Triplet pregnancies represent a rare and high-risk obstetric condition, occurring in approximately 93 per 100,000 deliveries worldwide (Martin et al., Reference Martin, Hamilton, Osterman and Driscoll2019). The rise in higher order multiple pregnancies over recent decades has largely been attributed to the widespread use of assisted reproductive technologies (ART). However, recent policies limiting the number of embryo transfers have led to a stabilization and even a decline in the incidence of triplet pregnancies in some countries (Fennessy et al., Reference Fennessy, Doyle, Naud, Reidy and Umstad2015; Haas et al., Reference Haas, Hourvitz, Dor, Yinon, Elizur and Mazaki-Tovi2014).
Compared to singleton and twin pregnancies, triplet pregnancies are associated with significantly increased maternal, fetal, and neonatal adverse outcomes (Bernal Claverol et al., Reference Bernal Claverol, Aracil Moreno, Ruiz Minaya, Fernández Muñoz, Reyes Angullo, González Navarro, García-Honduvilla, Ortega, García Tizón, Pintado-Recarte and de León-Luis2024; Bernal Claverol et al., Reference Bernal Claverol, Ruiz Minaya, Aracil Moreno, Tizón, Pintado Recarte, Alvarez-Mon, Arribas, Ortega and De Leon-Luis2022; Curado et al., Reference Curado, D’Antonio, Papageorghiou, Bhide, Thilaganathan and Khalil2019; Revello et al., Reference Revello, De la Calle, Moreno, Duyos, Salas and Zapardiel2013), with prematurity being the leading cause of neonatal morbidity and mortality.
Among the various determinants of perinatal outcome in triplet pregnancies, increasing attention has recently been directed toward the role of chorionicity. Trichorionic triamniotic triplet pregnancies, where each fetus has a separate placenta, are generally associated with more favorable outcomes than nontrichorionic pregnancies, which include monochorionic components characterized by placental vascular anastomoses (Bernal Claverol et al., Reference Bernal Claverol, Aracil Moreno, Ruiz Minaya, Fernández Muñoz, Reyes Angullo, González Navarro, García-Honduvilla, Ortega, García Tizón, Pintado-Recarte and de León-Luis2024; Kawaguchi et al., Reference Kawaguchi, Ishii, Yamamoto, Hayashi and Mitsuda2013). Monochorionicity in multiple gestations predisposes to selective intrauterine growth restriction, preterm birth, and unique complications such as twin-to-twin transfusion syndrome, all of which contribute to increased perinatal morbidity (Bernal Claverol et al., Reference Bernal Claverol, Ruiz Minaya, Aracil Moreno, Tizón, Pintado Recarte, Alvarez-Mon, Arribas, Ortega and De Leon-Luis2022; Lewi et al., Reference Lewi, Van Schoubroeck, Gratacós, Witters, Timmerman and Deprest2003).
Nontrichorionic triplets tend to be delivered earlier than trichorionic ones, resulting in a higher incidence of low birth weight, respiratory distress syndrome (RDS), and increased need for neonatal intensive care unit (NICU) (Curado et al., Reference Curado, D’Antonio, Papageorghiou, Bhide, Thilaganathan and Khalil2019; Revello et al., Reference Revello, De la Calle, Moreno, Duyos, Salas and Zapardiel2013). Maternal complications, such as postpartum hemorrhage, also appear to be influenced by chorionicity (Abdulsalam et al., Reference Abdulsalam, Bourdakos, Burns, Zervides, Yap, Adra, Nakanishi, Than, Chervenak and Arulkumaran2024).
Given the limited data available in the current literature, partly due to the rarity of this condition, triplet pregnancies pose a complex challenge for clinicians. Only a few studies have comprehensively analyzed the outcomes in triplet pregnancies stratified by chorionicity, leading to inconsistent conclusions. A better understanding of the determinants of obstetrics and neonatal care is essential for improving care strategies and providing accurate prenatal counseling regarding the potential risks associated with triplet pregnancies.
This study aimed to evaluate the impact of chorionicity on maternal, fetal, and neonatal outcomes in a cohort of triplet pregnancies managed at a tertiary referral center over a 15-year period.
Materials and Methods
Study Design and Population
This retrospective cohort study included all triplet pregnancies delivered at Careggi University Hospital in Florence, a tertiary referral maternity center, between January 2010 and May 2025. Pregnancies were identified retrospectively using the hospital’s comprehensive antenatal care database.
Triplet pregnancies complicated by selective fetal reduction or spontaneous first-trimester loss of one or more fetuses were excluded. Cases with inconclusive data regarding chorionicity were also excluded from the analysis.
Chorionicity was determined by first-trimester ultrasound examination performed between 11+0 and 13+6 weeks, based on the number of placentas and the presence or absence of the lambda sign. Triplet pregnancies were classified as trichorionic triamniotic or nontrichorionic (monochorionic-triamniotic or dichorionic-triamniotic).
Data Collection
Maternal demographic characteristics, obstetric history, mode of conception, and pregnancy complications were retrieved from electronic medical records. Obstetric outcomes included gestational age at delivery, mode of delivery, and occurrence of postpartum hemorrhage.
Neonatal outcomes assessed were perinatal mortality, birth weight, Apgar scores at 1 and 5 minutes, need for NICU admission, and requirement for respiratory support. Birth weight was categorized as follows: extremely low birth weight (<1000 g), very low birth weight (<1500 g), and low birth weight (<2500 g).
Birth-weight discordance was calculated according to the formula: (Larger weight - Smaller weight)/Larger weight × 100%, and was defined as significant when ≥20%.
Neonatal complications, including respiratory distress syndrome (RDS), hypoglycemia, sepsis, and jaundice, were also recorded.
Statistical Analysis
Clinical characteristics, along with maternal and neonatal outcomes, were gathered by reviewing electronic medical records and then encoded into a Microsoft Excel spreadsheet. Statistical analysis was performed using IBM SPSS Statistics, version 29. Descriptive statistics, including mean, median, and standard deviation, were utilized to summarize the characteristics of the women and neonates. Frequency and proportion were applied to categorical variables, while median and quartile or mean and standard deviation were used for numerical variables. Fisher’s exact or chi-square tests were employed to assess differences in frequency profiles between groups. Medians were compared using the Mann–Whitney U test, whereas means and standard deviation were compared using the Student’s t-test based on the Shapiro-Wilk test for normality. Correlation analysis was conducted using the Spearman test. Multivariable regression analyses were performed to identify factors independently associated with maternal and neonatal outcomes. Covariates included in the models were maternal age (>35 years), mode of conception (ART vs. spontaneous), chorionicity (trichorionic vs. nontrichorionic), and gestational age at delivery, as these variables are well-established determinants of perinatal outcomes in multiple gestations. Logistic regression was applied for binary outcomes (e.g., postpartum hemorrhage, NICU admission), while linear regression was used for continuous outcomes (e.g., gestational age at delivery, birth weight). Results are presented as odds ratios (OR) or regression coefficients (b) with 95% confidence intervals (CI). Maternal outcomes were analyzed at the maternal level, whereas neonatal outcomes were analyzed per newborn, acknowledging nonindependence within triplet sets. All statistical analyses were considered significant at p value < .05 and highly significant at p value < .01.
Results
Maternal and Pregnancy Characteristics According to Chorionicity
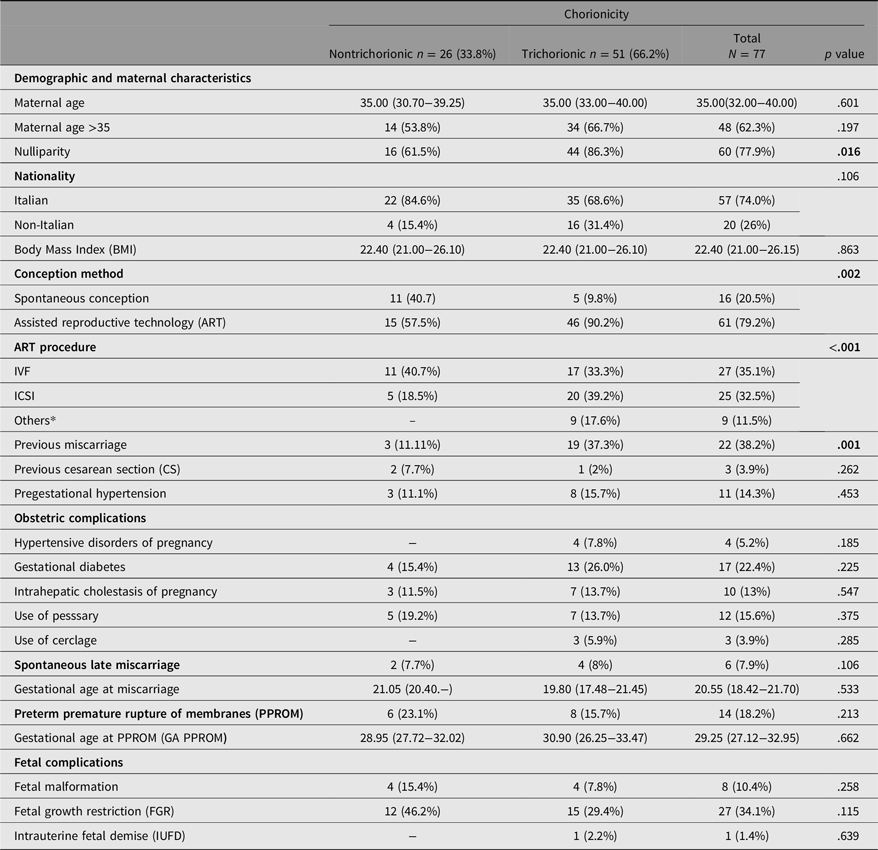
Maternal and pregnancy characteristics and fetal outcomes are summarized in Table 1. A total of 77 triplet pregnancies were identified during the study period and met the inclusion criteria. Of these, 51 pregnancies were trichorionic, and 26 were nontrichorionic (22 dichorionic and 4 monochorionic). No cases of diamniotic or monoamniotic triplet pregnancies were observed.
Table 1. Maternal demographic characteristics and obstetric and fetal outcomes

Note: Categoric variables are presented as n (%), continuous variables as median (interquartile range); *Pharmacological treatment and intrauterine injection. Bold p values indicate statistical significance (p < .05).
Four cases (5.2%) resulted in late miscarriage of all three fetuses. Seventy-one pregnancies (92.2%) resulted in the delivery of three live neonates, two pregnancies (2.6%) in late miscarriage of two fetuses, and one pregnancy (1.3%) was complicated by intrauterine fetal demise (IUFD) of one fetus. Thus, the 77 included pregnancies resulted in the birth of 214 live neonates.
The mean maternal age was 35 years, with 62.3% of women being over 35 years old. Most women were of Italian nationality (74.4%), and the mean pregestational body mass index was 22.4 kg/m2.
ART was the predominant mode of conception, particularly in the trichorionic group (90.2% vs. 57.5%, p = .002). In vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) was also significantly more frequent in the trichorionic group (p < .001). Nulliparity was more common among women with trichorionic pregnancies compared with those with nontrichorionic pregnancies (86.3% vs. 61.5%, p = .016), and a history of spontaneous miscarriage was also significantly more prevalent in the trichorionic group (37.3% vs. 11.1%, p = .001). No significant differences were observed between groups concerning hypertensive disorders or gestational diabetes mellitus.
Fetal malformations were observed in eight pregnancies: four cases of renal malformations, one cardiac, one gastrointestinal, and one skeletal malformation. No statistically significant differences were found between the groups.
Delivery and Neonatal Outcomes According to Chorionicity
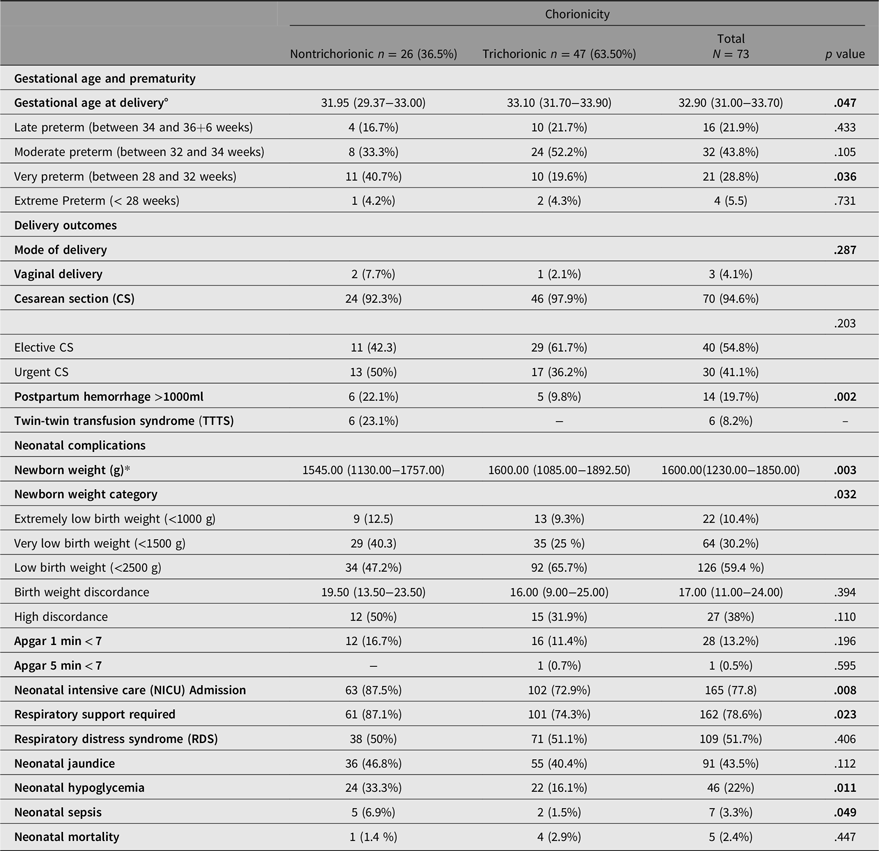
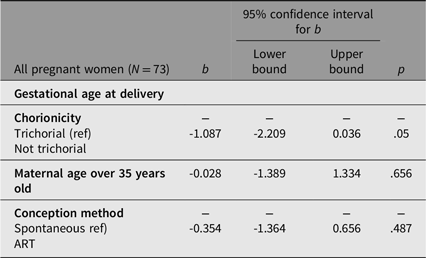
All delivery and neonatal complications are summarized in Table 2. The gestational age at delivery was significantly lower in nontrichorionic pregnancies compared to trichorionic pregnancies (median 31.95 vs. 33.10 weeks; p = .047). Multivariable linear regression analysis (Table 3A) revealed that nontrichorionicity was independently associated with a 1.1-week reduction in gestational age at delivery (b = -1.087; 95% CI, [–2.209, 0.036]; p = .05).
Table 2. Delivery and neonatal complications

Note: Categoric variables are presented as n (%), continuous variables as median (interquartile range); *The analysis was limited to women who delivered all three triplets, since women who retained only one fetus had a higher gestational age at delivery. Birth weight discordance was calculated as (largest birth weight – smallest birth weight)/largest birth weight × 100. High discordance was defined as ≥25%. Bold p values indicate statistical significance (p < .05).
Table 3A. Binary logistic regression model for the prediction of postpartum hemorrhage

Note: Bold p values indicate statistical significance (p < .05).
Cesarean section was the predominant mode of delivery in both groups, with a slightly higher rate in the trichorionic group (97.9% vs. 92.3%, p = .287). Vaginal delivery was rare, occurring in only 4.1% of cases overall.
Regarding obstetric complications, the incidence of postpartum hemorrhage (defined as blood loss > 1000 mL) was significantly higher in the nontrichorionic group (22.1% vs. 9.8%, p = .002). Multivariable logistic regression analysis confirmed that non-trichorionicity was an independent and strong risk factor for postpartum hemorrhage (odds ratio [OR] = 31.5, 95% CI [4.4, 266.0], p < .001), after adjusting for maternal age, gestational age at delivery, and mode of conception (Table 3B).
Table 3B. Multivariable linear regression model for the prediction of the gestational age at delivery

Median birth weight was significantly lower among non-trichorionic newborns (1545 g vs. 1600 g, p = .003). The incidence of extremely low birth weight (<1000 g) and very low birth weight (<1500 g) was higher in the non-trichorionic group (12.5% vs. 9.3%, and 40.3% vs. 25%, respectively; p<0.001). Intra-triplet birth-weight discordance assessment showed that 38% of all triplet pregnancies were complicated by high discordance (>20%) between the largest and the smallest neonate. The median discordance was 19.5% (IQR 13.5–23.5) in trichorionic pregnancies and 16.0% (IQR 9.0–25.0) in nontrichorionic pregnancies (p = .394). High discordance was more frequent in nontrichorionic pregnancies (50.0% vs. 31.9%), although the difference did not reach statistical significance (p = .110).
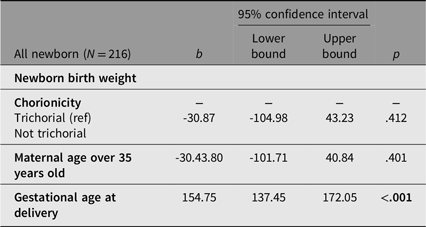
However, in multivariable regression analysis, only gestational age was independently and significantly associated with higher birth weight (b = 154.75, 95% CI [137.45, 172.05], p < .001). In contrast, nontrichorionicity and maternal age over 35 years were not significant predictors (Table 4A).
Table 4A. Multivariable linear logistic regression model for the prediction of the newborn birth weight

Note: Bold p values indicate statistical significance (p < .05).
Neonatal morbidity was overall more frequent in nontrichorionic pregnancies. The need for NICU admission was higher in the nontrichorionic group (87.5% vs. 72.9%, p = .008), as was the requirement for respiratory support (87.1% vs. 74.3%, p = .023).
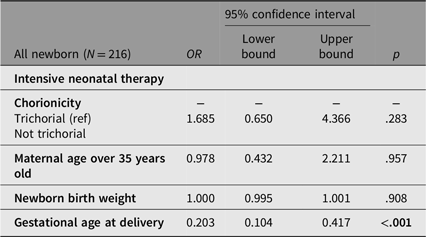
However, in multivariable logistic regression analysis, nontrichorionicity was not independently associated with NICU admission (OR = 1.685, 95% CI [0.650, 4.366], p = .283), nor were birth weight or maternal age over 35 years. Only advancing gestational age at delivery significantly reduced the odds of NICU admission (OR = 0.203, 95% CI [0.104, 0.417], p < .001; see Table 4B). Hypoglycemia and sepsis were also significantly more prevalent among nontrichorionic newborns (p = .011 and p = .049 respectively). No significant differences were observed between groups in the incidence of RDS or neonatal mortality (Table 2).
Table 4B. Binary logistic regression model for predicting admission to Intensive neonatal therapy

Note: Bold p values indicate statistical significance (p < .05).
Discussion
Our 15-year cohort study describes a substantial burden of complications associated with triplet pregnancies, regardless of chorionicity, with a high prevalence of maternal and neonatal complications and neonatal care requirements. Chorionicity emerged as a key determinant of risk. Our findings confirm its crucial role in influencing pregnancy outcomes and adverse perinatal events, primarily through its effect on gestational age at delivery.
Consistent with the observations of Fennessy et al. (Reference Fennessy, Doyle, Naud, Reidy and Umstad2015) and Shah et al. (Reference Shah, Roman, Viteri, Haidar, Ontiveros and Sibai2018), who reported a higher prevalence of trichorionicity following ART, the majority of cases in our cohort were conceived through ART, particularly within the trichorionic group. In contrast, spontaneous triplet pregnancies were more frequently associated with a monochorionic component, reflecting the natural occurrence of embryonic division (Morency et al., Reference Morency, Shah, Seaward, Whittle and Murphy2016).
Interestingly, although ART has previously been associated with increased obstetric adverse events in multiple gestation (Morency et al., Reference Morency, Shah, Seaward, Whittle and Murphy2016; Seravalli et al, Reference Seravalli, Maoloni, Pasquini, Bolzonella, Sisti, Petraglia and Di Tommaso2020; Shah et al., Reference Shah, Roman, Viteri, Haidar, Ontiveros and Sibai2018), our multivariable analysis indicates that ART was not an independent determinant of adverse outcomes once chorionicity was taken into account. This finding supports the hypothesis that placental sharing, rather than mode of conception, is the primary determinant of risk.
Advanced maternal age, more common among women conceiving via ART, has been suggested as a risk factor for obstetric complications and adverse neonatal outcomes in triplet pregnancies (Rubinshtein et al., Reference Rubinshtein and Golyanovskiy2021). Nevertheless, in our analysis, it did not emerge as a significant risk factor or independent determinant of adverse outcomes.
Regarding obstetric outcomes, nearly all triplet pregnancies in our cohort were delivered by cesarean section, consistent with current clinical guidelines (National Collaborating Centre for Women’s and Children’s Health, 2011; American College of Obstetricians and Gynecologists, 2014). Cesarean delivery remains the preferred mode of birth for triplet gestations due to the increased risk of fetal malpresentation, umbilical cord accidents, and complex intrapartum dynamics (Lappen et al., Reference Lappen, Hackney and Bailit2016; Revello et al., Reference Revello, De la Calle, Moreno, Duyos, Salas and Zapardiel2013). The high cesarean rate observed in our study is comparable to that reported by Bernal Claverol et al. (Reference Bernal Claverol, Aracil Moreno, Ruiz Minaya, Fernández Muñoz, Reyes Angullo, González Navarro, García-Honduvilla, Ortega, García Tizón, Pintado-Recarte and de León-Luis2024). Interestingly, urgent cesarean sections were more frequent among non-trichorionic pregnancies, likely reflecting their earlier gestational age at delivery and the higher incidence of monochorionic-related complications (Kawaguchi et al., Reference Kawaguchi, Ishii, Yamamoto, Hayashi and Mitsuda2013; Sato et al., Reference Sato, Ishii, Yokouchi, Murakoshi, Kiyoshi, Nakayama, Yonetani and Mitsuda2016).
Postpartum hemorrhage was significantly more frequent in non-trichorionic pregnancies. While Bernal Claverol et al. (Reference Bernal Claverol, Aracil Moreno, Ruiz Minaya, Fernández Muñoz, Reyes Angullo, González Navarro, García-Honduvilla, Ortega, García Tizón, Pintado-Recarte and de León-Luis2024) did not observe significant differences in postpartum hemorrhage rates according to chorionicity, our findings suggest that abnormal placentation associated with non-trichorionic pregnancies may contribute to an increased risk of hemorrhage. This is consistent with the hypotheses proposed by Abdulsalam et al. (Reference Abdulsalam, Bourdakos, Burns, Zervides, Yap, Adra, Nakanishi, Than, Chervenak and Arulkumaran2024), who linked placental abnormalities to hemorrhagic morbidity in twin gestations. Our multivariable analysis confirmed non-trichorionicity as an independent predictor of postpartum hemorrhage, highlighting the need to anticipate and proactively manage this complication during delivery planning.
Prematurity emerged as the principal adverse outcome associated with non-trichorionic pregnancies. Our data demonstrated a strong association between lower gestational age at delivery and non-trichorionicity, consistent with previous studies (Bernal Claverol et al., Reference Bernal Claverol, Aracil Moreno, Ruiz Minaya, Fernández Muñoz, Reyes Angullo, González Navarro, García-Honduvilla, Ortega, García Tizón, Pintado-Recarte and de León-Luis2024; Curado et al., Reference Curado, D’Antonio, Papageorghiou, Bhide, Thilaganathan and Khalil2019; Levy-Coles et al., Reference Levy-Coles, Erez, Mizrakli, Benshalom-Tirosh and Rabinovich2024; Revello et al., Reference Revello, De la Calle, Moreno, Duyos, Salas and Zapardiel2013). Furthermore, multivariable analysis confirmed that chorionicity remained an independent predictor of gestational age at delivery, even after adjusting for maternal age and mode of conception. These findings emphasize the central role of placental factors influenced by chorionicity, such as unequal placental sharing and vascular compromise, in contributing to earlier delivery (Kawaguchi et al., Reference Kawaguchi, Ishii, Yamamoto, Hayashi and Mitsuda2013; Sato et al., Reference Sato, Ishii, Yokouchi, Murakoshi, Kiyoshi, Nakayama, Yonetani and Mitsuda2016). Birth weight analysis further highlights the impact of prematurity. Newborns from non-trichorionic pregnancies had significantly lower birth weights. Extremely low birth weight and very low birth weight were significantly more frequent in this group. However, multivariable regression identified advancing gestational age as the primary independent predictor of birth weight. After adjusting for gestational age, non-trichorionicity was no longer found to be independently associated with birth weight. Our findings on birth weight are consistent with those reported by Lamb et al. (Reference Lamb, Middeldorp, van Beijsterveldt, Vink, Haak and Boomsma2011), who found that chorionicity and zygosity, rather than the mode of conception, were the primary determinants of birth weight in triplet pregnancies.
Furthermore, although FGR rates were numerically higher among non-trichorionic pregnancies, this difference did not reach statistical significance. These findings are consistent with previous studies (Kawaguchi et al., Reference Kawaguchi, Ishii, Yamamoto, Hayashi and Mitsuda2013; Lamb et al., Reference Lamb, Vink, Middeldorp, van Beijsterveldt, Haak, Overbeek and Boomsma2012) and support the hypothesis that non-trichorionic placentation may contribute to an increased risk of growth restriction, potentially due to compromised blood flow or increased competition for limited placental resources among fetuses. This suggests that the lower birth weights observed in non-trichorionic pregnancies may not be solely explained by earlier gestational age at delivery. Neonatal complications closely mirrored the patterns observed in birth weight and gestational age. Newborns from non-trichorionic pregnancies were more likely to require NICU admission, respiratory support, and treatments for hypoglycemia and sepsis. However, in multivariable analysis, only gestational age at delivery remained a significant independent predictor of NICU admission, while neither birth weight nor chorionicity showed significant associations. This suggests that the influence of chorionicity on neonatal outcomes may be mediated indirectly through its impact on gestational age, rather than acting as a direct risk factor. Interestingly, certain complications, such as RDS and neonatal mortality, did not differ significantly between groups, suggesting that advances in neonatal care may have mitigated some expected disparities, as also reported by Bernal Claverol et al. (Reference Bernal Claverol, Aracil Moreno, Ruiz Minaya, Fernández Muñoz, Reyes Angullo, González Navarro, García-Honduvilla, Ortega, García Tizón, Pintado-Recarte and de León-Luis2024).
Despite the increased morbidity, overall perinatal mortality in our cohort remained low, reflecting improvements in fetal surveillance, preterm birth management, and neonatal intensive care over the past decade. These findings are encouraging and suggest that, although non-trichorionic triplet pregnancies present significant clinical challenges, proactive multidisciplinary management can substantially improve outcomes (Mhatre & Craigo, Reference Mhatre and Craigo2021).
Strengths and Limitations
A key strength of this study is the comprehensive characterization of maternal, obstetric, and neonatal outcomes, with a specific focus on chorionicity. The use of multivariable analyses to identify independent risk factors strengthens the validity of the findings. Additionally, data were collected over an extended period in a tertiary referral center with standardized management protocols, enhancing consistency and reliability.
However, several limitations must be acknowledged. The retrospective and single-center design may limit generalizability, and the relatively small sample size reduces statistical power for some subgroup analyses. Another limitation of our study is that neonatal outcomes within triplet sets were analyzed at the individual newborn level without adjusting for within-pregnancy clustering. While this approach allowed us to evaluate outcomes specific to each neonate, we acknowledge that residual correlation between siblings may persist.
Conclusion
Our study demonstrates that chorionicity plays a critical role in determining outcomes in triplet pregnancy. Nontrichorionic pregnancies are associated with an increased risk for preterm birth, postpartum hemorrhage, lower birth weights, and higher rates of NICU admissions. These findings highlight the importance of early chorionicity assessment, accurate prenatal counselling, and the implementation of tailored prenatal surveillance strategies to optimize maternal and neonatal outcomes.
Authorship contribution
Oumaima Ammar was involved in data collection, methodology, analysis, and drafting of the manuscript. Mariarosaria Di Tommaso and Viola Seravalli contributed to the conceptualization and supervision of the study. Beatrice Baldassari, Mor Huri, and Serena Lucarelli contributed to data acquisition and critical review of the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics statement
Not applicable