Introduction
Craniospinal irradiation (CSI) is a technique used to treat the entire brain and spinal cord, with challenges in delivering a uniform dose distribution due to the long craniospinal axis. Traditional approaches, such as three-dimensional conformal radiation therapy (3D-CRT), use moving junctions between fields to prevent hot and cold spots but still result in inhomogeneous dose distribution along the spine. Hadley et al. Reference Hadley and Ding1 compared the conventional junction shift and gradient junction techniques, finding that the gradient method improves dose conformity and reduces hot spots and organs-at-risk (OARs) dose. Based on these findings, King Chulalongkorn Memorial Hospital has adopted volumetric-modulated arc therapy (VMAT) with low gradient junction shift and intensity-modulated proton therapy (IMPT), which both offer better conformity and no junction shift between fractions. Moreover, Majer et al. Reference Majer, Ambrožová and Davídková2 evaluated the out-of-field doses in pediatric CSI treatments using 3D-CRT, VMAT and proton therapy. They found that proton therapy offers reduced normal tissue dose and better conformity than photon techniques.
Traditionally, CSI patients at our centre were treated using the TrueBeam (TB) C-arm linear accelerator (LINAC) (Varian Medical Systems, Palo Alto, CA) and occasionally the ProBeam proton system (Varian Medical Systems, Palo Alto, CA). However, in 2023 and 2024, our centre acquired the new Halcyon (HAL) ring gantry (Varian Medical Systems, Palo Alto, CA) introduced in 2017. Since its introduction, various studies have explored Halcyon-based CSI VMAT, but the findings have been inconsistent. For instance, Sarkar et al. Reference Sarkar, Biswal and Shahid3 have shown that Halcyon-based CSI VMAT provides improved OAR sparing and reduced dose spill compared to TB. In contrast, Stroubinis et al. Reference Stroubinis, Psarras and Zygogianni4 have found similar results between the two systems. Our previous study Reference Buranavanitvong, Plangpleng and Sanghangthum5 found that TB plans had better dose coverage and OAR sparing, while Halcyon plans showed better treatment time and total normal tissue volume (TNTV) dose. Lastly, studies comparing various dosimetric parameters to the IMPT technique have been limited to C-arm LINACs or other systems. Thus, this study aims to compare dosimetric outcomes from the TB, Halcyon and IMPT systems for CSI treatments to explore the potential of the Halcyon machine as an alternative for treating CSI patients.
Methods
Patient selection criteria
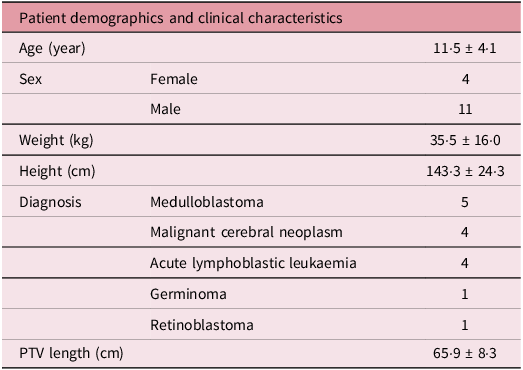
Based on our previous study, an additional five craniospinal irradiation (CSI) patients were included, resulting in a total of fifteen patients, all selected using the same criteria. Reference Buranavanitvong, Plangpleng and Sanghangthum5 The patient demographics and clinical characteristics are presented in Table 1.
Table 1. The 15 patient demographics and clinical characteristics

Contouring
The CT images were imported into the Eclipse Treatment Planning System (TPS). The clinical target volume (CTV), planning target volume (PTV), 16 OARs and TNTV were contoured following the same method as in the previous study. Reference Buranavanitvong, Plangpleng and Sanghangthum5 However, the PTV was not defined for IMPT plans. Instead, robust optimisation parameters were directly applied to the CTV, and the TNTV was delineated by subtracting the CTV from the body contour, unlike in VMAT plans, where the TNTV was based on the PTV, to assess the dose delivered to normal tissue outside the target volume.
Treatment planning
The VMAT plans were performed on TB, Halcyon and IMPT plans were created on ProBeam for each patient with the prescription dose of PTV in the VMAT plan, while CTV in the IMPT plan in 23·4 Gy, 1·8 Gy per fraction, 13 fractions.
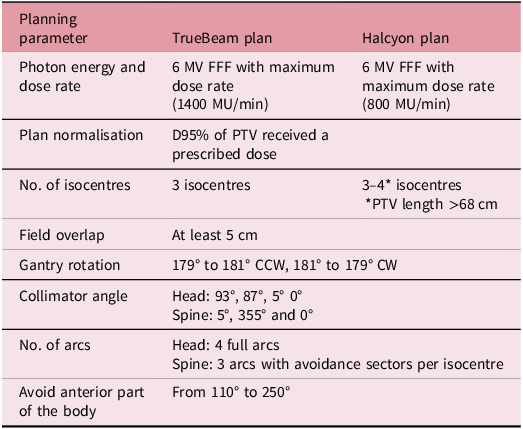
For the 30 VMAT plans, the treatment planning methodology followed our previous study, Reference Buranavanitvong, Plangpleng and Sanghangthum5 as summarised in Table 2. The arc arrangements are illustrated in Figure 1(a) and (b).

Figure 1. Arc arrangement on TrueBeam plan (a), Halcyon plan (b) and ProBeam plans (c).
Table 2. The treatment planning parameters of VMAT plans

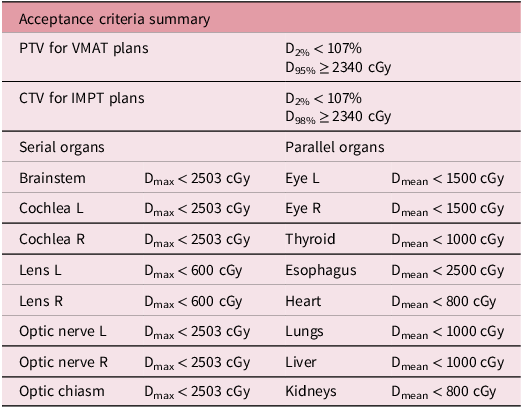
All photon plans were optimised using the same dose constraints. Then, the plans were fine-tuned through trade-offs or converted dose to structure until they met all the acceptance criteria shown in Table 3, aiming to minimise planner bias. The acceptance criteria used in this study were the clinical goals established at our institution. Dose constraints for serial organs were adjusted by lowering the maximum dose criteria to align with the prescribed dose, as no phase boost was applied.
Table 3. Acceptance criteria of target and OARs

For the 15 IMPT plans, the posteroanterior beams were applied in each isocentre with a field overlap of at least 6 cm, as shown in Figure 1(c). The range shifter and air gap were set at 5 cm and 8 cm, respectively. All proton plans were optimised using the same dose constraints. The robust optimisation was set with 5 mm setup uncertainty and 3·5% range uncertainty in 18 scenarios on the CTV structure and some OARs if they did not pass the clinical goal criteria, as shown in Table 3. The sufficient CTV coverage of the plans will be evaluated in all 18 scenarios, and the plans were normalised 98% of the CTV received the prescribed dose.
Plan evaluation
The photon and proton treatment plans were evaluated at D95%, D50%, D2%, conformity index (CI) and homogeneity index (HI) of CTV, the percentage of TNTV dose in 1, 2, 5, 22·23 and 23·4 Gy, the OARs dose in 0·2 cc dose (D0.2cc) for 8 serial organs and mean dose (Dmean) for 8 parallel organs and beam on time.
The CI was calculated according to Paddick’s CI Formula as follows (TVRI: the target volume (CTV) covered by the prescribed isodose line, TV: target volume and VRI: target volume of receiving the prescription dose). Reference Paddick6
The HI was calculated according to ICRU 83 as follows. 7
The paired t-test and analysis of variance were performed using SPSS version 30·0 for Windows. Statistical significance was defined at p < 0·05.
Patient-specific quality assurance (PSQA) plan
The verification plans of the CSI treatment plans were created for patient-specific quality assurance (PSQA) on each machine. For the VMAT plans, the electronic portal imaging device (EPID) was used in TB plans. The gantry and collimator were set at 0°, and the couch was set vertically, longitudinally and laterally at 10, 20 and 0 cm, respectively. The EPID was set at 100 cm source to detector distance and was calibrated before utilisation. However, for the Halcyon plans, the gantry and collimator were set at 0°, the couch was set outside the gantry and the source-imager distance was set at 154 cm. After that, in both TB and Halcyon plans, the device was irradiated based on the treatment plan to generate the composite image, which was used to obtain the measured portal dose image for evaluation with portal dosimetry software.
For the IMPT plans, the PTW Octavius detector array was used. A solid phantom with depths of 10 cm and 5 cm was placed beneath the detector to simulate full backscatter and above the detector to measure the dose at the centre of the CTV, respectively. The couch was positioned at 0 cm vertically, 100 cm longitudinally and 0 cm laterally. Before the measurement, the detector array was calibrated and irradiated based on the treatment plan, which was split into three plans (brain, upper spine and lower spine) for each patient. The results were then analysed using PTW software.
The results of all treatment plans were evaluated using gamma-passing rate criteria, as outlined in AAPM TG 218. Reference Miften, Olch and Mihailidis8 A gamma index of 3% dose difference (DD)/2 mm distance to agreement (DTA) was applied, with a 10% low dose threshold and a tolerance limit at a 95% passing rate. Both global normalisation and absolute evaluation methods were used. This evaluation method aims to analyse the difference between the calculated dose in the TPS and the measured dose to ensure that the treatment plans are suitable for patient care only.
Results
Dose coverage in CTV, CI and HI
The dose coverage in CTV on treatment plans from different machines is shown in Figure 2.

Figure 2. The dose coverage in (a) TrueBeam plans, (b) Halcyon plans and (c) ProBeam plans.
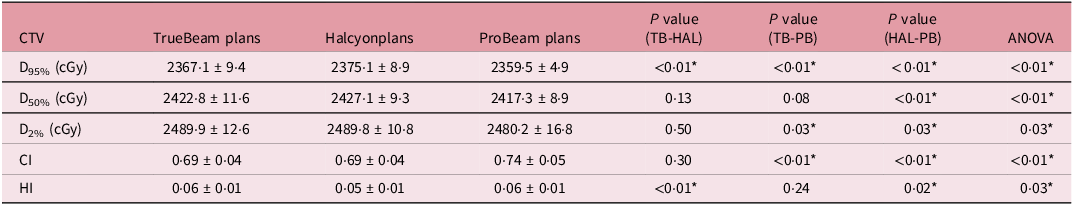
Table 4 shows the average dosimetric parameters for the target across the plans. Significant differences in D95% are observed between the plans. The ProBeam plans demonstrate superior CI, while the Halcyon plans show slightly better in the HI, with a significant difference.
Table 4. The average dose coverage, CI and HI for the target in VMAT plans on TrueBeam and Halcyon and IMPT plans on ProBeam

* For statistically significant values at a level of p < 0·05.
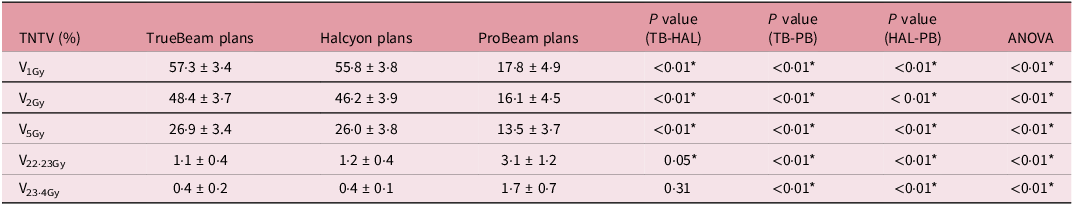
TNTV dose
In comparing the dose outside the PTV for VMAT plans and the CTV for IMPT plans, IMPT plans had the lowest average percentage of volume receiving low doses, followed by Halcyon and TB plans, with significant differences demonstrated in Table 5.
Table 5. The average TNTV dose in VMAT plans on TrueBeam and Halcyon and IMPT plans on ProBeam

* For statistically significant values at a level of p < 0·05.
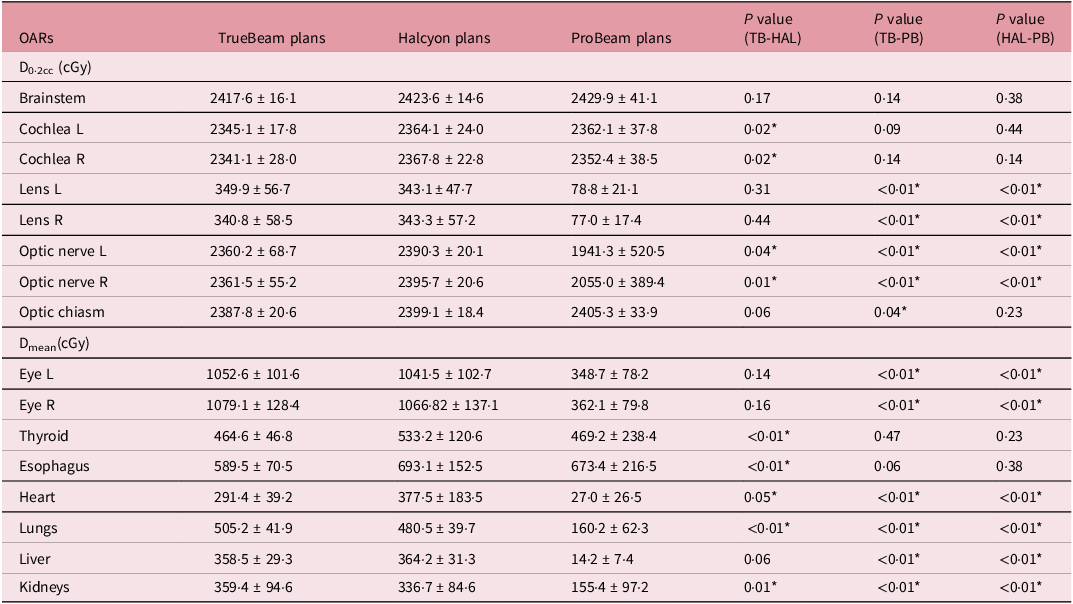
OARs dose
Table 6 shows that the ProBeam plan provided lower doses to 10 OARs compared to other plans. Among the VMAT plans, TB achieved lower doses to 11 OARs than Halcyon, with significant differences in 7 organs: cochlea L, cochlea R, optic nerve L, optic nerve R, thyroid, esophagus and heart.
Table 6. The average OARs dose in VMAT plans on TrueBeam and Halcyon and IMPT plans on ProBeam

* For statistically significant values at a level of p < 0·05.
Beam on time
The ProBeam plans had the shortest beam-on time, averaging 4·2 ± 0·1 minutes, followed by the Halcyon plans at 6·1 ± 0·8 minutes and the TB plans at 12·1 ± 0·5 minutes. However, ProBeam plans required a higher average total MU compared to the other plans. Specifically, the average MU for ProBeam was 15822·3 ± 21172·9 MU, while TB and Halcyon plans had average MUs of 1407·4 ± 116·8 MU and 1517·7 ± 315·3 MU, respectively.
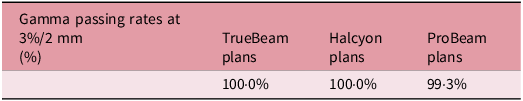
PSQA
All plans met the acceptance criteria, and the average percentage of gamma passing rate for each plan is presented in Table 7. The PSQA results demonstrated that all plans passed the 95% passing rate tolerance limit. Thus, all plans can be used to treat the patients.
Table 7. The mean value of the percentage gamma passing rate in VMAT plans on TrueBeam and Halcyon and IMPT plans on ProBeam

Discussion
This dosimetric comparison study evaluated the quality, dose outside the target, OAR sparing and beam-on time of VMAT Halcyon plans compared to VMAT TB and IMPT ProBeam plans. The ProBeam plans demonstrated the best dose coverage, as indicated by D95%, D50%, D2% and CI, with significant differences consistent with Mizuno et al. Reference Mizuno, Tomita and Takaoka9 who found that IMPT plans showed higher conformity but lower homogeneity. Similarly, our findings showed VMAT Halcyon plans had slightly better HI than TB plans. For both VMAT plans, significant differences in D95% and HI were observed, while D50%, D2% and CI showed no significant differences, aligning with Stroubinis et al. Reference Stroubinis, Psarras and Zygogianni4 TB plans had slightly better dose coverage than Halcyon, consistent with Peteoccia et al., Reference Petroccia, Malajovich and Barsky10 though Halcyon plans showed slightly better dose homogeneity, in agreement with Pokhrel et al. Reference Pokhrel, Webster and Mallory11
In terms of dose outside the target, IMPT plans had lower low-dose areas (1, 2 and 5 Gy) than Halcyon and TB, but delivered higher doses at 95% of the prescribed dose (Table 5), consistent with Seravalli et al., Reference Seravalli, Bosman and Lassen-Ramshad12 who noted proton plans reduced the TNTV dose. The TNTV dose in Halcyon plans was lower than in TB due to the dual-layer stacked MLC in Halcyon, which reduces leakage outside the target, as noted by Li et al. Reference Li, Scheuermann and Lin13,Reference Li, Irmen and Liu14 and in our earlier study. Reference Buranavanitvong, Plangpleng and Sanghangthum5 Reducing low-dose irradiation outside the target volume may contribute to a lower risk of radiation-induced second malignancies, an important consideration for pediatric patients who have a long remaining lifespan.
Regarding OAR sparing, IMPT plans showed superior OAR sparing, consistent with studies by Mizuno et al., Reference Mizuno, Tomita and Takaoka9 Seravalli et al. Reference Seravalli, Bosman and Lassen-Ramshad12 and others. Reference Whitaker, Routman and Schultz15–Reference Adeberg, Harrabi and Bougatf17 Whitaker et al. Reference Whitaker, Routman and Schultz15 found IMPT reduced doses to surrounding tissues, while Mirandola et al. Reference Mirandola, Colombo and Cavagnetto16 and Adeberg et al. Reference Adeberg, Harrabi and Bougatf17 reported similar reductions in paediatric neuroblastoma and intracranial tumour patients. Comparing Halcyon and TB, TB showed lower doses in 11 of 16 OARs, with significant differences in cochlea L, cochlea R, optic nerve L, optic nerve R, thyroid, esophagus and heart. The superior sparing in TB is attributed to jaw tracking, as described in our previous study. Reference Buranavanitvong, Plangpleng and Sanghangthum5 Halcyon plans showed lower doses in two parallel organs (lungs and kidneys), consistent with Sarkar et al. Reference Sarkar, Biswal and Shahid3 In our study, 7 out of 15 Halcyon plans required 4 isocentres, whereas TB used 3 due to field size limitations. Thus, Halcyon plans may cause more scatter and higher total MU, as noted by Sarkar et al. Reference Sarkar, Biswal and Shahid3 and Pokhrel et al. Reference Pokhrel, Webster and Mallory11 Despite this, both plans met OAR sparing criteria.
Nevertheless, the Halcyon machine’s advantages led to half the beam-on times compared to TB, enhancing treatment efficiency. Reference Buranavanitvong, Plangpleng and Sanghangthum5 Conversely, IMPT plans had shorter beam-on times due to fewer fields. However, when considering the overall treatment time, they may take longer because of the need for multiple CBCT scans. In contrast, both Halcyon and TB require only one CBCT scan per positioning. The reduction of treatment time in Halcyon may improve the efficiency of treatment delivery because of decreased patient motion during treatment and reduce anesthesia requirements, particularly in pediatric patients capable of tolerating treatment. Nonetheless, our limitation of this study is that the planning time was not evaluated, which may reflect both the relative complexity of each plan.
Conclusion
This dosimetric comparison demonstrates that IMPT provides the best plan quality. However, due to the limited availability of proton therapy machines, treatment delays may arise. Between the two VMAT plans, TB offers superior dose coverage and OAR sparing, especially for serial organs. Nevertheless, our findings indicate that Halcyon can provide sufficient plan quality in high dose homogeneity and OARs sparing, better in terms of TNTV at low doses and shorter beam-on time. Thus, for clinics equipped with both TB C-arm LINAC and Halcyon machines, Halcyon can serve as an alternative treatment option for CSI patients. If a centre already has only Halcyon machine and needs to perform CSI, there is no need to refer patients to another centre. This not only enables faster treatment but also reduces travel costs for patients.
Data available statement
All essential data supporting the conclusions of this study, including beam arrangements, dose constraints and planning techniques for VMAT and IMPT in craniospinal irradiation (CSI) cases, are described in detail within the manuscript. Due to patient confidentiality and institutional policies, raw patient-specific data are not publicly available due to privacy and institutional restrictions, but de-identified data may be available from the corresponding author upon reasonable request and with approval from the institutional ethics committee.
Acknowledgements
We would like to thank physicists of the Division of Radiation Oncology, Department of Radiology, King Chulalongkorn Memorial Hospital.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
The researchers declare that there are no affiliations with any companies.
Ethical approval
This retrospective study was approved by the Institutional Review Board of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (IRB No. 0532/67). All data were anonymised before analysis.
Patient consent statement
Not applicable.
Permission to reproduce material from other sources
Not applicable.
Clinical trial registration
Not applicable.