Background
A hospital patient housed in a room where a previous patient had a multidrug-resistant organism (MDRO) has twice the risk of acquiring that MDRO. Reference Mitchell, Dancer, Anderson and Dehn1 There are barriers to optimal environmental cleaning in hospitals, including for Environmental Management Service (EMS) staff, Reference Hewage, Cao, Jones and Fraser2,Reference Goedken, McKinley and Balkenende3 who often have limited training and high turnover, are not integrated into healthcare teams or empowered to change practices, and experience high time pressure to disinfect rooms quickly.
To improve disinfection, hospitals have added technologies like ultraviolet (UV-C) light devices that emit short-wavelength light. We previously found that UV-C implementation in Veterans Affairs (VA) hospitals was associated with a 19% reduction in gram-negative bloodstream infections (BSIs) but with significant hospital variation in BSI improvements. Reference Goto, Hasegawa, Balkenende, Clore, Safdar and Perencevich4 To investigate this variation, this project aimed to evaluate facilitators and barriers for UV-C disinfection as an adjunct to patient room disinfection across VA hospitals.
Methods
Data Collection
We invited personnel at 40 US VA hospitals that reported using UV-C disinfection during the 2010–2018 survey. Reference Goto, Hasegawa, Balkenende, Clore, Safdar and Perencevich4 From June 2022 to May 2023, we conducted nationwide interviews with hospital staff (EMS leaders, EMS personnel, infection preventionists, and multidrug-resistant-organism coordinators). The study was approved by the University of Iowa Institutional Review Board (#202112202) and the Research and Development Committee at the Iowa City VA. Prospectively developed interview guides included constructs of external and internal environments, organization, tools and technology, tasks, and persons. The qualitative team (KCD, SHS, CCG, AMR, JFW) conducted and recorded in-person or MS Teams interviews: (a) brief interviews focused on device types, types of rooms disinfected, and UV-C processes, and (b) in-depth individual or group interviews. Interviewers summarized brief interviews using a topical template; in-depth interviews were transcribed. We imported audited transcripts and template summaries into qualitative analysis software, MAXQda. 5
Data Analysis
We conducted template analysis of brief-interview summaries and consensus-based thematic analysis Reference Terry, Hayfield, Clarke and Braun6 of in-depth interviews using an adapted codebook, adding emergent inductive themes and documenting changes systematically. After finalizing the codebook, we applied codes to template summaries.
Results
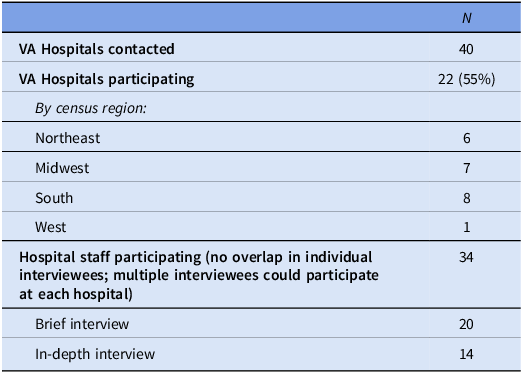
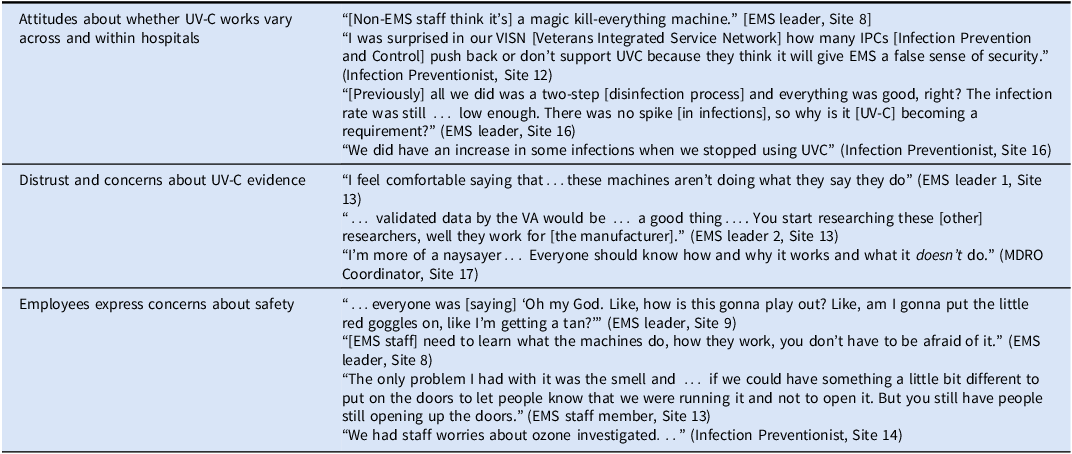
Table 1 provides information about hospitals and participants. Thirty-four staff members participated. Table 2 provides exemplar quotes for selected themes.
Table 1. Characteristics of participating hospitals and hospital personnel

Table 2. Exemplar quotes for selected themes

Summary of UV-C use
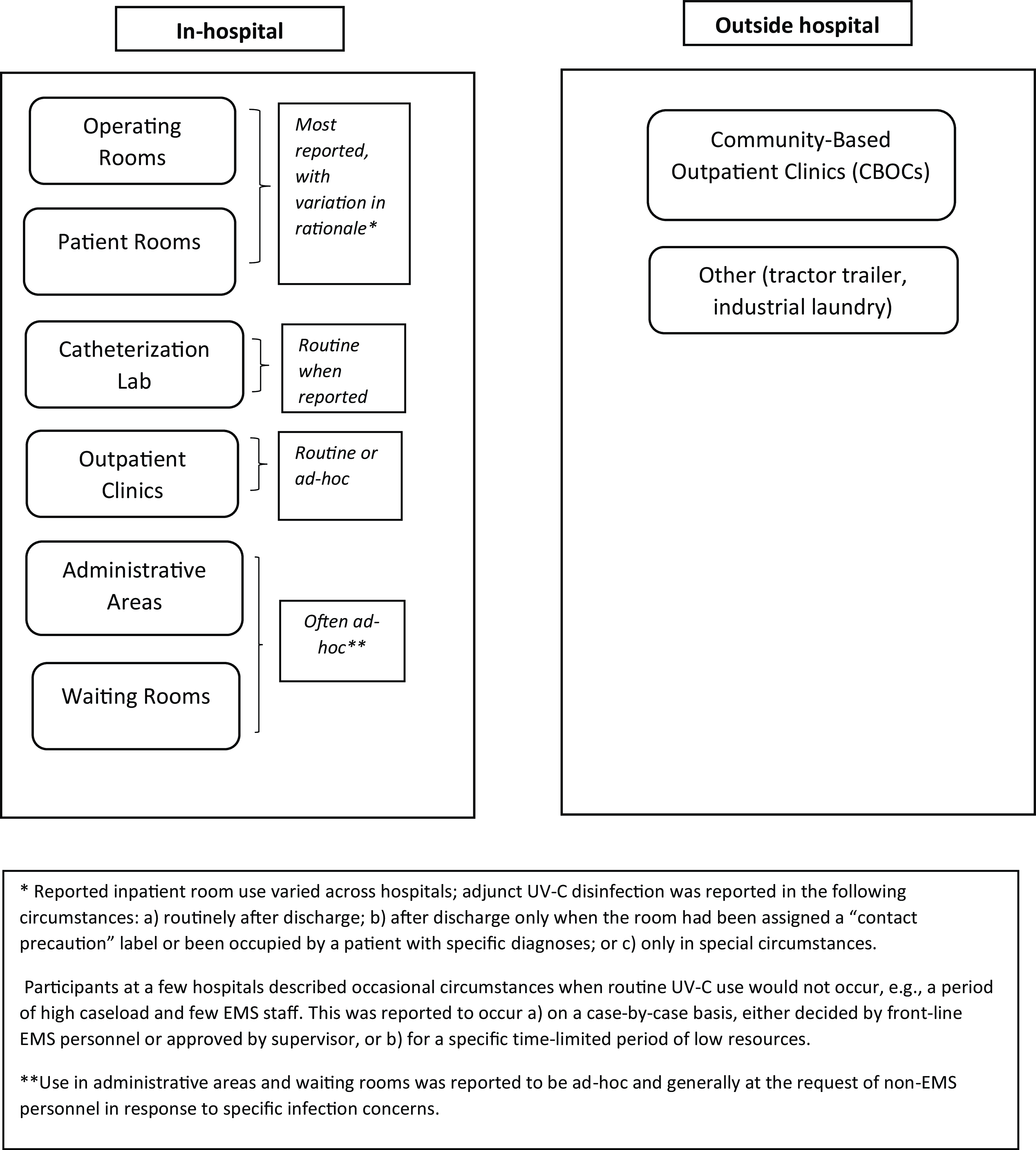
Twenty-one of 22 participating hospitals reported using UV-C disinfection in at least one hospital setting, with variation in locations, frequency, and rationales (Figure 1). One had discontinued all UV-C use. Another discontinued UV-C in patient rooms and reduced its use in operating rooms to after-hours, but continued its use in the catheterization lab and gastrointestinal clinic.

Figure 1. Reported UV-C use locations.
Manual cleaning first
All interviewees emphasized that manual cleaning and disinfection was the priority, with UV-C as an adjunct process, sometimes described using metaphors like a “cherry on top” or “clear nail polish on top of a painted nail.” A frequently expressed concern was that EMS staff might overestimate the impact of UV-C disinfection and reduce their manual cleaning.
At one hospital with this concern (“Before, EMS and nurses used to think UV was the be-all end-all”), EMS began reporting both UV-C usage and microbiology testing results at that hospital, to clarify that manual cleaning remained vital (Site 18).
Attitudes about UV-C
Attitudes were mixed regarding UV-C’s efficacy, feasibility, and acceptability. Many viewed UV-C as helpful for infection prevention (eg, “fantastic tool,” “I’m a big believer”) and multiple facilities reported successful implementation once procedures were in place and personnel were educated on the process and the technology.
However, sometimes leaders’ skepticism led to UV-C being discontinued or used inconsistently. Some personnel were not persuaded that UV-C was effective in killing organisms. Many distrusted manufacturer claims regarding exposure times and efficacy. For a few participants, even data from a clinical trial was insufficient evidence if it involved non-VA settings. A few participants did not perceive that UV-C reduced local infection rates.
Leadership support of UV-C, tied to their perception of its efficacy, affected implementation, including its discontinuation. At site 16, the EMS chief stopped using UV-C after previously working in 2 other VA hospitals that used it. At Site 4, two participants reported their EMS chief was “not a fan” and thought UV-C was ineffective; while this hospital had UV-C devices, implementation was “rocky at best” with staff “pushback,” frequent device breakage, and storage and access obstacles. At hospitals where leadership supported UV-C use (eg, “our chief is passionate”), implementation succeeded despite barriers (eg, time, storage) that deterred other hospitals.
Participants also described employee concerns about device safety, including smell, eye injuries, sunburns, and ozone exposure, especially early in implementation.
Other barriers
Other barriers included high patient volumes requiring fast room turnovers, reduced EMS staffing, equipment and maintenance costs, technology variation, concerns about potential degradation of equipment and furnishings, effective testing, and competing priorities. Minor barriers included user error, inadequate storage space, bulb or device breakage, and device element malfunction or loss.
Facilitators
COVID-19
Participants reported that COVID-19-related funds and leadership backing supported UV-C integration and pandemic-related infection concerns increased colleagues’ respect for EMS staff knowledge.
Role of education
Hospitals that reported successful UV-C integration emphasized training. Education frequency and types (hands-on, formal; manufacturer-led or internal) varied. Several hospitals conducted manufacturer-led training periodically and held refresher courses annually. However, several hospitals reported that they did not train all EMS employees to use UV-C, either because some employees were assigned to disinfect spaces where UV-C was not typically used, or some were uncomfortable with the technology. Education, when provided, reassured personnel about safety and improved employees’ knowledge and their skills, eg reducing bulb breakage.
Collaboration
Given concerns about room turnover and high census counts, EMS and nursing staff sometimes experienced frustration with UV-C’s addition, potentially exacerbating negative relationships between the two workforces. Participants reported that “relationship building” and improving communication among EMS, nursing, and infection control personnel could create a supportive environment.
For example, one EMS chief described a non-collegial situation when they assumed leadership. Within that context, “nursing would get mad that…we had to spend an extra 10 minutes cleaning a room [by using UV-C].” In response, the EMS leaders took steps to improve communication with nursing about EMS practices, including UV-C use. They “embedded” EMS staff in specific units to learn the nurses’ workflow and establish relationships, and educated nurses about EMS roles, responsibilities, and processes: “it took us learning about their jobs, them learning about ours.” These strategies allowed EMS and nursing staff to plan for both manual and UV-C disinfection during room turnovers and integrate this extra time into both EMS and nursing workflows.
At another hospital, IP personnel “micromanage[d]” environmental cleaning and UV-C use, eg. reading UV-C usage reports, conducting microbiology testing on all rooms to evaluate disinfection, then critiquing EMS. To reset relationships between IP and EMS, EMS took over control of testing and UV-C reports, and IP moved from “tattling” and “correcting” to acting as a “partner” that respected EMS’ professionalism.
Professionalism and commitment to infection prevention
Some participants at hospitals that successfully implemented UV-C into environmental cleaning described it as a way to show Veterans and families their commitment to patient safety or improve the hospital’s perceptions of EMS professionalism.
Discussion
There is some evidence that UV-C can be an effective adjunct to environmental cleaning in reducing certain healthcare-associated infections in hospitals, and yet some caution exists. Reference Anderson, Chen and Weber7–Reference Goto and Donskey9 Since it is being used in the VA healthcare system, our qualitative study identified barriers and enablers of UV-C disinfection and variation in UV-C disinfection locations and rationales. Some hospitals reported that UV-C was well integrated into their routine practices. However, barriers were significant enough that one hospital discontinued its use entirely, and another stopped in patient rooms. Literature suggests US EMS workers experience challenges related to work pressure, low staffing, high turnover, or feelings of undervalue. Reference Hewage, Cao, Jones and Fraser2,Reference Goedken, McKinley and Balkenende3,Reference Pedersen, Masroor and Cooper10 Counterbalancing these, we found that EMS personnel were proud of their infection prevention expertise and that UV-C use could strengthen colleagues’ perception of EMS professionalism. However, we also found personnel questioned UV-C’s efficacy and identified other barriers including cost, efficiency, and safety concerns.
Goedken et al Reference Goedken, McKinley and Balkenende3 note the benefit of integrating EMS personnel into the larger healthcare team. We also found that greater collaboration among nursing, IP, and EMS personnel can help support EMS staff to integrate UV-C into routine environmental cleaning. Other facilitators included leadership support of UV-C use, personnel’s professional competence and commitment to infection prevention, and COVID-19-related financial resources and infection concerns.
These VA hospitals used a wide variety of UV-C devices and had varied UV-C locations, processes, and procedures. Thus, our findings may not be generalizable. However, findings were similar across hospitals, and many barriers and facilitators we identified may transfer to UV-C implementation in a range of hospitals.
Conclusions
Given the potential benefits of UV-C, efforts to address barriers and support facilitators could drive implementation. A UV-C implementation toolkit, informed by VA staff feedback, may improve acceptability of UV-C technology among EMS staff. Interprofessional collaboration and leadership support is likely to enhance integration of UV-C into infection prevention systems in VA hospitals.
Acknowledgements
The views expressed in this presentation are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Financial Support
This work was funded by the VA Quality Enhancement Research Initiative (QUERI) Award QUE 20-016.
Competing interests
No authors report a conflict of interest with this study.