This volume is the result of a long-term collaboration by an international consortium of mental health researchers from over two dozen countries who participated in the World Mental Health (WMH) surveys. The WMH initiative is a coordinated series of epidemiological surveys conducted throughout the world that are designed to provide a comprehensive global portrait of the prevalence, risk factors, and consequences of common mental disorders. WMH survey results, which have been reported in numerous papers in leading scientific journals, have served as the basis for five previous books published by Cambridge University Press. The first volume in this series focused on the descriptive epidemiology of mental disorders (Kessler & Üstün, Reference Kessler and Üstün2008), the second on mental–physical comorbidity (Von Korff et al., Reference Von Korff, Scott and Gureje2009), the third on suicidal behaviors (Nock et al., Reference Nock, Borges and Ono2012), the fourth on the burdens of mental disorders (Alonso et al., Reference Alonso, Chatterje and He2013) and the fifth on facts about mental disorders around the world (Scott et al., Reference 12Scott, de Jonge, Stein and Kessler2018). The current volume addresses trauma and posttraumatic stress disorder (PTSD).
A Brief History of PTSD
The symptoms of PTSD have been recognized since the beginnings of recorded history, as exemplified by Homer's epic poem, The Iliad (Shay, Reference Shay1994). However, PTSD was not fully acknowledged as a unique diagnostic entity until the publication of the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) (American Psychiatric Association, 1980). DSM-III defined PTSD as a set of re-experiencing, avoidance, and hyper-arousal symptoms in the wake of a trauma that was “outside the range of normal human experience.” The DSM-III conceptualization, which was more inclusive than the acute stress reaction categories in DSM-I (American Psychiatric Association, 1952) and DSM-II (American Psychiatric Association, 1968), was influenced by a growing body of evidence about the distinctive features and comorbidity of posttraumatic symptoms in active-duty soldiers (Moskos, Reference Moskos1975), veterans (Kardiner & Spiegel, Reference Kardiner and Spiegel1947; Figley, 1978; Helzer et al., Reference Helzer, Robins, Wish and Hesselbrock1979), prisoners of war (Strassman et al., Reference Strassman, Thaler and Schein1956), as well as in other trauma-exposed groups, such as Holocaust victims (Klein, Reference Klein1971), atomic bomb survivors (Lifton, Reference Lifton1967), and women subjected to child sexual abuse (Herman & Hirschman, Reference Herman and Hirschman1977), rape (Burgess & Holmstrom, Reference Burgess and Holmstrom1974), and physical assault (Walker, Reference Walker1979). DSM-III assumed that PTSD was rare, and early epidemiological studies, which assessed trauma with two open-ended stem questions, reported lifetime prevalence rates of 1% to 3% (Shore et al., Reference Shore, Tatum and Vollmer1986; Helzer et al., Reference Helzer, Robins and McEvoy1987; Davidson et al., Reference Davidson, Hughes, Blazer and George1991). The low rates later proved to be underestimates, but the reported correlations of female sex, childhood trauma, and suicidality with DSM-III PTSD were consistently confirmed in later studies.
DSM-III-R (American Psychiatric Association, 1987), together with newly developed trauma checklists (Wolfe & Kimerling, Reference Wolfe, Kimerling, Wilson and Keane1997), facilitated epidemiological research on PTSD by clearly elucidating the nature of qualifying traumas, clarifying the required symptoms, and specifying a minimum duration for the diagnosis (Brett et al., Reference Brett, Spitzer and Williams1988). DSM-IV (American Psychiatric Association, 1994) later reformulated the definition of trauma to include experiencing or witnessing events that involved actual or threatened death or serious injury or a threat to the physical integrity of self or others. Indeed, these revised criteria stimulated a new generation of epidemiological and public health research on PTSD in both general populations (Resnick et al., Reference Resnick, Kilpatrick, Danksy, Saunders and Best1993; Finkelhor, Reference Finkelhor1994; Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995) and in vulnerable groups (e.g., Kulka et al., Reference Kulka, Schlenger and Fairbanks1990; Zerach et al., Reference Zerach, Solomon, Cohen and Ein-Dor2013). While ICD-10 also introduced PTSD as a separate diagnosis (Janca et al., Reference Janca, Üstün and Sartorius1994), most epidemiological studies of PTSD have been based on DSM criteria (Gradus, Reference Gradus2017). Finally, DSM-5 (American Psychiatric Association, 2013) added behavioral symptoms and a fourth symptom cluster involving negative cognition and mood, and recent studies are operationalizing PTSD using these new criteria.
Epidemiology of Trauma and PTSD
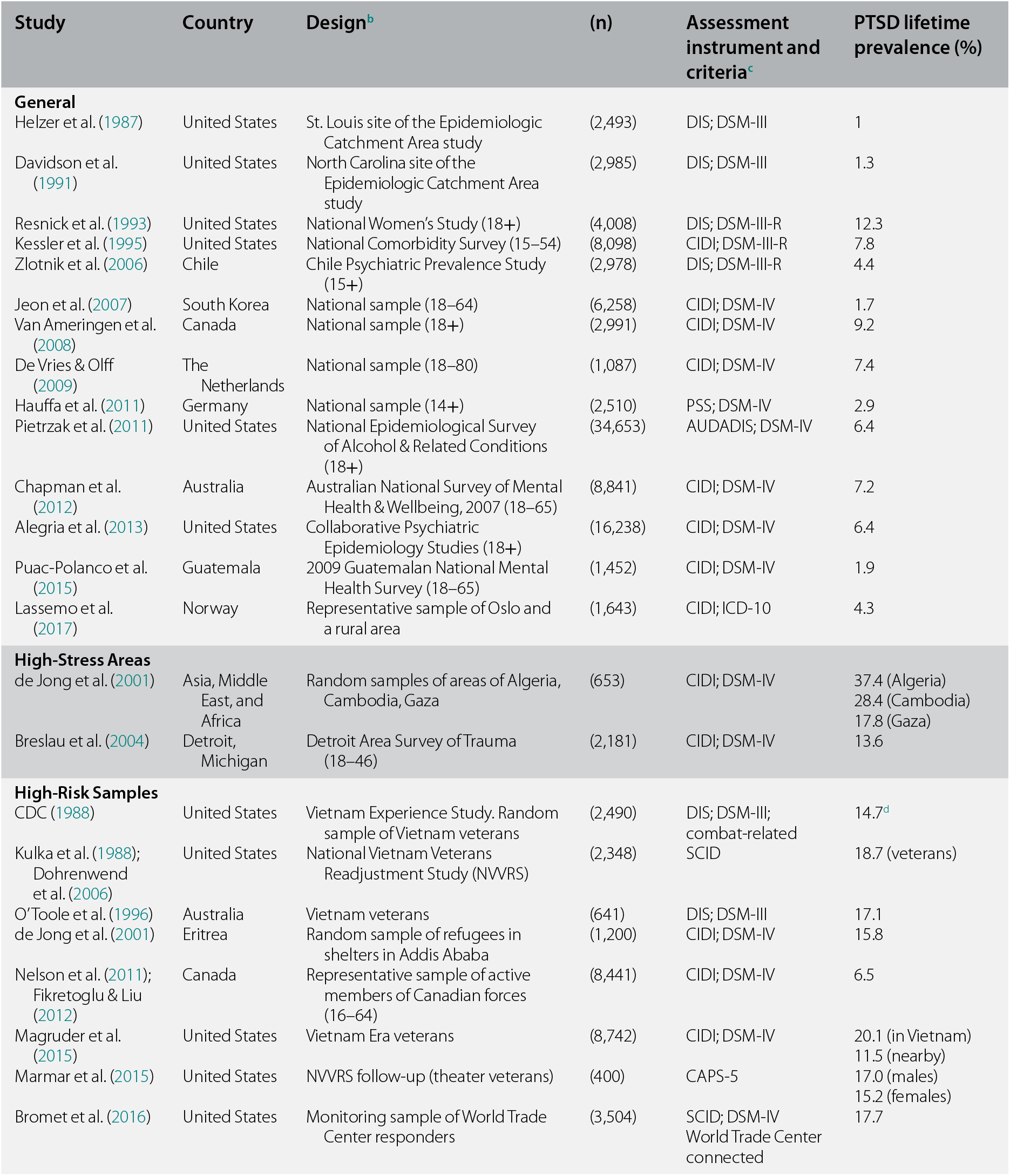
Since the publication of DSM-III, a number of epidemiological studies of trauma and PTSD have been conducted in North America and Europe. In contrast, far fewer epidemiological studies have been conducted in other countries and regions of the world. This chapter summarizes findings from surveys that examined lifetime PTSD diagnoses in representative samples drawn from the general population, high-risk regions of the world, and vulnerable groups, such as veterans. (Studies based on symptom checklists or child/adolescent samples are not considered here.) These surveys all use the respondent-selected worst or most stressful trauma as the focal trauma.
Table 1.1 provides examples of widely cited surveys of trauma and PTSD that took place primarily in select high-income countries. The WMH survey findings reported in this book thus fill in a large gap in knowledge about the global epidemiology of trauma and PTSD.
Table 1.1 Major epidemiological surveys of PTSD based on worst lifetime trauma as the focal traumaa
| Study | Country | Designb | (n) | Assessment instrument and criteriac | PTSD lifetime prevalence (%) |
|---|---|---|---|---|---|
| General | |||||
| Helzer et al. (Reference Helzer, Robins and McEvoy1987) | United States | St. Louis site of the Epidemiologic Catchment Area study | (2,493) | DIS; DSM-III | 1 |
| Davidson et al. (Reference Davidson, Hughes, Blazer and George1991) | United States | North Carolina site of the Epidemiologic Catchment Area study | (2,985) | DIS; DSM-III | 1.3 |
| Resnick et al. (Reference Resnick, Kilpatrick, Danksy, Saunders and Best1993) | United States | National Women's Study (18+) | (4,008) | DIS; DSM-III-R | 12.3 |
| Kessler et al. (Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995) | United States | National Comorbidity Survey (15–54) | (8,098) | CIDI; DSM-III-R | 7.8 |
| Zlotnik et al. (Reference Zlotnik, Johnson and Kohn2006) | Chile | Chile Psychiatric Prevalence Study (15+) | (2,978) | DIS; DSM-III-R | 4.4 |
| Jeon et al. (Reference Jeon, Suh and Lee2007) | South Korea | National sample (18–64) | (6,258) | CIDI; DSM-IV | 1.7 |
| Van Ameringen et al. (Reference Van Ameringen, Mancini, Patterson and Boyle2008) | Canada | National sample (18+) | (2,991) | CIDI; DSM-IV | 9.2 |
| De Vries & Olff (Reference de Vries and Olff2009) | The Netherlands | National sample (18–80) | (1,087) | CIDI; DSM-IV | 7.4 |
| Hauffa et al. (Reference Hauffa, Rief and Brähler2011) | Germany | National sample (14+) | (2,510) | PSS; DSM-IV | 2.9 |
| Pietrzak et al. (Reference Pietrzak, Goldstein, Southwick and Grant2011) | United States | National Epidemiological Survey of Alcohol & Related Conditions (18+) | (34,653) | AUDADIS; DSM-IV | 6.4 |
| Chapman et al. (Reference Chapman, Mills and Slade2012) | Australia | Australian National Survey of Mental Health & Wellbeing, 2007 (18–65) | (8,841) | CIDI; DSM-IV | 7.2 |
| Alegria et al. (Reference Alegria, Fortuna and Lin2013) | United States | Collaborative Psychiatric Epidemiology Studies (18+) | (16,238) | CIDI; DSM-IV | 6.4 |
| Puac-Polanco et al. (Reference Puac-Polanco, Lopez-Soto and Kohn2015) | Guatemala | 2009 Guatemalan National Mental Health Survey (18–65) | (1,452) | CIDI; DSM-IV | 1.9 |
| Lassemo et al. (Reference Lassemo, Sandanger, Nygard and Sorgaard2017) | Norway | Representative sample of Oslo and a rural area | (1,643) | CIDI; ICD-10 | 4.3 |
| High-Stress Areas | |||||
| de Jong et al. (Reference de Jong, Komproe and Van Ommeren2001) | Asia, Middle East, and Africa | Random samples of areas of Algeria, Cambodia, Gaza | (653) | CIDI; DSM-IV | 37.4 (Algeria) 28.4 (Cambodia) 17.8 (Gaza) |
| Breslau et al. (Reference Breslau, Peterson, Poisson, Schultz and Lucia2004) | Detroit, Michigan | Detroit Area Survey of Trauma (18–46) | (2,181) | CIDI; DSM-IV | 13.6 |
| High-Risk Samples | |||||
| CDC (1988) | United States | Vietnam Experience Study. Random sample of Vietnam veterans | (2,490) | DIS; DSM-III; combat-related | 14.7d |
| Kulka et al. (Reference Kulka, Schlenger and Fairbank1988); Dohrenwend et al. (Reference Dohrenwend, Turner and Turse2006) | United States | National Vietnam Veterans Readjustment Study (NVVRS) | (2,348) | SCID | 18.7 (veterans) |
| O'Toole et al. (Reference O'Toole, Marshall and Grayson1996) | Australia | Vietnam veterans | (641) | DIS; DSM-III | 17.1 |
| de Jong et al. (Reference de Jong, Komproe and Van Ommeren2001) | Eritrea | Random sample of refugees in shelters in Addis Ababa | (1,200) | CIDI; DSM-IV | 15.8 |
| Nelson et al. (Reference Nelson, Cyr and Corbett2011); Fikretoglu & Liu (Reference Fikretoglu and Liu2012) | Canada | Representative sample of active members of Canadian forces (16–64) | (8,441) | CIDI; DSM-IV | 6.5 |
| Magruder et al. (Reference Magruder, Serpi and Kimerling2015) | United States | Vietnam Era veterans | (8,742) | CIDI; DSM-IV | 20.1 (in Vietnam) 11.5 (nearby) |
| Marmar et al. (Reference Marmar, Schlenger and Henn-Haase2015) | United States | NVVRS follow-up (theater veterans) | (400) | CAPS-5 | 17.0 (males) 15.2 (females) |
| Bromet et al. (Reference Bromet, Hobbs and Clouston2016) | United States | Monitoring sample of World Trade Center responders | (3,504) | SCID; DSM-IV World Trade Center connected | 17.7 |
a Data from Lowe, S. R., Blachman-Forshay, J., & Koenen, K. C. (2015). Trauma as a public health issue: epidemiology of trauma and trauma-related disorders. In U. Schnyder & M. Cloitre, eds., Evidence Based Treatments for Trauma-Related Psychological Disorders: A Practical Guide for Clinicians. Cham, Switzerland: Springer International Publishing, pp. 11–40.
b Age in parenthesis.
c DIS is the Diagnostic Interview Schedule; AUDADIS is the Alcohol Use Disorders and Associated Disabilities Interview Schedule; SCID is the Structured Clinical Interview for DSM; PSS is the PTSD Symptom Scale; CAPS is the Clinician Administered PTSD Scale.
d Total prevalence not reported; value represents trauma with highest prevalence.
The first comprehensive study of trauma and PTSD in the general population was the highly influential National Comorbidity Survey (NCS), conducted in the United States in 1990–2 (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995). The NCS was a nationwide, in-person survey of 8,098 adults aged 15–54 who were administered a modified version of the Composite International Diagnostic Interview (CIDI). The CIDI inquired about 12 DSM-III-R-qualifying traumas (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995). To minimize embarrassment and stigma, the traumas were presented to respondents in a booklet and were asked about by number (“Did you ever experience event number 1 on the list?”). More than half of the sample (60.7% of men and 51.2% of women) reported exposure to at least one trauma, and the majority endorsed two or more. Comparable rates of lifetime trauma exposure have subsequently been found in other studies assessing a similar number of traumas, including research conducted in Kenya (48.2%, Jenkins et al., Reference Jenkins, Otheieno and Omollo2015), the Netherlands (52.2%, Bronner et al., Reference Bronner, Peek and Vries2009), and Australia (57.2%, Rosenman, Reference Rosenman2002). However, rates have varied from less than 30% in Germany (Maercker et al., Reference Maercker, Forstmeier, Wagner, Glaesmer and Brähler2008) and South Korea (Jeon et al., Reference Jeon, Suh and Lee2007) to more than 70% in Mexico (Norris et al., Reference Norris, Murphy and Baker2003), Canada (Stein et al., Reference Stein, Walker, Hazen and Forde1997), and Portugal (Albuquerque et al., Reference Albuquerque, Soares, De Jesus and Alves2003). In contrast, studies that used longer trauma lists (20+ traumas) have typically found lifetime exposure rates of 75% to 85%. Examples include national surveys in Australia (Mills et al., Reference Mills, McFarlane and Slade2011), Canada (Van Ameringen et al., Reference Van Ameringen, Mancini, Patterson and Boyle2008), and the Netherlands (de Vries & Olff, Reference de Vries and Olff2009), as well as regional surveys in Detroit, Michigan (Breslau et al., Reference Breslau, Kessler and Chilcoat1998; Goldmann et al., Reference Goldmann, Aiello and Uddin2011). The most commonly reported traumas were unexpected death of a loved one, motor vehicle collisions, and being mugged (Norris, Reference Norris1992; Breslau et al., Reference Breslau, Kessler and Chilcoat1998; Roberts et al., Reference Roberts, Gilman, Breslau, Breslau and Koenen2011). Overall, the most consistent risk factors for trauma exposure include younger age, male sex, lower socioeconomic status, and a history of prior traumas (Hatch & Dohrenwend, Reference Hatch and Dohrenwend2007; Shalev et al., Reference Shalev, Liberzon and Marmar2017). Some traumas, such as severe motor vehicle collisions, appear to be more prevalent in high-income countries than in developing countries (World Health Organization, 2016). Cross-national comparisons of the rates and risk factors for specific trauma exposures in the WMH cohorts are explored in Chapters 3 and 4 as well as in Section 4 of this volume.
In addition to examining exposure to trauma, the NCS provided the first systematic portrait of the descriptive epidemiology of PTSD associated with respondents’ most upsetting (i.e., worst) trauma. The lifetime rate of PTSD was 7.8% overall, ranking it lower than major depression (17.1%) but considerably higher than panic disorder (3.5%) and bipolar disorder (1.7%) (Kessler et al., Reference Kessler, McGonagle and Zhao1994). Other US general population surveys of lifetime PTSD after respondent-nominated worst trauma have found similar rates of PTSD (e.g., Roberts et al., Reference Roberts, Gilman, Breslau, Breslau and Koenen2011; Alegria et al., Reference Alegria, Fortuna and Lin2013; Breslau et al., Reference Breslau, Troost, Bohnert and Luo2013) as did surveys conducted in the Netherlands (de Vries & Olff, Reference de Vries and Olff2009) and Canada (Van Amerigen et al., Reference Van Ameringen, Mancini, Patterson and Boyle2008). Of note, two national surveys found considerably lower rates of PTSD for respondents’ most stressful event – namely, Zlotnik et al. (Reference Zlotnik, Johnson and Kohn2006), which reported 4.4% in Chile and Jeon et al. (Reference Jeon, Suh and Lee2007), which reported 1.7% in South Korea. As expected, regional studies of high-conflict areas have reported higher rates of PTSD than national surveys. Examples include the 13.6% rate of PTSD in the Detroit Area Survey of Trauma (Breslau et al., Reference Breslau, Peterson, Poisson, Schultz and Lucia2004) and the high rates found by de Jong et al. (Reference de Jong, Komproe and Van Ommeren2001) in Algeria (37.4%), Cambodia (28.9%), and Gaza (15.8%). Studies of high-risk samples, such as active-duty soldiers, veterans, and first-responders, most of which were conducted in high-income countries, have also reported rates that are higher (e.g., 17–20%) than those found in general population samples.
The lifetime risk of PTSD in conjunction with specific traumas (i.e., the conditional probability of PTSD) has been shown to vary widely, depending on the type of trauma (Shalev et al., Reference Shalev, Liberzon and Marmar2017). In the NCS, the rates of PTSD in men for respondent-nominated worst trauma ranged from 1.8% (physical attack) to 65.0% (rape), while in women, the range was 5.4% (natural disaster) to 48.5% (physical abuse) (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995). In the Detroit Area Survey of Trauma, the trauma-specific rates of PTSD also ranged widely, with rates varying from a low of 1.5% (learning that a relative was attacked) to a high of 62.0% (being held captive/tortured/kidnapped) (Breslau et al., Reference Breslau, Peterson, Poisson, Schultz and Lucia2004). Overall, the severity of the threat associated with the trauma is strongly linked to the risk of PTSD. In line with this body of research, this volume reports the conditional risks of PTSD after 29 trauma types for survey participants residing in both high- and low-income countries. As discussed later in this chapter, the trauma for which PTSD was evaluated was a randomly selected trauma rather than the respondent-nominated worst trauma.
Various personal risk factors have also been shown to be associated with an elevated likelihood of PTSD. Meta-analyses (Brewin et al., Reference Brewin, Andrews and Valentine2000; Ozer et al., Reference Ozer, Best, Lipsey and Weiss2003) and a systematic review of prospective studies of PTSD (DiGangi et al., Reference DiGangi, Gomez and Mendoza2013) have shown that cognitive ability, prior traumas, and history of psychopathology are among the most important risk factors for developing PTSD (Koenen et al., Reference Koenen, Moffitt, Poulton, Martin and Caspi2007; Scott et al., Reference Scott, Smith and Ellis2010; Breslau et al., Reference Breslau, Koenen and Luo2014). Demographic risk factors were also found to be associated with PTSD, especially female sex, younger age, being unmarried, lower socioeconomic status, and unemployment (Norris et al., Reference Norris, Kaniasty, Conrad, Inman and Murphy2002; Shalev et al., Reference Shalev, Liberzon and Marmar2017). Notably, research from high-income countries has repeatedly shown that men are more likely to experience a trauma, but once exposed, women are more likely to develop PTSD (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995; Breslau et al., Reference Breslau, Chilcoat, Kessler, Peterson and Lucia1999; Breslau, Reference 9Breslau2002).
Since the earliest epidemiological studies, PTSD has been shown to be highly comorbid with both other types of mental disorders and a wide range of physical health disorders. Mood, anxiety, and substance use disorders have all been reliably linked to PTSD in general population samples (e.g., Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995; Chilcoat & Breslau, Reference Chilcoat and Breslau1998; Breslau, Reference Breslau2009) and vulnerable groups (e.g., Kulka et al., Reference Kulka, Schlenger and Fairbanks1990; Smith et al., Reference Smith, Armelle, Boarts, Brazil and Delahanty2016). In a recent review, Flory and Yehuda (Reference Flory and Yehuda2015) noted that almost 50% of individuals with PTSD have comorbid depression. Similarly, McFarlane (Reference McFarlane2000) concluded that depression, anxiety, and substance use disorders accompany PTSD in the majority of cases. In general, prospective studies have also shown that preexisting psychopathology is a major risk factor for the development of PTSD after trauma exposure (Breslau, Reference 9Breslau2002; DiGangi et al., Reference DiGangi, Gomez and Mendoza2013; Smith et al., Reference Smith, Armelle, Boarts, Brazil and Delahanty2016), and longitudinal studies have shown that PTSD increases the risk of new onset psychiatric and substance use disorders (e.g., Breslau et al., Reference Breslau, Davis, Peterson and Schultz1997). PTSD is also comorbid with various physical health conditions (Eaton, Reference Eaton2006; Boscarino, Reference Boscarino2008; Von Korff et al., Reference Von Korff, Scott and Gureje2009; Miller & Sadeh, Reference Miller and Sadeh2014), particularly cardiovascular disease (Sumner et al., Reference Sumner, Kubranksy and Elkind2015; Edmonson & von Känel, Reference Edmonson and von Känel2017; Koenen et al., Reference Koenen, Sumner and Gilsanz2017) and chronic pain (Brennstuhl et al., Reference Brennstuhl, Tarquinio and Montel2015). In addition, preliminary evidence suggests that PTSD is also associated with signs of accelerated aging (Cohen et al., Reference Cohen, Neylan and Yaffe2013; Clouston et al., Reference Clouston, Kotov and Pietrzak2016; Roberts et al., Reference Roberts, Koenen and Chen2017; Wolf et al., 2017), dementia (Yaffe et al., Reference Yaffe, Vittinghoff and Lindquist2010; Flatt et al., 2017), and premature mortality (Lohr et al., Reference Lohr, Palmer and Eidt2015). There is also growing awareness that medical diagnoses, especially cardiovascular disease, cancer, and degenerative neurological diseases, can cause medical-related PTSD symptoms, which worsen prognosis by interfering with treatment adherence (e.g., Hobfoll et al., Reference Hobfoll, Gehart and Zaita2015; Edmonson & von Känel, Reference Edmonson and von Känel2017). The same gap in knowledge about the prevalence of trauma and PTSD and their respective risk factors applies to studies on the comorbidity of mental and physical conditions – namely, that to date, the research has by and large taken place only in high-income countries.
One of the most highly cited findings from the NCS was that a third of individuals with PTSD failed to remit after many years, even with treatment (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995). This result was subsequently confirmed in a population-based survey of Australia (Chapman et al., Reference Chapman, Mills and Slade2012), in which approximately one-third of respondents with PTSD continued to experience symptoms more than 30 years after onset. In addition, more than half of the remitted PTSD cases in the Australian cohort still experienced symptoms after 14 years. Recent meta-analyses of epidemiological and clinical samples have placed the average rate of chronicity at closer to 50% (Morina et al., Reference Morina, Wicherts, Lobbrecht and Priebe2014; Steinert et al., Reference Steinert, Hofmann, Leichsenring and Kruse2015). The Morina et al. (Reference Morina, Wicherts, Lobbrecht and Priebe2014) meta-analysis focused on prospective studies of clinical and community cases diagnosed with PTSD who had a minimum of 10 months of follow-up. Among the more than 80,000 participants, less than half (44.0%) were in remission at follow-up, although the range varied from 8% to 89%, depending on the trauma that triggered the PTSD, the length of the follow-up, and personal characteristics.
One of the most consistent findings in the literature is that women with PTSD are far more likely than men with PTSD to develop a chronic disorder. An early epidemiological study of 1,000 adults between 20 and 30 years of age found that the risk of chronicity in women was increased by a factor of four (Breslau & Davis, Reference Breslau and Davis1992). A partial explanation can be found in data from a national survey of American women in which PTSD chronicity was associated with reporting rape and physical assault before age 18 (Cougle et al., Reference Cougle, Resnick and Kilpatrick2009). Other risk factors for chronicity found in surveys in high-income countries include those associated with PTSD onset noted earlier (i.e., history of childhood adversities, history of prior traumas, preexisting psychopathology, and intensity of the current trauma) as well as adverse circumstances that occur in the immediate aftermath of the trauma, such as trauma-linked stressful life events, inadequate emotional and practical support, new onset of psychiatric and substance disorders, and physical injury and illness (Steinert et al., Reference Steinert, Hofmann, Leichsenring and Kruse2015).
Despite the chronicity and impairment attached to PTSD, the vast majority of affected individuals do not receive any treatment, and only a small minority receive evidence-based treatments, such as cognitive-behavioral therapy (CBT), selective-serotonin uptake inhibitors (SSRIs), and serotonin-norepinephrine reuptake inhibitors (SNRIs), or a combination therapy (Bisson et al., Reference Bisson, Roberts, Andrew, Cooper and Lewis2013). In the United States, where mental health services are much more available than in most other countries (Roberts et al., Reference Roberts, Gilman, Breslau, Breslau and Koenen2011), only about half of those with PTSD seek treatment, and only 58% of those seeking treatment receive care from a mental health professional (Kessler, Reference Kessler2000). It is worth noting that the rates of treatment for PTSD in the United States are consistent with the rates of mental health treatment for severe mental and substance use disorders in general (Kessler et al., Reference Kessler, Demler and Frank2005). As expected, ethnic minorities are less likely and women are more likely to receive treatment than Whites and men (Roberts et al., Reference Roberts, Gilman, Breslau, Breslau and Koenen2011). Relatively little is known about treatment-seeking by individuals with PTSD in developing countries – another gap investigated in the WMH surveys (Chapter 8).
Research has shown that early treatment in first-response settings can help prevent the onset of PTSD (Foa et al., Reference Foa, Hearst-Ikeda and Perry1995; Kearns et al., Reference Kearns, Ressler, Zatzick and Rothbaum2012; Shalev et al., Reference Shalev, Ankri and Israeli-Shalev2012). However, since a minority of trauma victims go on to develop PTSD (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995; Kessler, Reference Kessler2000; Roberts et al., Reference Roberts, Austin, Corliss, Vandemorris and Koenen2010, Reference Roberts, Gilman, Breslau, Breslau and Koenen2011), and a substantial proportion of acute cases recover spontaneously (Shalev et al., Reference Shalev, Liberzon and Marmar2017), researchers have been developing models to predict which individuals are most likely to develop PTSD and thus also most likely to benefit from expensive early interventions. One example is the PsySTART system adopted by the American Red Cross to target rapid delivery of psychological first aid and referral for mental health services to survivors judged to be at high risk of mental disorders in the immediate aftermath of a disaster (Schreiber et al., Reference Schreiber, Yin, Omaish and Broderick2014). PsySTART differs from previous post-disaster risk evaluation schemes by focusing on evidence-based predictors of PTSD (severity of exposure, prior traumas, and history of prior mental disorders) and acute suicidality, rather than on current distress. Recent data-mining approaches aimed at detecting patterns of behavior in large data sets are also being applied to identify the highest risk groups for developing PTSD in the wake of specific types of traumas. This approach is discussed in Chapter 22 using relevant data from both high- and low-income countries.
Dissecting the Clinical Picture
Given that a majority of individuals with PTSD do not seek treatment, especially within the mental health sector, and treatment-seeking is not random (Kessler et al., Reference Kessler, Demler and Frank2005), respondents with PTSD identified in general population surveys provide the least biased source of clinical information available for examining phenomenological and nosological issues (Cohen & Cohen, Reference Cohen and Cohen1984). One pressing issue best examined with epidemiological evidence involves differences in rates of PTSD across current criterion sets. As noted above, while most PTSD studies to date have been based on DSM-IV criteria, some European epidemiological studies have been based on ICD-10 criteria (e.g., Lassemo et al., Reference Lassemo, Sandanger, Nygard and Sorgaard2017). In addition, recent studies have begun to examine PTSD using DSM-5 criteria. Potential differences in prevalence as well as in clinical and demographic characteristics of individuals diagnosed according to these different criterion sets are a central concern not just for meta-analyses that compare results across epidemiological studies, but also for recent national and international multicenter genetic and neurobiological studies of PTSD. Such genome-wide association studies (Logue et al., Reference Logue, Amstadter and Baker2015) require massive sample sizes that are beyond the reach of a single research team. For example, the Psychiatric Genomics Consortium-Post-Traumatic Stress Disorder Working Group pools data globally to identify genes for PTSD. For the first pooled analysis, caseness was determined according to DSM-IV criteria as that was the criterion used in extant studies (Duncan et al., 2017). The specific instruments applied to diagnose PTSD caseness, however, varied across data sets. Moreover, future analyses will include PTSD diagnosed according to DSM-5, raising new challenges in terms of pooling phenotypes across studies. (Caseness based on symptom scale cut-points rather than gold standard diagnostic assessments presents another set of problems.) The CIDI was designed to make both ICD-10 and DSM-IV diagnoses and contains sufficient information to estimate DSM-5 and the likely features of ICD-11. Chapter 17 uses the WMH data to provide a rare glimpse into the relative prevalence and risk factors for PTSD based on different diagnostic criteria.
DSM-5 also eliminated the requirement that the trauma must immediately induce “fear, helplessness, or horror” (Criterion A2) in order to be considered a qualifying event. As noted above, this decision in DSM-5 is consistent with the Red Cross PsySTART risk criteria in which current distress is no longer a critical part of the triage process. The WMH surveys provided empirical evidence to the DSM-5 PTSD work group committee that supported the decision to remove the A2 criterion. These previously published findings (Karam et al., Reference Karam, Andrews and Bromet2010), which serve as the basis for Chapter 18, illustrate the value of large epidemiological data sets for assessing the utility of specific diagnostic criteria.
Many studies of trauma-exposed populations have focused on partial or subthreshold PTSD, but these studies have applied different operational definitions. The criteria for subthreshold PTSD include fully endorsing a specific number of symptom clusters, requiring fewer symptoms from each cluster, or the narrower approach, namely, focusing on symptoms that are unique to PTSD, such as re-experiencing symptoms (Maercker et al., Reference Maercker, Brewin and Bryant2013). Clearly, the rates of subthreshold PTSD will vary according to the strictness of the criteria applied. Thus, for epidemiological purposes, a consensus definition of subthreshold PTSD would enable examination of the rates, risk factors, and consequences of subthreshold PTSD across multiple investigations. The WMH surveys attempted to determine an optimal criterion set for defining subthreshold PTSD (Chapter 19). Further replication is required before the issue can be settled, but given the growing attention to subthreshold PTSD, it is critical that the field develop an empirically based consensus classification system.
Epidemiological evidence can also inform discussions about subtypes of PTSD, particularly the dissociative subtype and complex PTSD. A few studies have suggested that PTSD characterized by dissociative symptoms is underpinned by somewhat different neurobiological mechanisms from most other PTSD symptom constellations and that patients with the dissociative subtype may require different interventions (Lanius et al., Reference Lanius, Brand, Vermetten, Frewen and Spiegel2012). Similarly, the field has debated questions about the uniqueness of complex PTSD, a subtype characterized by dysfunction in self-organization or emotional regulation, with symptoms in the affective, self-concept, and relational domains (Herman, Reference Herman1992). DSM-5 introduced a dissociative subtype, and ICD-11 has proposed including complex PTSD as a separate subtype. Epidemiological evidence on both issues is presented in Chapter 20 and in Chapter 21 of this volume.
Overall, the contributions to understanding the nature of PTSD included in Section 5 of this volume fulfill one of the basic functions of epidemiology, which is to complete the clinical picture (Morris, Reference Morris1957). For PTSD and other psychiatric disorders, this is best accomplished with data from community samples composed of a mix of untreated and treated cases.
Strengths and Limitations of the WMH Surveys
PTSD clearly places a great burden on the population because of the ubiquity of trauma, the relatively high rate of PTSD, the high rate of chronicity after onset, and in many parts of the world, the scarcity of treatment interventions that might lead to prevention or early remission. The WMH studies discussed in this volume take a comprehensive approach to the global epidemiology and phenomenology of PTSD. The WMH initiative constitutes the largest cross-national series of population-based surveys of mental disorders ever conducted (Kessler & Üstün, Reference Kessler and Üstün2008). The core strength of the WMH surveys is the standardization of every aspect of the study, from the comprehensive assessment of mental and substance use disorders to the broad selection of risk factors and consequences. Methodologically, these surveys employed uniform procedures for (1) translation and back-translation of the CIDI; (2) representative sampling strategies; (3) training and oversight of local trainers and supervisors; and (4) oversight of country-specific data collection, management, and analysis.
The heart of the study is the CIDI diagnostic interview schedule, which is described in detail in Chapter 2. The instrument has broad diagnostic coverage and special methods for determining age-of-onset, disability, service utilization, medical conditions, demographic histories, family history, and childhood adversities. Interviewers are given special training about best practices for keeping respondents focused and motivated throughout the assessment. Most importantly, the WMH surveys instituted unique methods to facilitate recall in order to create a database containing temporally ordered variables capable of disentangling antecedents from sequelae.
A critical feature of the CIDI is the assessment of PTSD for a randomly selected trauma in order to provide unbiased estimates of the prevalence of PTSD in general and the conditional risk of PTSD after specific traumas. Prior community surveys assessed PTSD for respondent-reported most stressful or worst trauma. For clinical samples, this approach is judicious. For epidemiological purposes, however, this approach overestimates the overall and conditional rates of PTSD because the traumas selected (DSM-IV Criterion A1) are not representative of the multiple traumas occurring over the course of the lifetime. In addition, the worst traumas are not representative of all traumas of a given type. Thus, the use of the random trauma method ensures that the conditional risks of PTSD reflect the full range of human experiences, not just the worst possible situations. This decision was based in part on a comparison of PTSD prevalence after random versus worst trauma in a general population sample, which, not surprisingly, found higher rates of PTSD after respondent-reported worst trauma (Breslau et al., Reference Breslau, Peterson, Poisson, Schultz and Lucia2004). Specifically, the overall rate of PTSD after worst traumas was 13.6%, while the rate after randomly selected traumas was 9.2%. This considerable disparity was found for PTSD in conjunction with each trauma assessed by the study. The biggest disparity occurred for one of the most commonly reported traumas – life-threatening illness. When selected as the worst trauma, the rate of PTSD was 31.2%. When selected as a random trauma, it was 1.1%. Similarly, when rape was chosen by respondents as their worst trauma, the rate of PTSD was 62.0%. When rape was chosen randomly, the rate was 49.0%. Such discrepancies suggest that for purposes of determining the prevalence and risk factors for PTSD in general population samples drawn from culturally and socioeconomically diverse settings, basing estimates of PTSD on a randomly selected trauma would provide a more unbiased portrait of the epidemiology of PTSD.
Another pivotal decision in designing the version of the CIDI used in the WMH surveys was to assess all of the DSM-IV PTSD criteria, without skipping out if the respondent failed to endorse the A2 criterion or the requisite number of re-experiencing, avoidance/numbing, or hyper-arousal symptoms. This was especially important for achieving the nosological aims described above. Due to the choice of a random trauma as the focal trauma for assessing PTSD as well as the rest of the WMH methodology, this volume brings together a fresh perspective on the epidemiology and phenomenology of PTSD.
Of course, cross-national studies such as the WMH surveys have built-in limitations, as is true of all cross-sectional surveys. Each chapter of this volume reflects on the limitations of the specific analyses of trauma and PTSD under consideration. Overall, we note that the WMH surveys made an effort to balance the standardization needed to compare and combine data from countries across the globe with inclusion of culturally relevant clinical, demographic, and psychosocial risk factors needed for clinically meaningful country-specific analyses of PTSD. The final chapter of this volume discusses the research and policy implications of the WMH findings.
As alluded to earlier in this chapter, PTSD and psychiatric epidemiology as a whole are both relatively new fields of research. It is thus noteworthy that since its inception, the WMH initiative has been a training ground for investigators from around the world with an interest in psychiatric epidemiology. In addition to annual WMH meetings where achievements, problems, and new ideas for research are discussed, WMH investigators receive feedback about framing research questions, carrying out analyses, writing, and making in-person presentations of research results from senior WMH colleagues and outside experts. WMH collaborators also have access to the basic tools, building blocks, and supports needed to build successful and productive careers in psychiatric epidemiology. Several researchers who initially joined the WMH initiative as junior investigators have since become internationally recognized leaders in mental health research in general and PTSD research specifically. This accomplishment is a tribute to the vision and consistent oversight by the WMH founders and their staff to whom the field of global mental health research owes an enormous debt.
Conclusion
This volume is the culmination of in-depth interviews with close to 70,000 adult participants from 24 countries on 6 continents who answered questions about exposure to 29 separate trauma types and the PTSD symptoms that occurred in their wake. This book represents the collective work of investigators from each country and their outstanding research teams. Section 1 provides an overview of key studies of the epidemiology of PTSD and details about the methodology implemented by the WMH surveys. Section 2 assesses the nature and extent of trauma exposure around the globe, socio-demographic risk factors, and two potent influences on the risk of exposure, childhood adversities and pre-existing psychopathology. Section 3, which is devoted to the descriptive epidemiology of PTSD, contains chapters on the prevalence and risk factors for PTSD, secondary psychiatric and medical morbidities, impairments, and use of mental health services as well as barriers to care. Section 4, the longest section of the book, explores a few critical drivers of the development and course of PTSD, such as childhood adversities and prior psychopathology, and examines four specific traumas in detail: sexual assault in women, motor vehicle collisions, unexpected death of a loved one, and disasters. Section 5 provides evidence from the WMH on key nosological issues, including the overlap in case identification across sets of diagnostic criteria, empirical findings supporting the DSM-5 decision to remove the DSM-IV A2 criterion, and WMH evidence on the prevalence and correlates of subthreshold, dissociative, and complex PTSD. Section 6 features a chapter describing a novel statistical strategy for identifying groups at high risk for developing PTSD, and a concluding chapter on the broad implications of the WMH results for both our current understanding of PTSD and for future research into this commonly occurring, seriously impairing, and severely undertreated disorder. Our deepest hope is that this volume will serve as a valuable resource for clinicians, researchers, and policy makers around the world for many years to come.