Non-cancer screening
Screening for health conditions is predicated on the principle that early detection of health anomalies provides access to earlier treatment, as well as increasing healthy behaviours and reducing risky ones, leading to positive health outcomes. 1,Reference Bell, Grad, Dickinson, Singh, Moore and Kasperavicius2 However, this is not always the case. Screening occurs in individuals who are asymptomatic (without symptoms); however, when the screening outcome is above but close to the diagnostic threshold, subsequent diagnostic labelling (e.g. mild hypertension, mild hyperlipidaemia) potentially identifies otherwise healthy individuals as unwell. Reference Bell, Grad, Dickinson, Singh, Moore and Kasperavicius2,Reference Dickinson, Pimlott, Grad, Singh, Szafran and Wilson3 Although some researchers have proposed that screening may reduce clinical and economic burden, others have highlighted an increased burden owing to more individuals being labelled and the potential for those labelled to experience negative psychological, psychosocial and physical consequences following screening and subsequent diagnostic labelling. 1–Reference Brodersen, Schwartz, Heneghan, O’Sullivan, Aronson and Woloshin6 Evidence for the impacts of cancer screening (e.g. breast cancer, prostate cancer) and subsequent diagnostic labelling and treatment has received significant research attention. Reference Chad-Friedman, Coleman, Traeger, Pirl, Goldman and Atlas4,Reference Kim, Chung, Keir and Patrick5 However, routine non-cancer screening – that is, screening for physical (e.g. hypertension, hyperlipidaemia) and psychological (e.g. depression, anxiety) non-cancer health conditions – has received less research focus.
Diagnostic labelling
The use of diagnostic labels has been found to be increasing. Reference Brodersen, Schwartz, Heneghan, O’Sullivan, Aronson and Woloshin6,Reference Moynihan, Brodersen, Heath, Johansson, Kuehlein and Minue-Lorenzo7 This trend is likely to be influenced by screening and changes in diagnostic criteria, including the expansion of disease definitions to encompass mild or lower thresholds for health conditions. Reference Brodersen, Schwartz, Heneghan, O’Sullivan, Aronson and Woloshin6,Reference Kale and Korenstein8,Reference Sexton, Heal, Banks and Braniff9 The impacts of diagnostic labelling on individuals and healthcare services range from positive (e.g. relief, self-understanding) to negative (e.g. psychological distress, anxiety, negative side-effects of treatment) and include financial impacts due to diagnostic cascades and overtreatment. Reference Kale and Korenstein8,Reference Sims, Michaleff, Glasziou and Thomas10 A recent systematic review found that anxiety increased in the short term following health condition screening; however, longer-term consequences were unclear. Reference Sims, Michaleff, Glasziou, Jones and Thomas11 Further, social constructionism emphasises the role of society and social interactions in developing and maintaining routine screening and diagnostic labelling, as well as stereotypes and perceptions of capabilities of individuals with a diagnostic label. Reference Bell, Grad, Dickinson, Singh, Moore and Kasperavicius2,Reference Andrews12–Reference Conrad and Barker14 Despite the potential impacts of screening and subsequent condition-labelling, even in their mildest form, it is not known whether or how general practitioners (GPs) discuss these complex issues with patients or whether patients are aware or adequately informed of the potential consequences of screening.
Objectives
From the perspective of GPs and healthcare consumers (consumers), we aimed to identify whether GPs and consumers discussed the potential consequences of diagnostic labelling before screening and the applicability of the current literature in the clinical encounter. The research questions for this study were as follows.
-
(a) Do GPs discuss the potential consequences of diagnostic labelling before routine screening for non-cancer health conditions? If so, why and how, and if not, why not?
-
(b) What is the applicability of the current literature to the consequences of diagnostic labelling before non-cancer screening?
Methods
The study protocol is available on Open Science Framework (https://osf.io/3fxvn/). The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. All procedures involving human subjects and/or patients were approved by Bond University Human Research Ethics Committee (RS00318 and RS00322).
Participants and recruitment
The sample size required for qualitative studies using thematic analysis has been suggested to be 6–10 interviews and 2–4 focus groups. Reference Ritchie, Lewis, McNaughton-Nicholls and Ormston15 However, the stopping criteria are based on data saturation or the non-emergence of new themes, rather than achieving a specific number of interviews or focus groups. Reference Ritchie, Lewis, McNaughton-Nicholls and Ormston15
General practitioners
Eligible GPs were those currently practising as GPs in Australia. Recruitment strategies included advertising through mailing lists, websites and social media accounts of professional organisations (e.g. GoldNet Research) and snowballing. Interested participants completed an online survey, which included written consent and eligibility and demographic questions. Eligible participants were contacted by R.S. to schedule the semi-structured interview. GPs received a AU$100 gift voucher as reimbursement for their time.
Healthcare consumers
Consumers were purposely sampled to align with the Royal Australian College of General Practitioners recommendations for preventive age-related health checks for individuals aged 45–65 years. 16 We recruited consumers aged 40–65 years who were currently or soon would be eligible for these checks. 16 As we were interested in discussing the consequences of diagnostic labelling following screening, we included consumers who had not been diagnosed with cancer or health conditions requiring intensive treatment. We excluded consumers receiving treatment for a long-standing or life-threatening health condition (e.g. chronic kidney disease, cardiovascular disease), undergoing testing for a suspected health condition, unable to provide informed consent, unable to speak or understand English, or unable to access a computer and reliable internet connection.
Recruitment strategies included advertising through mailing lists, websites and social media accounts of consumer organisations (e.g. JoinUs) and snowballing. Interested participants completed an online survey, which included eligibility checking, written consent and demographic questions. Eligible participants were contacted by R.S. to be allocated to a focus group. Consumers received a AU$50 gift voucher as reimbursement for their time.
Procedure and materials
Data were collected through semi-structured interviews with GPs and focus groups with consumers. Different data collection methods were used owing to challenges in coordinating multiple GPs to attend a scheduled focus group. Reference Ritchie, Lewis, McNaughton-Nicholls and Ormston15 Semi-structured interviews and focus group structures, interview guides and presentation materials were developed in consultation with the wider research team; additional information is provided in Supplementary Table 1 available at https://doi.org/10.1192/bjo.2025.5.
Semi-structured interviews with GPs
R.S. conducted semi-structured interviews of up to 1 h duration between May and July 2023 via video-enabled online platforms (i.e. Zoom and Microsoft Teams). GPs were asked open-ended questions regarding their clinical practice, presented with a short pre-recorded presentation on available research evidence about the consequences of diagnostic labelling (recorded by R.S. and available at https://osf.io/yp5wz), offered the opportunity to comment on the presentation and asked to discuss the clinical applicability of the information presented.
Focus groups with consumers
Focus groups, each 90 min in duration, were conducted in August 2023 via Zoom and were facilitated by R.S. and R.T. Consumers were presented with two short, pre-recorded presentations. The first provided overviews of routine screening and interpretation of risks for health conditions (recorded by P.G. and available at https://osf.io/75mpa). The second was the same as that presented to GPs. After each presentation, consumers were offered the opportunity to discuss the information presented and ask questions. Consumers were then asked open-ended questions to facilitate discussion regarding the applicability of the information to screening.
The research team
Adhering to the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist, the study team have expertise across psychology, clinical medicine, clinical epidemiology and public health. R.S. is a clinical psychologist and PhD candidate, with an interest in the impacts of diagnostic labelling. Z.A.M. is a physiotherapist with a PhD and an interest in evidence-based assessment, diagnosis and treatment of health conditions. P.G. is an academic general practitioner and clinical epidemiologist with a PhD and leads international research on overdiagnosis and overtreatment. R.T. is a psychologist with a PhD and an interest in consumer and community involvement in healthcare and policy development. R.S., Z.A.M. and R.T. are female, and P.G. is male. The completed COREQ checklist is provided in Supplementary Table 2.
Analyses
Demographic data were collated, summarised and presented using descriptive statistics. Data from semi-structured interviews with GPs and focus groups with consumers were audio recorded and transcribed verbatim using automated transcription. Transcripts were checked for accuracy by R.S. We used thematic analysis methods based on framework analysis, as described by Ritchie and colleagues. Reference Ritchie, Lewis, McNaughton-Nicholls and Ormston15 Social constructionism underpins the theoretical framework, whereby the meanings produced through research are influenced by the social world of both the participants and researchers. Reference Andrews12,Reference Moncrieffe, Moncrieffe and Eyben13,Reference Ritchie, Lewis, McNaughton-Nicholls and Ormston15 Subsequently, we aimed to understand the diversity of participants’ experiences, rather than identifying one uniform meaning.
Transcripts were analysed using NVIVO version 12 (Lumivero; see https://lumivero.com/products/nvivo/). An inductive and iterative thematic approach was used to facilitate understanding of responses and participant perspectives. First, data familiarisation involved transcript review and development of an initial coding framework (R.S.), analysing responses to each question and collective responses across transcripts. Through discussion and feedback from the wider research team, the initial framework was refocused on how the data addressed the specific research questions, and the number of themes was reduced to reflect the data more accurately. R.S. then re-coded two transcripts to the revised framework. This coding was discussed among the wider research team, with the overall themes and subthemes remaining unchanged following discussion. The framework was then applied to the whole data-set (R.S.), and data saturation was achieved. Last, the final coding was reviewed by R.T. and/or Z.A.M. to ensure reliability.
Transparency declaration
The authors confirm that this manuscript is an honest, accurate and transparent account of the study reported; that no important aspects of the study have been omitted; and that any discrepancies from the study protocol have been explained.
Patient and public involvement
No patients or members of the public were involved in the conceptualisation of this study. GPs and consumers took part in the conduct of this study as participants but were not involved in the study design or the analysis or write-up of results.
Results
Demographics
General practitioners
Thirteen GPs expressed interest in participating, and 11 participated. The 11 GPs had an average of 13 years practising as a GP (range 4–27 years), and six of them were female (55%). Most GPs (n = 10, 91%) practised in metropolitan locations, and roughly half (n = 6, 55%) worked in GP-only practices and across multiple patient demographics. One eligible GP failed respond to initial researcher contact following expression of interest, and another failed to attend their scheduled semi-structured interview and did not respond to subsequent contact. Table 1 provides additional information regarding GPs.
Table 1 General practitioner (GP) demographics
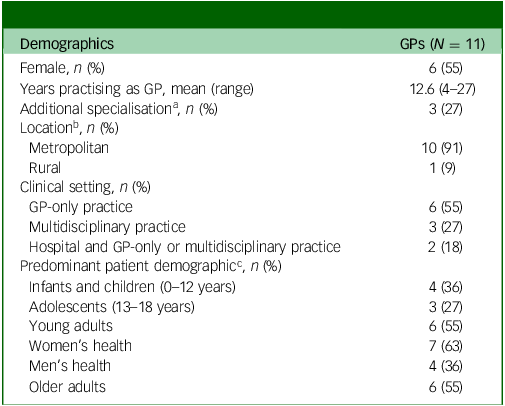
a. Areas of additional specialisation were psychiatry and research, Diploma of Child Health, rural generalism, and Fellow of the Royal Australian College of General Practitioners.
b. Location based on the modified Monash model. 17
c. GP could practise across more than one patient demographic.
Healthcare consumers
Eleven consumers expressed interest in participating, and eight participated. Six of the eight (75%) consumers were female and married or in a de facto relationship, and the average age was 55 years (range 46–63 years). Four (50%) lived in a regional location and were highly educated (university postgraduate degree). Four (50%) reported having undergone screening for a health condition, and most (n = 7, 87.5%) reported having a diagnosed health condition (e.g. asthma, coeliac disease, hypertension) detected more than 2 years ago. In addition, one consumer did not respond to initial researcher contact after an expression of interest, and two failed to attend their scheduled focus group and did not respond to subsequent contact. Table 2 provides additional information regarding consumers.
Table 2 Healthcare consumer demographics
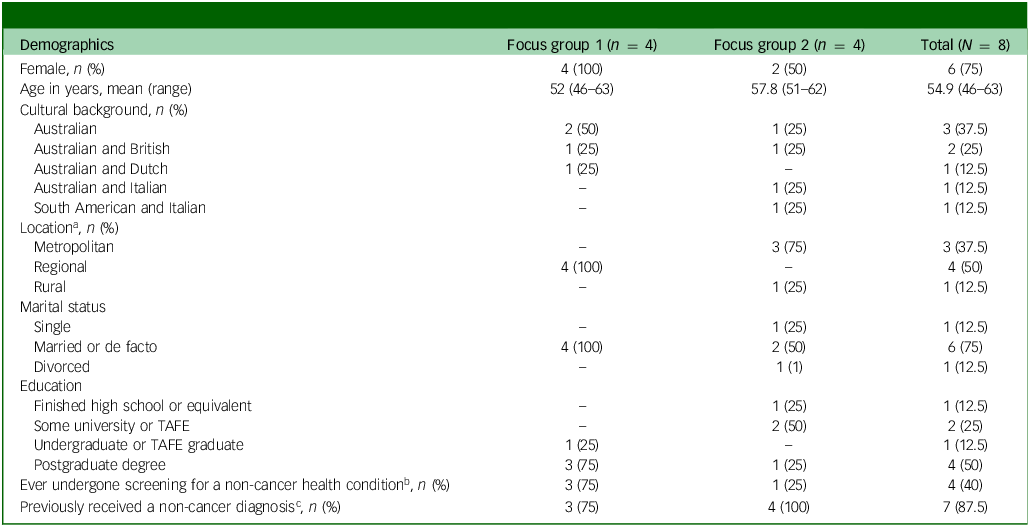
TAFE, Technical and Further Education.
a. Location based on the modified Monash model. 17
b. Reported non-cancer screening included blood pressure and diabetes.
c. Reported non-cancer diagnoses included asthma, coeliac disease, rheumatoid juvenile arthritis, gestational diabetes mellitus, hypertension, vasculitis, thalassemia trait, gastroesophageal reflux disease and narrow-angle glaucoma (with all reported diagnoses made more than 2 years ago).
Qualitative synthesis
When asked whether GPs discussed the potential impacts of diagnostic labelling before screening (research question 1), there was little support for discussing specific impacts of diagnostic labelling before a condition was identified. However, we identified themes regarding general information GPs included in conversations before screening. Whether the literature on the consequences of diagnostic labelling was applicable to their GP–patient encounters (research question 2), qualitative themes related to the value of discussions being routine or only when a health condition was identified. Overall, the two research questions were addressed through six themes: patient empowerment, patient variability, condition-specific information, GP and patient interactions and relationship (four subthemes), GP role and responsibilities (four subthemes), and characteristics of the screening test (two subthemes).
Table 3 defines themes and subthemes, and Fig. 1 provides a representation of the relationship between themes and research questions. Quotes from participants are attributed to group and characteristics. GPs are acknowledged by their participant number, sex (F, female; M, male), years of clinical experience and location (e.g. GP1, M, 4 years, metropolitan). Consumers are designated by their participant number, sex (F, female; M, male), previously diagnosed health condition (yes, no) and location (e.g., C1, F, yes, regional).
Table 3 Theme and subtheme descriptions
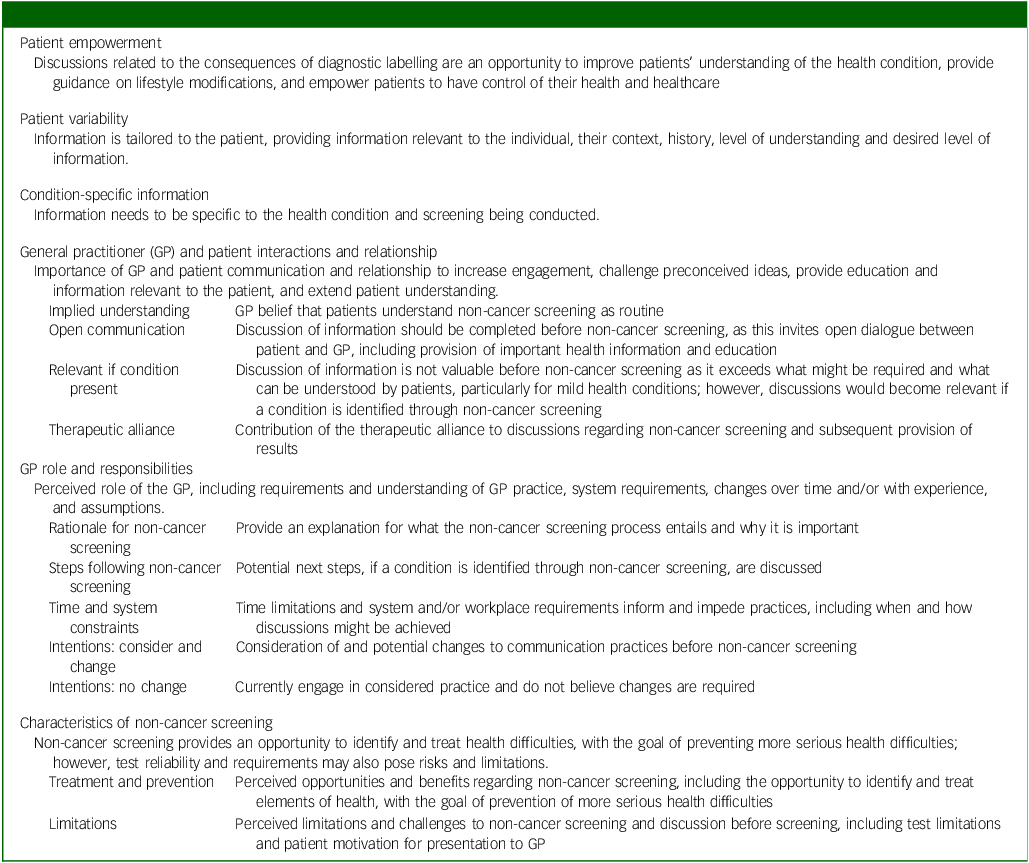
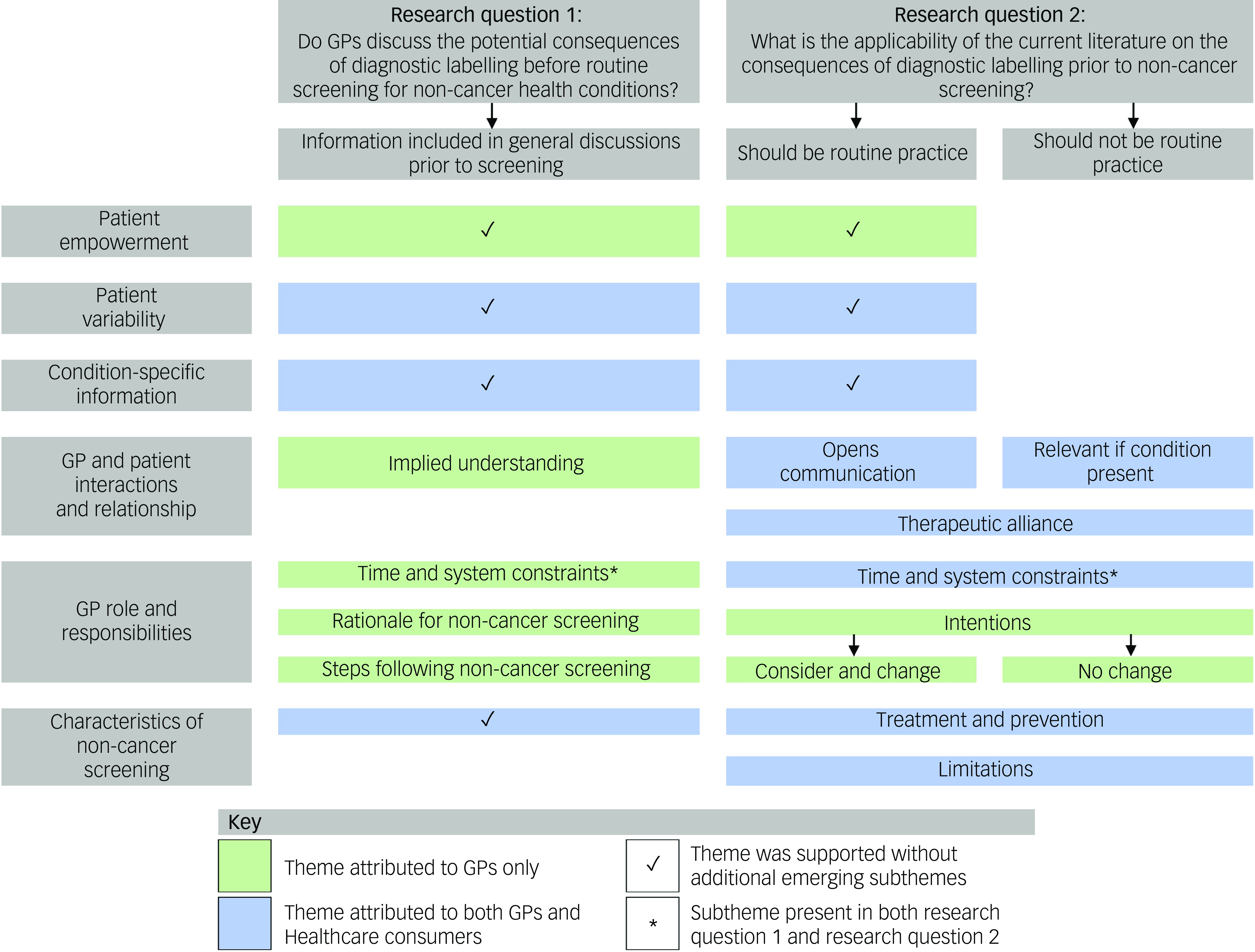
Fig. 1 Relationships among themes, subthemes and research questions supported by general practitioners and/or consumers. GP, general practitioner.
Research question 1: Do GPs discuss the potential consequences of diagnostic labelling prior to routine screening for non-cancer health conditions? If so, why and how, and if not, why not?
Most GPs said they did not discuss potential impacts of diagnostic labelling before routine screening. However, many reported that they had brief conversations, centred on the screening procedure and possible limitations, with patients before screening. Other than screening during pregnancy, consumers struggled to identify health conditions for which they might be screened and could not recall GPs discussing potential impacts of diagnostic labelling before screening. All six themes were identified in relation to this research question (Fig. 1), with subthemes within the GP role and responsibilities (time and system constraints, rationale for non-cancer screening, steps following non-cancer screening) and GP and patient interactions and relationship (implied understanding) themes. Three themes were reported by GPs only (patient empowerment, GP and patient interactions and relationship, and GP role and responsibilities), and three were reported by both GPs and consumers (patient variability, condition-specific information, and characteristics of non-cancer screening). Themes are discussed below and detailed in Table 4.
Table 4 Do general practitioners (GPs) discuss the potential consequences of diagnostic labelling before routine screening for non-cancer health conditions? If so, why and how, and if not, why not?
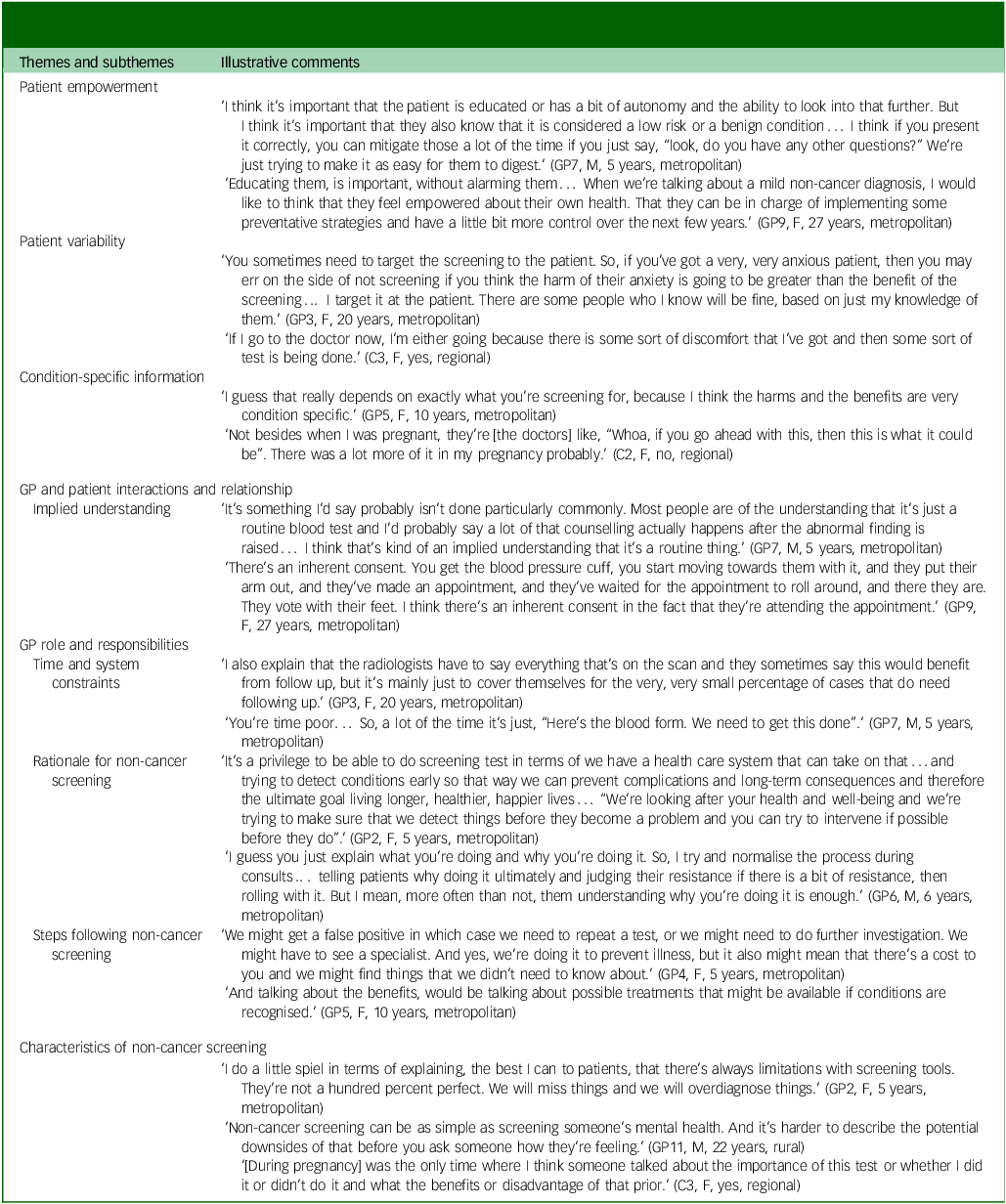
Patient empowerment
GPs discussed the importance of empowering patients though provision of information to aid patients’ ability to make an informed decision before undergoing screening. GPs acknowledged the importance of providing information and an opportunity for the patient to ask questions and consider lifestyle changes.
Patient variability
Both GPs and consumers discussed the need to target screening discussions and information provision to the requirements and preferences of the individual patient. GPs reported that they tailored the information provided to patients based on a range of factors including their clinical acumen.
Condition-specific information
Similarly, GPs and consumers discussed the information provided being specific to the condition being screened.
GP and patient interactions and relationship
GPs discussed the importance of GP and patient relationships in facilitating patient engagement and understanding. However, some GPs stated that patients understood screening as routine (implied understanding); therefore, they did not ordinarily have discussions about labelling before screening.
GP role and responsibilities
Only GPs raised this theme in relation to discussing the potential impacts of diagnostic labelling. Three subthemes were identified. The time and system constraints subtheme highlighted that clinical encounters are often guided by time limitations and workplace regulations. The rationale for non-cancer screening subtheme centred around general discussions about screening tests rather than the impact of diagnostic labelling, whereas the steps following screening subtheme centred on managing patient impact after test results were provided.
Characteristics of non-cancer screening
GPs highlighted limitations and challenges associated with screening tests. Many comments about screening involved minimally invasive tests which provided an opportunity to identify, treat and prevent more serious health difficulties. However, challenges associated with test reliability were also raised. Consumers did not recall any discussions about the potential impact of having a diagnostic label except during pregnancy.
Research Question 2: What is the applicability of the current literature on the consequences of diagnostic labelling before non-cancer screening?
Following the presentation of information, most GPs and consumers said that conversations regarding the consequences of diagnostic labelling ‘should be routine practice,’ with this view represented across all six themes. However, others perceived these discussions as relevant only if a condition was identified through screening (‘should not be routine practice’). This latter viewpoint was supported in three themes (GP and patient interactions and relationship, GP role and responsibilities, and characteristics of non-cancer screening). For all themes except patient empowerment, both GP and consumer viewpoints were reported (Fig. 1). Within the GP roles and responsibilities theme the subtheme of time and system constraints was again identified, with GPs also mentioning their intentions regarding changes to clinical practice (GP intentions). Subthemes also emerged for GP and patient interactions and relationship (opens communication, relevant if condition present, therapeutic alliance) and characteristics of non-cancer screening (treatment and prevention, limitations). Themes are discussed below and detailed in Table 5.
Table 5 What is the applicability of the current literature on the consequences of diagnostic labelling prior to non-cancer screening?
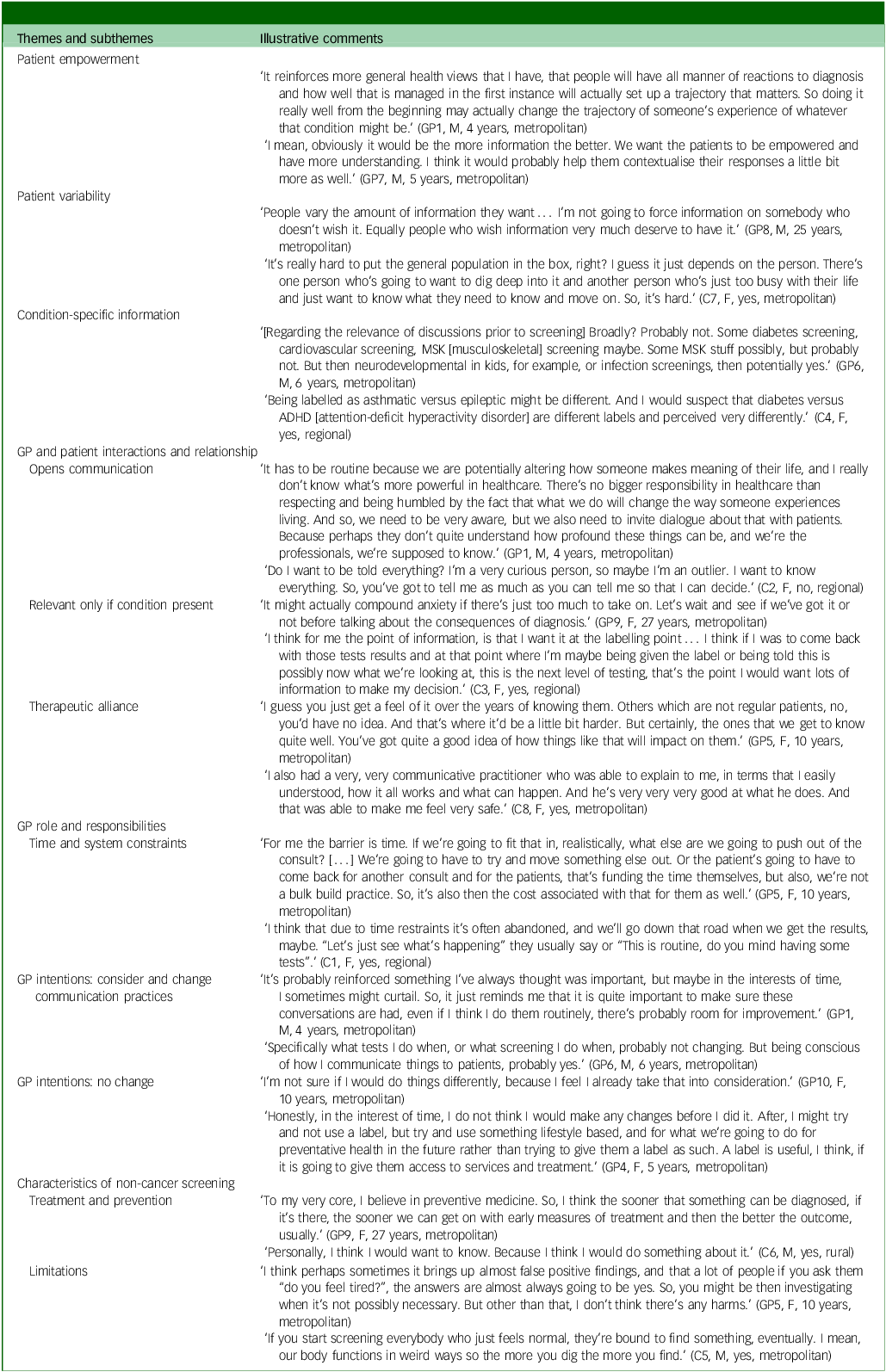
Patient empowerment
Some GPs noted that discussions before screening would be valuable to facilitate patient understanding of and receptiveness to information in the future, even if the information discussed was not immediately relevant.
Patient variability
Regarding the potential of a diagnostic label to be useful in discussions before screening, both GPs and consumers considered differences in individual patient preferences for information and the need to adapt to these preferences.
Condition-specific information
GPs and consumers noted that discussions before screening needed to contain information specific to the condition being screened, with differences between physical and psychological health conditions also identified.
GP and patient interactions and relationships
Some GPs and consumers perceived discussions regarding the consequences of diagnostic labelling before screening as valuable and considered that they should be routine practice. Reasons for this included the potential to invite dialogue between the GP and patient and provide an opportunity to convey important health information and education (opens communication). Other GPs and consumers perceived discussions regarding the consequences of diagnostic labelling as not valuable and considered that they should not be routine practice before screening, as such concepts might be difficult to understand and exceed requirements. However, these GPs and consumers added that discussions would be necessary after screening if conditions were identified.
Regardless of whether discussions were preferred as routine practice or only if conditions were identified, the contribution of the therapeutic alliance to the clinical encounter was emphasised by GPs and consumers, with a stronger therapeutic alliance suggested to increase GP ease of, and patient response to, communication.
GP role and responsibilities
Time and system constraints were again identified as challenging with respect to how and when routine discussions about the consequences of diagnostic labelling might occur, with these difficulties raised irrespective of whether GPs and consumers considered that discussions should be routine or not.
Regarding intentions, from the information provided and discussed in the semi-structured interviews, many GPs noted that they would consider and change conversations prior to screening. Specifically, GPs stated that they would be more conscious of potential impacts of screening, including diagnostic labelling, and allow increased time to have discussions with patients before screening. Other GPs noted that no change would be made to screening practices or discussions before this, mostly because they perceived their current practices to include sufficient discussions or because of time constraints.
Characteristics of non-cancer screening
Two subthemes emerged in relation to the value of discussing potential impacts of diagnostic labelling, with these identified as important in both routine and non-routine conversations. Both GPs and consumers discussed screening as an opportunity to identify and treat elements of health and prevent more serious health complications (treatment and prevention). Further, possible limitations to screening were identified, including test limitations, over-investigation, financial requirements and the potential to overwhelm patients (limitations).
Discussion
We conducted 11 semi-structured interviews with GPs and two focus groups with eight consumers to examine whether the potential consequences of diagnostic labelling were discussed before routine screening and to identify the perceived value of such evidence-informed discussions. Many GPs reported that they provided patients with brief information regarding screening procedures and limitations before routine screening; however, no GPs reported discussing potential consequences of diagnostic labelling. Similarly, consumers could not recall GPs discussing potential consequences of diagnostic labelling before screening, except during pregnancy. The perceived value of discussing consequences of diagnostic labelling before screening varied. Some GPs and consumers considered that these types of discussion would facilitate understanding, whereas others thought they would only be valuable after a condition had been identified. Some GPs noted that they would consider making changes to their clinical practice to incorporate these labelling discussions before screening, whereas others stated that no changes were required. Six overarching themes related to the value of discussing the consequences of diagnostic labelling were identified: patient empowerment, patient variability, condition-specific information, GP and patient interactions and relationship, GP role and responsibilities, and characteristics of non-cancer screening.
Strengths and limitations
This study provided insights from the two perspectives present in the clinical encounter: GP and consumer. This allowed comparison of perceptions between two populations who either impact (GPs) or are impacted by (consumers) screening and highlighted differences and similarities in perceptions of the information discussed. Conducting both semi-structured interviews and focus groups was also a strength, as it was intended to facilitate greater engagement from both populations. Multiple recruitment techniques were used to broaden the potential participant pool and increase the diversity of perspectives. Provision of pre-recorded presentations ensured consistency of information presented, and the use of standardised interview guides enabled targeted, but flexible, discussions.
Several limitations potentially affected our results. Difficulty recruiting both GPs and consumers resulted in participant numbers substantially lower than those anticipated for both semi-structured interviews and focus groups. Although thematic saturation was achieved across modalities and populations, additional findings may have emerged if further focus groups with greater participant numbers had been completed. Homogeneity of recruited participants, including geographical similarities, may have affected the diversity of themes; it is thus important to consider the applicability of the developed themes to rural, remote or underprivileged populations and to consumers with low literacy. The online format of both semi-structured interviews and focus groups, while potentially increasing accessibility, may have deterred some individuals from participating and affected the level of engagement of those who participated.
Results in relation to existing studies
Our results highlight variability in patient preferences regarding discussions of diagnostic labelling and a need for GPs to be aware of or quickly ascertain a patient’s informational needs and preferences. Similar patient variability has been found in research examining medical maximising and minimising in healthcare preferences, whereby medical maximisers prefer active healthcare (e.g. optional medical tests and treatments), whereas medical minimisers prefer passive healthcare (e.g. medical tests and treatments only when necessary). Reference Scherer, Caverly, Burke, De Witt and Zikmund-Fisher18 In addition to patient factors, our findings emphasise the importance of GP–patient interactions and relationship (including therapeutic alliance) in facilitating when and how discussions are completed, as well as patients’ feeling understood and respected in the communication. Similarly, previous research supports therapeutic alliance and GP–patient relationships as important to patient satisfaction, treatment adherence and clinical outcomes. Reference Chipidza, Wallwork and Stern19–Reference Krogsbøll, Jørgensen and Gøtzsche23
In the current sample, discussions regarding the potential consequences of a diagnostic label before screening were not ordinarily completed, and both GPs and consumers appreciated patient preferences and health conditions as important considerations. However, our findings parallel results of research examining the communication of test results in primary care, with one study finding that patient characteristics (e.g. anxiety, health literacy) and health condition characteristics (e.g. severity) influenced how and when results were communicated. Reference Litchfield, Bentham, Lilford and Greenfield24 Previous research has suggested a tendency for both GPs and patients to overestimate the benefits and underestimate the harms of screening. Reference Hoffmann and Del Mar25,Reference Hoffmann and Del Mar26 The potential to underestimate the harms of screening was further highlighted by the findings of this study, which suggest that some GPs may overlook potential harms of screening in favour of potential benefits. One such overlooked harm may be the possibility that unnecessary testing, resulting from screening, might itself be harmful. We also found that the language used by GPs, particularly when discussing the minimal invasiveness of screening tests, echoes the underestimation of potential consequences of being given a diagnostic label.
A systematic review of both qualitative and quantitative studies examined the barriers and facilitators to prevention (e.g. through screening and/or addressing lifestyle change) of cardiometabolic diseases (e.g. diabetes mellitus, chronic kidney disease) in primary care. Reference Wändell, de Waard, Holzmann, Gornitzki, Lionis and deWit27 The review found GP time restrictions and workload to be among the most frequently reported barriers, whereas strong GP–patient relationships and appreciation of the importance of prevention were frequently reported facilitators of screening and prevention. Reference Wändell, de Waard, Holzmann, Gornitzki, Lionis and deWit27 Although it did not focus on the consequences of diagnostic labelling, the review echoed our findings, highlighting time and workload as barriers to addressing asymptomatic health conditions in primary care. Additional discussions regarding the consequences of diagnostic labelling may inflate this barrier, with further consideration of how and when to best implement discussions regarding the consequences of diagnostic labelling required to minimise potential barriers.
Implications
These results have implications for clinical encounters and health systems, and future research exploring these. Consumers had difficulty identifying non-cancer health conditions that could be identified through screening and did not recall GPs having conversations before screening regarding possible impacts of diagnostic labelling or screening procedures. By contrast, many GPs noted having discussions regarding screening procedures and test limitations before screening. This may simply reflect a lack of recall, or it might result from differences between GP and patient perceptions of needs and preferences regarding discussions related to screening. This finding, when combined with the literature on overestimating benefits and underestimating harms, indicates that this may be a problem. Reference Hoffmann and Del Mar25,Reference Hoffmann and Del Mar26 To address it, we may need to observe clinical encounters to determine whether and how these conversations occur.
A frequently occurring barrier to discussions, reported by both GPs and consumers, was time limitations. Careful balancing of time limitations with developed guidelines is important to ensure evidence-based healthcare. To facilitate this, changes to health systems, particularly in primary care, may be required to provide GPs sufficient time to engage in discussions with patients regarding the consequences of diagnostic labelling. In addition, consideration of the involvement of all health professionals who conduct screening tests in initiating conversations regarding diagnostic labelling may facilitate discussions while supporting time limitations. Although service provision time and cost require balancing, health system change may transform socially constructed views and understandings of health and healthcare. Reference Conrad and Barker14 This transformation may facilitate how health conditions, diagnostic labels and intervention are viewed.
Future research
We focused on non-cancer screening for individuals aged 40–65 years to align with guidelines for preventive health checks in Australia. 16 However, research examining similarities and differences between older and younger age groups regarding screening is important, as health condition risk, treatment and prognosis may differ. GPs in our study expressed that patients had an implied understanding of non-cancer screening. Whether implied understanding is sufficient, or whether there is need for greater informed consent within non-cancer screening, remains unclear. It may be that discussion about the potential harms and benefits of a diagnostic label enhances patient informed consent. However additional research is required. It is possible that developing decision aids for screening tests, as well as patient-reported outcome measures and patient-reported experience measures, aimed at non-cancer screening and diagnostic labelling will improve this, but research is needed. Reference Kingsley and Patel28,Reference Agoritsas, Heen, Brandt, Alonso-Coello, Kristiansen and Akl29 Such further research would support the development of clinical guidelines to facilitate GP–patient interactions and minimise potential harms, while maximising potential benefits, when diagnostic labelling is required.
Supplementary material
The supplementary material is available online at https://doi.org/10.1192/bjo.2025.5
Data availability
Data generated and/or analysed during the current study are available from the corresponding author upon reasonable request.
Acknowledgements
We thank all the GPs and healthcare consumers for their assistance in completing this research. We also thank GoldNet Research and JoinUs for their assistance in recruitment.
Author contributions
R.S., Z.A.M., R.T. and P.G. contributed to the conception and design of the study. R.S. conducted all interviews, and R.S. and R.T. facilitated focus groups. R.S., Z.A.M. and R.T. contributed to data analysis and interpretation. R.S., Z.A.M., R.T. and P.G. contributed to the drafting of the manuscript, and all authors approved the final version.
Funding
R.S. is supported by an Australian Government Research Training Program Scholarship. R.T. is supported by the Tropical Australian Academic Health Centre. Z.A.M. is supported by the Northern New South Wales Local Health District. P.G. is supported by a NHMRC Investigator grant (no. 1175487). The funding sources had no role in study design, data collection, data analysis, data interpretation or the writing of the report.
Declaration of interest
None.









eLetters
No eLetters have been published for this article.