served to examine the incremental validity of the FRS score over and above the non-FRS score. We controlled for age, gender, and diagnosis (schizophrenia v. other psychotic disorders) in the analyses.
The mean age at admission was 33.5 years (s.d. = 13.4), 58% of the subjects were male, 73% were single and the mean educational level was 9.74 years (s.d. = 3.42). The DSM-IV diagnostic breakdown was as follows: schizophrenia (n = 513, 44.8%), schizophreniform disorder (n = 138, 12%), brief psychotic disorder (n = 136, 11.9%), delusional disorder (n = 62, 5.4%), schizoaffective disorder (n = 60, 5.2%), bipolar disorder (n = 106, 9.2%), major depressive disorder (n = 79, 6.9%), and psychotic disorder not otherwise specified (n = 52, 4,5%).
The mean (s.d.) FRS score was 5.94 (8.19), and the mean non-FRS score was 10.2 (6.65). The Pearson's correlation coefficient between the two scores was 0.51.
At least one of the FRS was present in 296 subjects with schizophrenia (56.9%) and in 224 subjects with other psychotic disorders (43.1%).
Diagnostic performance indices (with 95% confidence intervals) of FRS for diagnosing schizophrenia were as follows: sensitivity = 0.58 (0.54−0.61), specificity = 0.65 (0.62−0.67), positive predictive value (PPV) = 0.57 (0.54−0.60), negative predictive value (NPV) = 0.65 (0.63−0.68), positive likelihood ratio (LR) = 1.61 (1.43−1.86), negative LR = 0.65 (0.58−0.73), number needed to diagnose = 4.48 (3.56−6.07), and number needed to misdiagnose = 2.60 (2.41−2.80). Using a set prevalence for schizophrenia of 0.5, corresponding to an acute care unit, the adjusted PPV and NPV were 0.62 (0.57−0.66) and 0.60 (0.57−0.64), respectively; when using a set prevalence of 0.1, corresponding to a primary care setting, the adjusted PPV and PPN were 0.15 (0.13−0.19) and 0.93 (0.91−0.95), respectively. Table 1 shows the associations of FRS and non-FRS scores with the validators.
Table 1. Associations of first-rank and non-first-rank symptom scores from the Scale for the Assessment of Positive Symptoms (SAPS) with the validators
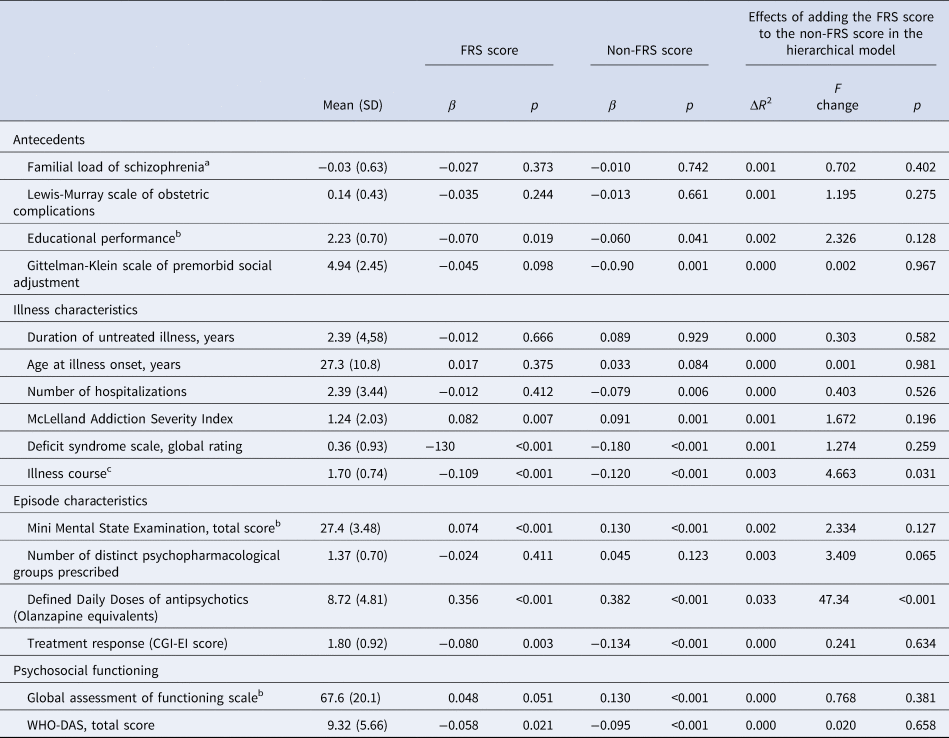
CGI-EI, Clinical Global Impression-Efficacy Index; FRS, First-rank symptoms; WHO-DAS, World Health Organization-Disability Assessment Schedule.
a Log-transformed score based on the presence of a positive history of schizophrenia in first-degree relatives taking into account age and number of relatives.
b Unless than otherwise specified, higher scores indicate more impairment.
c Scored 1 (remission), 2 (partial remission), and 3 (chronic/continuous).
Discussion
Following a strictly phenomenological approach to ascertain FRS in subjects with psychotic disorders, such as a restrictive definition of FRS to avoid false-positive cases, our data on the diagnostic value of FRS are in broad agreement with a recent meta-analysis reporting sensitivity and specificity values of 58% and 74%, respectively (Soares-Weiser et al., Reference Soares-Weiser, Maayan, Bergman, Davenport, Kirkham, Grabowski and Adams2015). Our findings indicate that within a mixed sample of psychotic disorders, the presence of at least one FRS increases the probability of a diagnosis of schizophrenia by 1.6-fold, which invalidates these symptoms as a diagnostic test according to standard criteria (Jaeschke et al., Reference Jaeschke, Guyatt, Liimer, Guyyat and Drummond2002).
Regarding the external validity issue, we found that the overall association pattern of FRS and non-FRS scores with the validators was rather similar. A major difference was that some validators (i.e. premorbid social adjustment, number of hospitalizations, and global assessment of functioning) were significantly related to non-FRS but not to FRS; however, the reverse was not true, which indicates an overall better predictive validity for non-FRS. Of the 16 validators examined, the FRS score significantly predicted only two validators over and above other reality-distortion symptoms (antipsychotic dose and illness course), and this was with a negligible increase in the explained variance. Thus, it can be concluded that FRS do not meaningfully add to the external validity showed by other delusions and hallucinations.
In view of the lack of diagnostic significance of FRS for schizophrenia together with the negligible added validity relative to other delusions and hallucinations, the following question arises: Why are we continuously debating about the relevance of FRS for schizophrenia when there is a lack of empirical data supporting it? Without doubt, the phenomenology of FRS is fascinating, and they clearly appear to be qualitatively distinct from other reality-distortion symptoms from a phenomenological perspective. However, the phenomenological distinctiveness of FRS does not appear to be of diagnostic or clinical relevance. For example, if delusional FRS are not only merely a kind of delusional content but also a form of experience, as claimed by Cermolacce, Sass, & Parnas (Reference Cermolacce, Sass and Parnas2010), this form of experience should be assessed and subjected to empirical testing to examine its clinical validity and utility. Otherwise, such hypotheses will remain a sterile ground for the clinician.
It is rarely noted in the literature regarding the putative diagnostic value of FRS that the weight of the question is not (or not only) the FRS issue but the very concept of schizophrenia and Schneider's own concept thereof. Schneider never provided clear diagnostic criteria for schizophrenia, except for his famous assertion that ‘if first-rank symptoms are present in absence of an organic pathology, we call it schizophrenia’ (Schneider, Reference Schneider, Hirsh and Shepperd1974). Furthermore, he acknowledged that schizophrenia could be diagnosed on the basis of second-rank (i.e. other disorders of the experience) and even third-rank symptoms (i.e. behavioral signs) ‘if present in certain combinations and numbers’ (Schneider, Reference Schneider, Hirsh and Shepperd1974). The main problem here is that Schneider never provided such ‘combinations [of symptoms] and numbers’, and, as a consequence, his schizophrenia concept remained a rather obscure matter. He never published empirical data about the prevalence of symptoms and other illness characteristics, and the majority of the diagnoses of schizophrenia according to Schneider's concept appear to be founded on non-FRS (Marneros, Reference Marneros1984). In other words, based on a subjective position, Schneider placed a high specificity value on FRS, but he left unanswered their sensitivity value, and hence their true diagnostic significance. We believe that much of the misunderstanding about the diagnostic and clinical validity of FRS for schizophrenia is rooted in Schneider's confusing concept of the disorder.
Funding
This work was supported by the Carlos III Health Institute (FEDER Funds) from the Spanish Ministry of Economy and Competitiveness (VP grant number PI16/02148) and the Regional Government of Navarra (VP grant number 31/17). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.






