No CrossRef data available.
Published online by Cambridge University Press: 24 March 2025
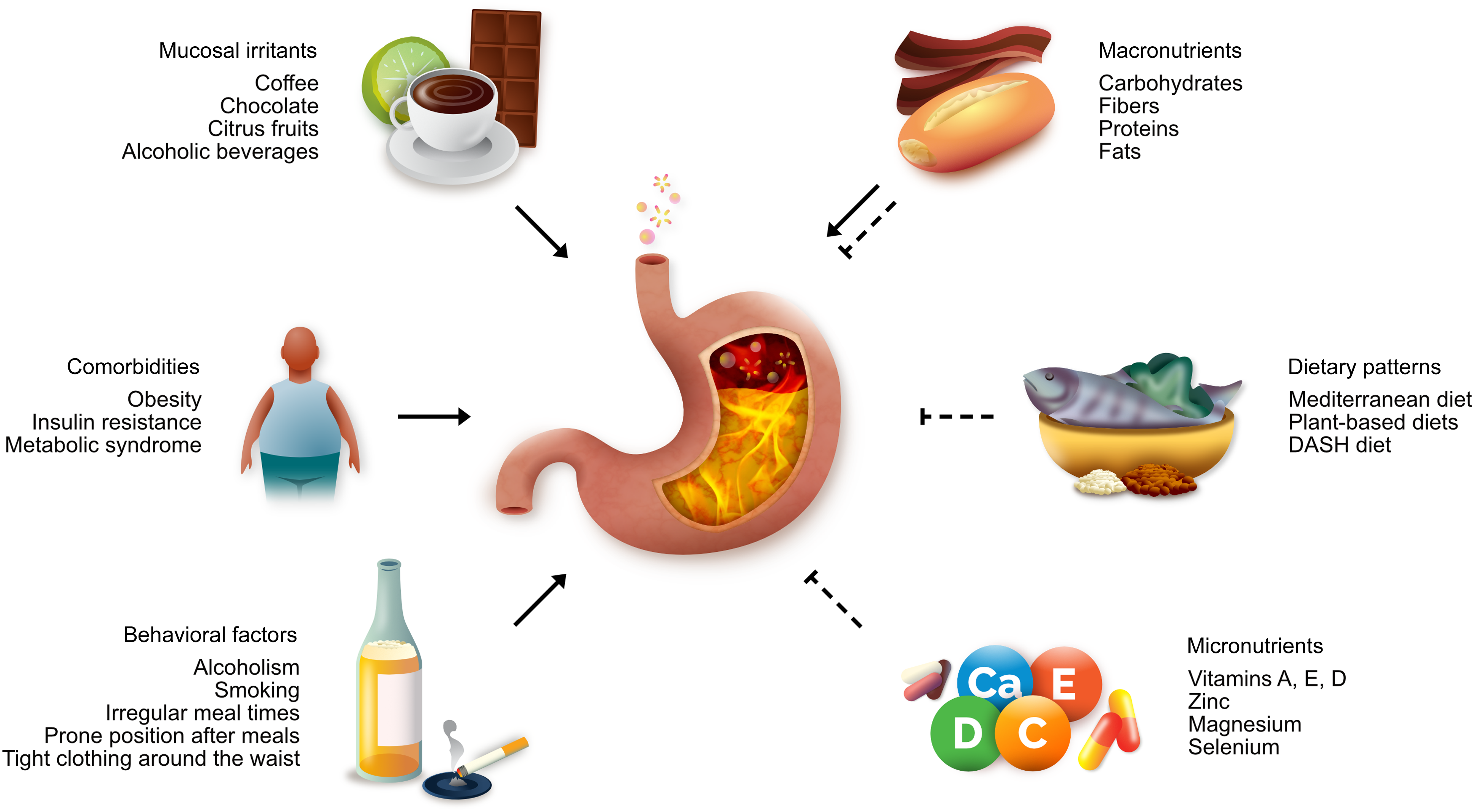
Gastroesophageal reflux disease (GERD) is a prevalent condition observed across various medical specialties, including gastroenterology, otorhinolaryngology, surgery and primary care. Despite the routine prescription of proton pump inhibitors, some patients fail to experience adequate symptom relief. This review delves into the multifactorial mechanisms of reflux, which extend beyond hydrochloric acid to include pepsin, bile acids and trypsin. These factors significantly contribute to mucosal injury in GERD and are influenced by dietary composition. Moreover, dietary patterns with anti-inflammatory properties, such as the Mediterranean and dietary approaches to stop hypertension diets, have shown potential in GERD managing, particularly in the context of obesity–an important risk factor.