Devastating physical morbidity and mortality outcomes due to coronavirus disease 2019 (COVID-19) have been mitigated by(1,Reference Madhav, Oppenheim and Gallivan2) social distancing and quarantine measures(Reference Ismail, Materwala and Znati3), with significant direct and indirect health implications. Although lockdown has reduced the ‘R number’, physical well-being may have suffered from increased levels of stress, anxiety and mental health issues(Reference Khan and Moverley Smith4–Reference Every-Palmer, Jenkins and Gendall6). Moderate weight gain in people with a normal BMI has an adverse effect on metabolism, which increases the risk of diabetes, CVD(Reference Mozaffarian, Hao and Rimm7) or long-term ill-health(Reference Khan, Hashim and Mustafa8). Lockdown may precipitate weight gain similar to that seen during the 6-week summer holidays because of increased inactive time spent at home and snacking on energy-dense foods(Reference Gallo, Moritz and Akison9–Reference Diaz-Zavala, Castro-Cantú and Valencia11). Rundle and colleagues argued that the extent and haste of the restrictions have exaggerated these observations(Reference Rundle, Park and Herbstman12) leading to rapid weight gain. This presents particular issues with the gained weight being more difficult to shed(Reference Mason, Farley and Pallan13). Moreover, physical and social isolation is a recognised risk factor for obesity(Reference Hafner, Hough and Getz14), with weight due to overconsumption, particularly when large “emergency” food stores are present(Reference Pearl15). Reduced physical activity has further exacerbated the weight gain.
The COVID-19 outbreak adversely affected food supply and demand on a global scale(Reference Laborde, Martin and Swinnen16). For some, lockdown gave more time to cook and overconsume, while those who were financially disadvantaged suffered from malnutrition and weight loss because of inflated food prices and food insecurity(Reference Huizar, Arena and Laddu17,18) .
Recent research has linked obesity to an increased risk of contracting severe infections of COVID-19, thereby increasing the risk for extended hospitalisation and increased mortality(Reference Cuschieri and Grech19). Importantly, therapeutic interventions and prophylactic treatments are more difficult and less effective in this group(Reference Di Renzo, Gualtieri and Pivari20–Reference Zachary, Brianna and Brianna25), with resultant poorer outcomes. Thus, weight gain secondary to pandemic confinement has an increased significance.
As the pandemic unfolds, researchers all over the globe try to better understand the prevalence, factors involved and impact of weight change in order to guide prevention strategies that will address this major public health crisis. These efforts have led to the identification of multiple determinants including biological, psychological and sociological processes that influence body weight during the pandemic. In this report, the interplay between these factors has been extrapolated from a systematic review of the current literature. Through an analysis of these observations, future public health interventions can be determined.
Materials and methods
Methods and analysis
This review has been informed by the Cochrane Handbook for Systematic Reviews of Interventions(Reference Higgins, Thomas and Chandler26) and is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses(Reference Moher, Liberati and Tetzlaff27). The review protocol is registered in the PROSPERO International Register of Systematic Reviews (Registration number CRD42020193440). This systematic review did not need approval from the ethics committee or required informed consent from the study populations as the data were retrieved from open-source databases and internet searches.
Search strategy
A medical librarian (L.Ö.) performed a comprehensive literature search in the electronic databases PubMed Embase, Scopus, PsycInfo, Cochrane, CINAHL and Web of Science in June and July of 2020. Search terms related to ‘pandemics’ AND ‘body weight’ AND ‘confinement’ were systematically developed with the help of PubMed and PubMed’s MeSH and reviewed and discussed with a subject specialist (M.A.B.K.). The search string developed in PubMed was later adapted and applied to all databases. A combination of the search fields of ‘Title’, ‘Abstract’ and MeSH/Thesaurus (when available) was used to ensure the best possible search precision and results. No filters or limitations were applied to ensure the inclusion of pre-indexed materials. All databases were searched from their inception until July 2020. Selected sources of grey literature and the preprint archive medRxiv were additionally included in the literature search. A search update in PubMed and Scopus was conducted on 1 February 2021. No additional relevant studies were located after hand screening the results from the updated search.
A search log with database specifications, detailed search strings, results and notes for all sources included in the search is available in online Supplementary Appendix 1.
Inclusion and exclusion criteria
All study designs relevant to human pandemic confinements and their effects on body weight were included (Table 1). All age groups were included, and there were no language restrictions.
Table 1. Inclusion and exclusion criteria
This review was extended to articles published from the time of inception until 1 July 2020 and from an update in PubMed and Scopus on 1 February 2021. The primary outcome was to determine the effects of pandemic confinements on body weight. The secondary research outcome was to identify factors affecting body weight during pandemic confinements.
We excluded animal studies and studies investigating the effect of obesity or overweight on various outcomes during the pandemic. We also excluded studies that only narrated the effects of obesity or overweight as a risk factor worsening pandemic-related disease. Studies on diseases, such as HIV, measles and mumps, were also excluded.
Screening and selection
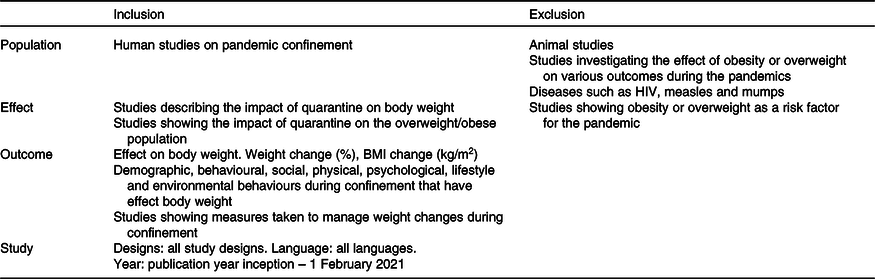
All references identified in the databases and grey searches (n 5070) were uploaded to the systematic review tool Covidence (Veritas Health Innovation, 2020) for automatic deduplication and blinded screening (Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram (Fig. 1)). Two reviewers (H.M. and M.A.B.K.) independently screened the references at both the title/abstract (n 2361) and full-text level (n 78). A third reviewer (P.M.) resolved any conflicts. The grey references and preprints were screened and deduplicated manually by M.A.B.K. and L.Ö. Finally, the reference lists of the included papers were hand screened. Those full-text articles that did not meet the inclusion criterion were excluded (n 27) (Fig. 1). One study investigating weight gain exclusively in pregnant women was excluded(Reference Zhang, Zhang and Huo28) as it was impossible to distinguish physiological from pandemic-related weight gain in this group.
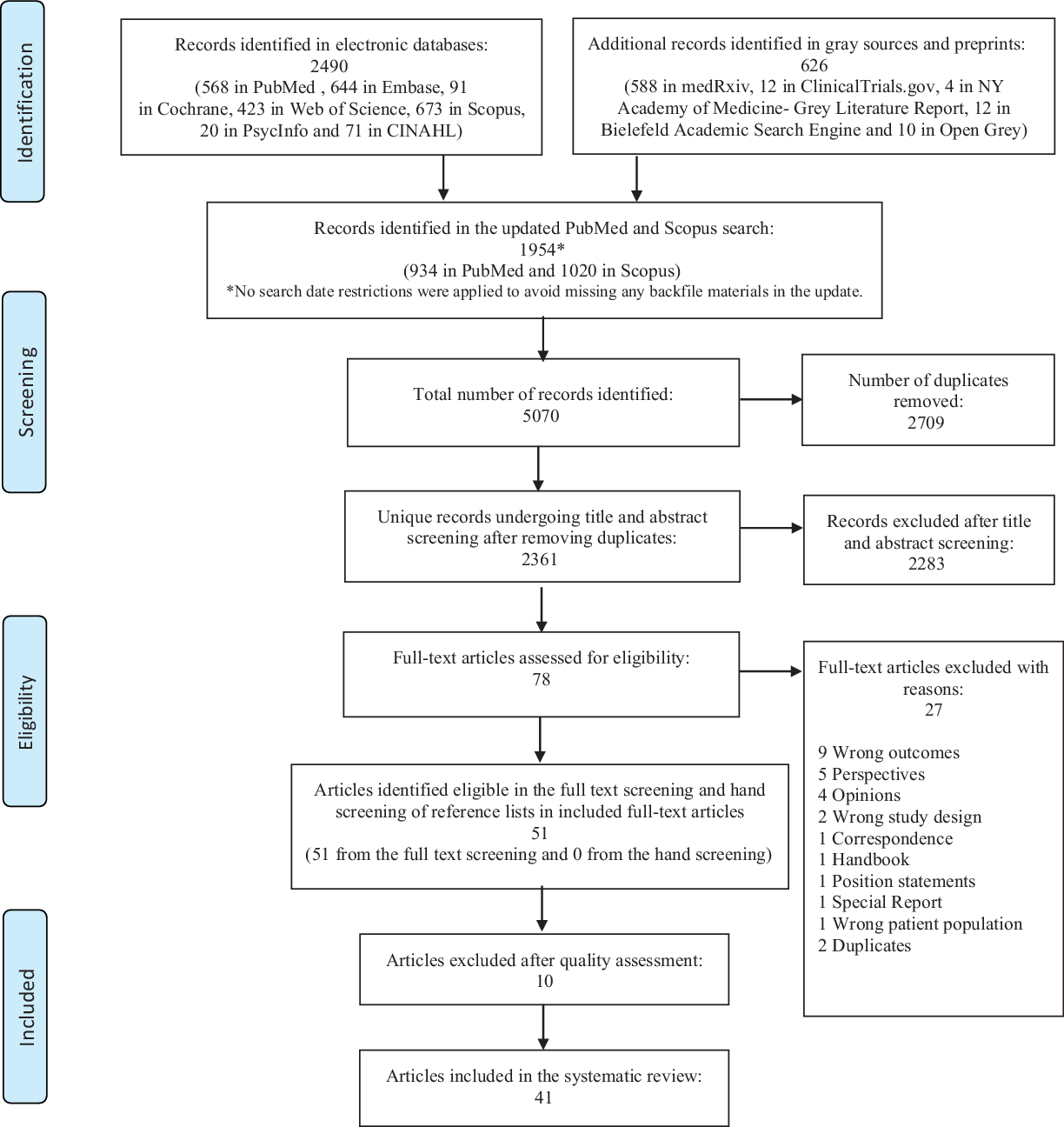
Fig. 1. PRISMA flow chart showing the screening process.
Data extraction
The study characteristics including the authors, year of publication, country of origin, study design, research instruments used, validity of survey questionnaire, proportion of female participants, age range and mean age of participants, mean BMI of participants and mean weight of participants were extracted by one reviewer (M.A.B.K.). The other reviewers (P.M., R.G. and A.M.B.A.S.) extracted and reviewed the data independently. Determinants that had an impact on body weight were extracted and reviewed (primarily by M.A.B.K. and secondarily by P.M., R.G. and A.M.B.A.S.).
Quality assessment (n 51)
Two reviewers (M.A.B.K. and P.M.) independently performed a quality assessment of the fifty-one studies identified as eligible in the screening (online Supplementary Appendix 2). We applied a validated Newcastle–Ottawa Quality Assessment Scale to assess the quality of the studies that were included in the review(Reference Herzog, Álvarez-Pasquin and Díaz29–Reference Peterson, Welch and Losos31). Quality scores obtained via the Newcastle–Ottawa scale for cross-sectional, cohort studies and case–control studies were used to assess selection, comparison and outcomes. Score disagreements were resolved through a discussion between M.A.B.K. and P.M., and a final consensual rating was assigned to each study. Studies six or more stars were considered high quality and were included in the review. Studies with fewer than six stars were excluded (online Supplementary Appendix 2).
Results (n 41)
Categorisation of determinants
Ten studies met the inclusion criteria covering pandemic confinements and their effects. These were then further subdivided into the following five main categories:
-
a. Demographic determinants
-
b. The impact of pandemic confinements on body weight
-
c. Dietary changes and other lifestyle behaviour changes during the confinement
-
d. Behaviour changes observed in obese participants
-
e. Determinants of obesity during pandemic confinements.
Our search yielded 5070 records of which 2361 unique studies remained after deduplication. After applying the inclusion and exclusion criteria in the title and abstract screening, seventy-eight articles were eligible for full-text screening (Fig. 1). We excluded ten studies based on a quality assessment of the results, and twenty-seven studies were excluded based on reasons presented in the Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram (Fig. 1). The range of observations covered dietary choices(Reference Mason, Farley and Pallan13,Reference Di Renzo, Gualtieri and Pivari20–Reference Zachary, Brianna and Brianna25,Reference Cheikh Ismail, Osaili and Mohamad32–Reference Dondi, Candela and Morigi35,Reference Dondi, Candela and Morigi35–Reference Chagué, Boulin and Eicher46) , lifestyle changes in children(Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Dondi, Candela and Morigi35,Reference Shah, Karguppikar and Bhor47–Reference Dragun, Veček and Marendić50) , physical activity levels(Reference Cheikh Ismail, Osaili and Mohamad32–Reference Di Santo, Franchini and Filiputti34,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Keel, Gomez and Harris37–Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42,Reference Martínez-de-Quel, Suárez-Iglesias and López-Flores45,Reference Chagué, Boulin and Eicher46,Reference Adıbelli and Sümen48,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Giustino, Parroco and Gennaro52–Reference Ruissen, Regeer and Landstra59) , psychosocial factors(Reference Mitchell, Yang and Behr21,Reference Pellegrini, Ponzo and Rosato22,Reference Zachary, Brianna and Brianna25,Reference Keel, Gomez and Harris37,Reference Jimenez, de Hollanda and Palou43,Reference Marchitelli, Mazza and Lenzi44,Reference Dragun, Veček and Marendić50,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Chopra, Ranjan and Singh54,Reference Cransac-Miet, Zeller and Chagué55,Reference Malkawi, Almhdawi and Jaber57,Reference Ahmed60,Reference Gentile, Torales and O’Higgins61) , socio-economic factors(Reference Pellegrini, Ponzo and Rosato22,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Shah, Karguppikar and Bhor47,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Rogers, Roberts and Waterlow53,Reference Ahmed60) and sleeping patterns(Reference Zachary, Brianna and Brianna25,Reference Martínez-de-Quel, Suárez-Iglesias and López-Flores45,Reference Dragun, Veček and Marendić50,Reference Romero-Blanco, Rodríguez-Almagro and Onieva-Zafra62) .
Demographic determinants (study and sample characteristics) (n 41)
Table 2 describes the characteristics of each of the forty-one included studies. All of the studies were published in 2020 and 2021. Two studies were from preprints and were included after assessing their qualities individually(Reference Mitchell, Yang and Behr21,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51) .
Table 2. Characteristics of included studies
(Mean values and standard deviations)
BMI in children; NR, not reported.
The included studies had the following countries of origin: Brazil(Reference de Matos, Aidar and Almeida-Neto58), China(Reference He, Xian and Lv39,Reference Jia, Zhang and Yu56) , Croatia(Reference Dragun, Veček and Marendić50,Reference Dogas, Kalcina and Dodig63) , France(Reference Chagué, Boulin and Eicher46,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Cransac-Miet, Zeller and Chagué55) , Jordan(Reference Malkawi, Almhdawi and Jaber57), India(Reference Shah, Karguppikar and Bhor47,Reference Chopra, Ranjan and Singh54) , Iraq(Reference Ahmed60), Italy(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Di Santo, Franchini and Filiputti34,Reference Dondi, Candela and Morigi35,Reference Marchitelli, Mazza and Lenzi44,Reference Marchitelli, Mazza and Lenzi44,Reference Giustino, Parroco and Gennaro52) , Korea(Reference Kang, Jeong and Suh49), Lithuania(Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38), Netherlands(Reference Ruissen, Regeer and Landstra59), Poland(Reference Sidor and Rzymski24,Reference Błaszczyk-Bębenek, Jagielski and Bolesławska41,Reference Dragun, Veček and Marendić50) , Spain(Reference Jimenez, de Hollanda and Palou43,Reference Martínez-de-Quel, Suárez-Iglesias and López-Flores45,Reference Romero-Blanco, Rodríguez-Almagro and Onieva-Zafra62) , Turkey(Reference Ozden and Parlar Kiliç42,Reference Adıbelli and Sümen48,Reference Onmez, Gamsızkan and Özdemir64,Reference Karatas, Yesim and Beysel65) , United Arab Emirates(Reference Cheikh Ismail, Osaili and Mohamad32), UK(Reference Rogers, Roberts and Waterlow53) and the USA(Reference Zachary, Brianna and Brianna25,Reference Keel, Gomez and Harris37,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Mason, Barrington-Trimis and Leventhal66) . Furthermore, multi-regional studies conducted intercontinentally(Reference Mitchell, Yang and Behr21), among eighteen countries in the Middle East and North Africa region(Reference Ismail, Osaili and Mohamad33), and Paraguay and Italian-based multinational researches(Reference Gentile, Torales and O’Higgins61) are included in our analysis.
Altogether, the studies enrolled 469 362 participants. The participants ranged in age from 6 to 86 years, and the mean ages for the individuals studied ranged from 9·9 to 74·3 years. The proportion of female participants ranged from 37 % to 100 %. The number of participants in the included studies ranged from 41 to 381 564. All studies included both male and female participants except one study(Reference Drywień, Hamulka and Zielinska-Pukos36). The duration of confinement for the selected studies for this systematic review ranged between 1 and 24 weeks.
Impact of confinement on body weight
In our study, 7·2–72·4 % of all participants including both adults and children experienced an increase in body weight during the confinement periods(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Sidor and Rzymski24,Reference Zachary, Brianna and Brianna25,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Di Santo, Franchini and Filiputti34–Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38–Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42–Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Chopra, Ranjan and Singh54,Reference Jia, Zhang and Yu56–Reference Gentile, Torales and O’Higgins61,Reference Dogas, Kalcina and Dodig63–Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) (Fig. 2). The mean weight gain ranged from 0·6 (sd 1·3) to 3·0 (sd 2·4) kg. There was a higher weight gain among participants who self-reported stress(Reference Zachary, Brianna and Brianna25,Reference Marchitelli, Mazza and Lenzi44,Reference Chopra, Ranjan and Singh54,Reference Cransac-Miet, Zeller and Chagué55,Reference Malkawi, Almhdawi and Jaber57,Reference Ahmed60,Reference Gentile, Torales and O’Higgins61) , anxiety and depression(Reference Pellegrini, Ponzo and Rosato22,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Malkawi, Almhdawi and Jaber57,Reference Ahmed60,Reference Gentile, Torales and O’Higgins61) . Weight loss was observed in 11·1–32·0 % of participants(Reference Di Renzo, Gualtieri and Pivari20,Reference Sidor and Rzymski24,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Di Santo, Franchini and Filiputti34,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference He, Xian and Lv39,Reference Dragun, Veček and Marendić50,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Chopra, Ranjan and Singh54,Reference Ruissen, Regeer and Landstra59,Reference Onmez, Gamsızkan and Özdemir64,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) . The mean experienced weight loss ranged from 2·0 (sd 1·4) to 2·9 (sd 1·5) kg.
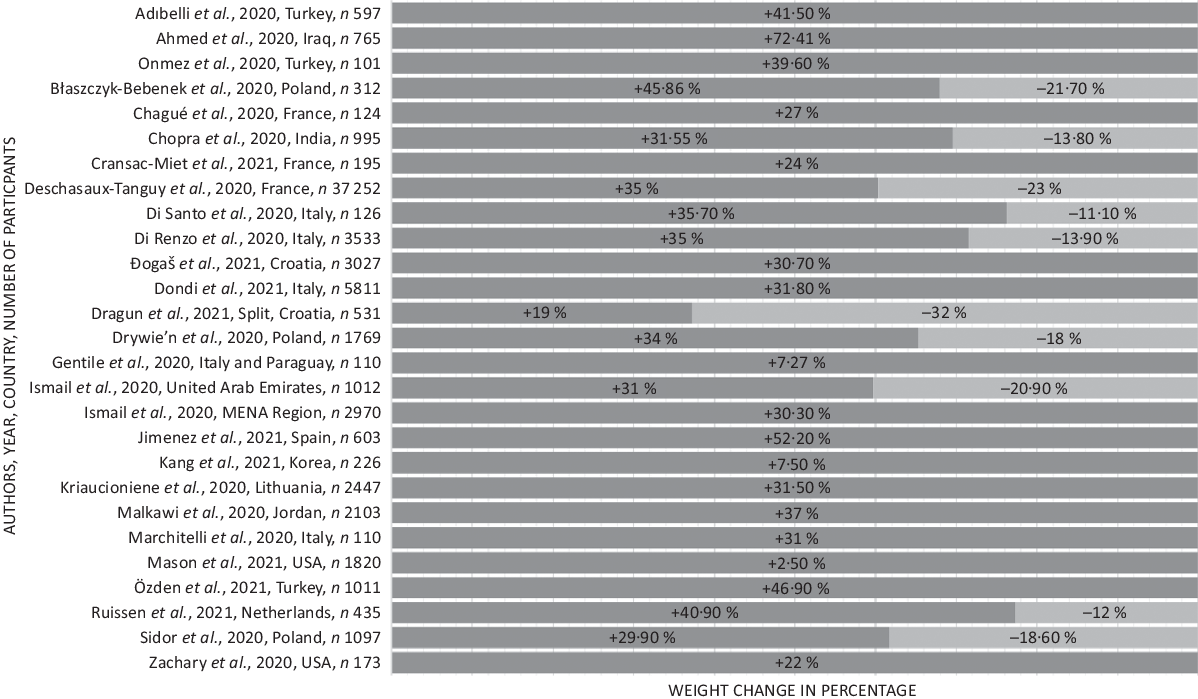
Fig. 2. Body weight changes during pandemic confinements. Selected studies showing percentage of body weight changes. For the full list of weight changes, please refer to Table 3. +, increase in weight; −, decrease in weight.
Dietary and other lifestyle behaviour changes during confinement
Table 3 describes dietary and behavioural changes that were caused by pandemic-related confinements. Most studies reported an increase in food intake associated with increased snacking(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Sidor and Rzymski24,Reference Zachary, Brianna and Brianna25,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Ismail, Osaili and Mohamad33,Reference Dondi, Candela and Morigi35,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42,Reference Jimenez, de Hollanda and Palou43,Reference Dragun, Veček and Marendić50,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Chopra, Ranjan and Singh54,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) and all these studies documenting perceived weight gain(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Sidor and Rzymski24,Reference Zachary, Brianna and Brianna25,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Ismail, Osaili and Mohamad33,Reference Dondi, Candela and Morigi35,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42,Reference Jimenez, de Hollanda and Palou43,Reference Dragun, Veček and Marendić50,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Chopra, Ranjan and Singh54,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) .
Table 3. Behavioural and dietary changes related to pandemic confinements
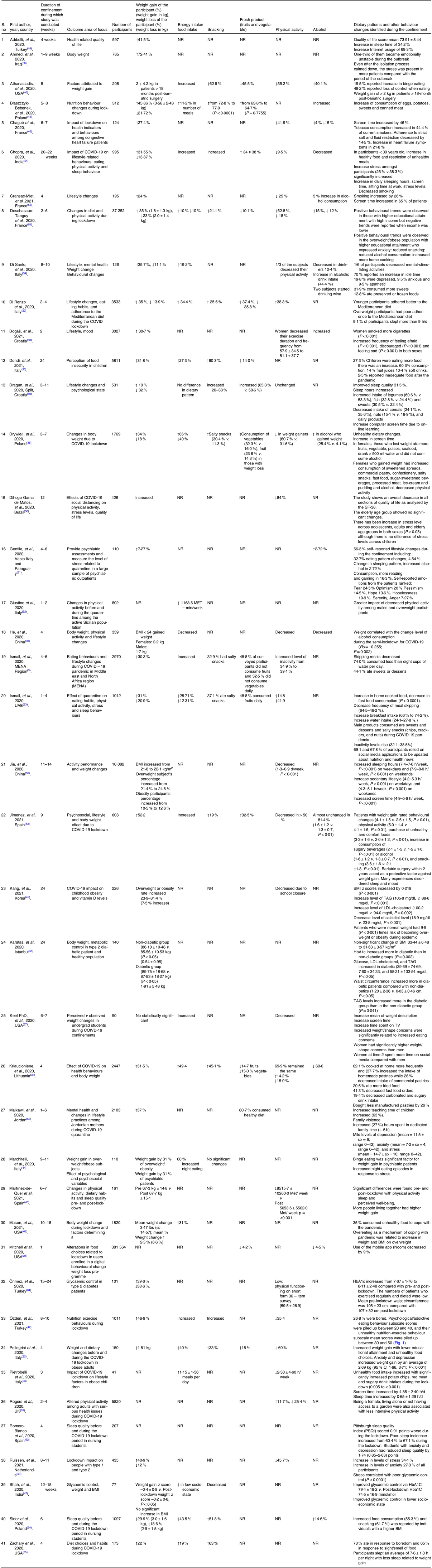
↑, increased; ↓, decreased; NR, not reported; MET–minute/week, metabolic equivalent of task minute/week; IQR, interquartile range; lbs, pound.
Appetite was modified either negatively or positively and was associated with employment change, suspension or working from home(Reference Di Renzo, Gualtieri and Pivari20,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Giustino, Parroco and Gennaro52,Reference Malkawi, Almhdawi and Jaber57) or due to suspension of school attendance(Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Shah, Karguppikar and Bhor47–Reference Kang, Jeong and Suh49) .
The initiating factors were as follows: response to smell and sight of food(Reference Sidor and Rzymski24,Reference Zachary, Brianna and Brianna25) , boredom, binge eating and food cravings(Reference Sidor and Rzymski24,Reference Zachary, Brianna and Brianna25,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42,Reference Marchitelli, Mazza and Lenzi44,Reference Chopra, Ranjan and Singh54,Reference Mason, Barrington-Trimis and Leventhal66) , snacking post dinner(Reference Zachary, Brianna and Brianna25,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Ismail, Osaili and Mohamad33,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38) and visual stimulation through social media(Reference Cheikh Ismail, Osaili and Mohamad32). A significant correlation was observed between snacking, the consumption of high density processed food and a higher BMI(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Sidor and Rzymski24,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38) . Increased energy intake by 10–49·4 % was observed among study participants(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Sidor and Rzymski24,Reference Zachary, Brianna and Brianna25,Reference Cheikh Ismail, Osaili and Mohamad32–Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42–Reference Marchitelli, Mazza and Lenzi44,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Chopra, Ranjan and Singh54,Reference Mason, Barrington-Trimis and Leventhal66) , particularly those with an increased consumption of high density processed foods(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Di Santo, Franchini and Filiputti34–Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42,Reference Jimenez, de Hollanda and Palou43,Reference Dragun, Veček and Marendić50,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) , female sex(Reference Di Renzo, Gualtieri and Pivari20,Reference Di Santo, Franchini and Filiputti34,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Ozden and Parlar Kiliç42,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Dogas, Kalcina and Dodig63) or with a higher BMI(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22–Reference Sidor and Rzymski24,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Jimenez, de Hollanda and Palou43,Reference Marchitelli, Mazza and Lenzi44,Reference Adıbelli and Sümen48,Reference Dogas, Kalcina and Dodig63) . There was an increase in the number of meals eaten per day(Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Dondi, Candela and Morigi35,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Marchitelli, Mazza and Lenzi44,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) and participants ate more than usual(Reference Di Santo, Franchini and Filiputti34,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Ozden and Parlar Kiliç42,Reference Chopra, Ranjan and Singh54) . The proportion of respondents engaged in cooking increased from 40 % to 62 % in our study sample(Reference Sidor and Rzymski24,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51) . Likewise, consumption of homemade recipes increased(Reference Pellegrini, Ponzo and Rosato22,Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Ismail, Osaili and Mohamad33,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51) and eating homemade desserts increased compared with pre-lockdown(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22,Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Di Santo, Franchini and Filiputti34,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) .
Less than one-third of the surveyed participants consumed fresh fruits and vegetables on a daily basis, while a similar number consumed sweets and desserts every day(Reference Di Renzo, Gualtieri and Pivari20,Reference Mitchell, Yang and Behr21,Reference Sidor and Rzymski24,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference He, Xian and Lv39,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51) . In contrast, some studies have shown a decrease in unhealthy food consumption(Reference Pellegrini, Ponzo and Rosato22,Reference Ismail, Osaili and Mohamad33,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Chopra, Ranjan and Singh54,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) .
Where Mediterranean diet was followed, 18- to 30-year-olds were more compliant than other age groups(Reference Di Renzo, Gualtieri and Pivari20). Inverse associations were found between adherence to Mediterranean diet and BMI(Reference Di Renzo, Gualtieri and Pivari20,Reference Dragun, Veček and Marendić50) . A total of 54 % of respondents used leftovers for at least a third of meals, and those who shopped at farmers’ markets or local or organic markets ate up leftovers more (OR = 1·468, P < 0·001)(Reference Di Renzo, Gualtieri and Pivari20). Among app users, mobile behavioural change app interaction was reduced by 9 %(Reference Mitchell, Yang and Behr21). Eating in response to stress was associated with weight gain(Reference Zachary, Brianna and Brianna25,Reference Di Santo, Franchini and Filiputti34,Reference de Matos, Aidar and Almeida-Neto58,Reference Mason, Barrington-Trimis and Leventhal66) . There was increased alcohol consumption(Reference Sidor and Rzymski24,Reference Chagué, Boulin and Eicher46,Reference Cransac-Miet, Zeller and Chagué55,Reference Gentile, Torales and O’Higgins61,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) during the lockdown, while a decrease in alcohol consumption was also noted compared with pre-COVID-19 in another study(Reference Di Renzo, Gualtieri and Pivari20,Reference Chagué, Boulin and Eicher46) . There was an increase in cigarette smoking generally(Reference Chagué, Boulin and Eicher46,Reference Dragun, Veček and Marendić50,Reference Cransac-Miet, Zeller and Chagué55,Reference Dogas, Kalcina and Dodig63) while in contrast, 3·3 % of the smokers surveyed reported reduced smoking during quarantine(Reference Cuschieri and Grech19).
Although the participants reported spending more time in bed before lockdown(Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Zachary, Brianna and Brianna25,Reference Chopra, Ranjan and Singh54,Reference Jia, Zhang and Yu56) , the overall sleep quality was worse(Reference Martínez-de-Quel, Suárez-Iglesias and López-Flores45,Reference Chopra, Ranjan and Singh54,Reference Romero-Blanco, Rodríguez-Almagro and Onieva-Zafra62) . In contrast, secondary school students felt refreshed on awakening and increased sleeping hours(Reference Dragun, Veček and Marendić50). Weight gain was reported by others to be related to decreased night-time sleep and reduced physical activity time(Reference Zachary, Brianna and Brianna25,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ruissen, Regeer and Landstra59)
Sedentary lifestyle and screen time increased during the lockdown(Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Zachary, Brianna and Brianna25,Reference Keel, Gomez and Harris37,Reference Chagué, Boulin and Eicher46,Reference Chopra, Ranjan and Singh54–Reference Jia, Zhang and Yu56) . Those participants who were not currently working or those who started working from home felt that they gained more weight compared with participants who did not have a change in job routine(Reference Di Renzo, Gualtieri and Pivari20,Reference Di Renzo, Gualtieri and Pivari20,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Malkawi, Almhdawi and Jaber57) .
Physical activity altered by varying amounts, reduced in some studies to between 18 and 84 %(Reference Pellegrini, Ponzo and Rosato22,Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Ismail, Osaili and Mohamad33,Reference Di Santo, Franchini and Filiputti34,Reference He, Xian and Lv39,Reference Chagué, Boulin and Eicher46,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Rogers, Roberts and Waterlow53,Reference Chopra, Ranjan and Singh54,Reference de Matos, Aidar and Almeida-Neto58) . People who were already overweight or obese engaged in less physical activity and had decreased energy expenditure during lockdown(Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Jimenez, de Hollanda and Palou43,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51–Reference Rogers, Roberts and Waterlow53,Reference Cransac-Miet, Zeller and Chagué55,Reference de Matos, Aidar and Almeida-Neto58) . Obese children spent less time participating in sports activities(Reference Pietrobelli, Pecoraro and Ferruzzi23).
By contrast, studies reporting an increase in physical activity(Reference Di Renzo, Gualtieri and Pivari20,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51) found greater engagement in yoga/pilates, functional training, home training, and treadmill use and overall increased training frequency(Reference Di Renzo, Gualtieri and Pivari20).
Behaviour changes observed in obese participants
Weight gain was more common in those already overweight or obese prior to lockdown and in individuals with pre-existing difficulty in weight management(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22–Reference Sidor and Rzymski24,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Jimenez, de Hollanda and Palou43,Reference Martínez-de-Quel, Suárez-Iglesias and López-Flores45,Reference Adıbelli and Sümen48,Reference Dogas, Kalcina and Dodig63) .
Increased snacking and food consumption were observed in participants with a higher BMI(Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Sidor and Rzymski24,Reference Cheikh Ismail, Osaili and Mohamad32,Reference Ismail, Osaili and Mohamad33,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) . Many of the participants agreed that they consumed less fruits and vegetables on a daily basis(Reference Mitchell, Yang and Behr21,Reference Sidor and Rzymski24,Reference Ismail, Osaili and Mohamad33,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51) but more high energy processed foods(Reference Pellegrini, Ponzo and Rosato22–Reference Sidor and Rzymski24,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Jimenez, de Hollanda and Palou43) .
This intake was associated with an enhanced appetite and after-dinner hunger(Reference Di Renzo, Gualtieri and Pivari20,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Marchitelli, Mazza and Lenzi44) . Obese children reported an increase in the number of meals eaten along with an increased consumption of sweetened drinks, potato chips and red meat(Reference Pietrobelli, Pecoraro and Ferruzzi23). A decrease in intensive physical activity was associated with obesity(Reference Rogers, Roberts and Waterlow53). An inverse relationship was found between changes occurring in sporting activities and the number of meals consumed per day(Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Giustino, Parroco and Gennaro52,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) . The participants self-reporting anxiety and depression displayed an estimated weight gain(Reference Pellegrini, Ponzo and Rosato22,Reference Marchitelli, Mazza and Lenzi44,Reference Chopra, Ranjan and Singh54,Reference Cransac-Miet, Zeller and Chagué55,Reference Malkawi, Almhdawi and Jaber57,Reference Gentile, Torales and O’Higgins61) .
Determinants that can influence body weight during pandemics
Table 4 describes the determinants of body weight changes during the pandemic. Many determinants that can influence increased weight gain during confinement were identified via this current systematic review. This includes past behaviours, dietary behaviours, physical activity patterns, work environment, psychosocial and socio-economic factors, and pre-existing co-morbidities.
Table 4. Determinants of body weight during pandemic confinements

Female sex(Reference Di Renzo, Gualtieri and Pivari20,Reference Di Santo, Franchini and Filiputti34,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Ozden and Parlar Kiliç42,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Dogas, Kalcina and Dodig63) , age under 25 years and over 45 years(Reference Sidor and Rzymski24,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Rogers, Roberts and Waterlow53) are in particular at higher risk of gaining weight. Initial weight status, diet quality and physical exercise pattern before lockdown are important factors(Reference Di Renzo, Gualtieri and Pivari20,Reference Pellegrini, Ponzo and Rosato22–Reference Sidor and Rzymski24,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Marchitelli, Mazza and Lenzi44,Reference Adıbelli and Sümen48,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Dogas, Kalcina and Dodig63) . In Chinese(Reference He, Xian and Lv39) and Korean(Reference Kang, Jeong and Suh49) populations, BMI < 24 kg/m2 was associated with weight gain. However, some observed that those who were underweight before confinement lost more weight during confinement(Reference Sidor and Rzymski24,Reference Drywień, Hamulka and Zielinska-Pukos36) .
Poor diet quality before the lockdown was associated with weight gain(Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51). Decreased consumptions of legumes, fruits and vegetables(Reference Sidor and Rzymski24,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38) were related to an increased consumption of sweets(Reference Pellegrini, Ponzo and Rosato22–Reference Sidor and Rzymski24). Moreover, more home cooking with consumption of unhealthy foods is associated with increased weight gain(Reference Cuschieri and Grech19,Reference Mitchell, Yang and Behr21,Reference Pellegrini, Ponzo and Rosato22,Reference Ismail, Osaili and Mohamad33–Reference Dondi, Candela and Morigi35,Reference Keel, Gomez and Harris37,Reference He, Xian and Lv39,Reference Błaszczyk-Bębenek, Jagielski and Bolesławska41,Reference Ozden and Parlar Kiliç42,Reference Shah, Karguppikar and Bhor47,Reference Onmez, Gamsızkan and Özdemir64) as is increased alcohol intake(Reference Di Santo, Franchini and Filiputti34,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Chagué, Boulin and Eicher46,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) .
Less intense physical behaviours were noted during lockdown periods compared with behaviours before lockdown causing increased weight gain(Reference Pellegrini, Ponzo and Rosato22,Reference Pietrobelli, Pecoraro and Ferruzzi23,Reference Zachary, Brianna and Brianna25,Reference Cheikh Ismail, Osaili and Mohamad32–Reference Di Santo, Franchini and Filiputti34,Reference Drywień, Hamulka and Zielinska-Pukos36–Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Ozden and Parlar Kiliç42,Reference Martínez-de-Quel, Suárez-Iglesias and López-Flores45,Reference Chagué, Boulin and Eicher46,Reference Adıbelli and Sümen48,Reference Giustino, Parroco and Gennaro52,Reference Chopra, Ranjan and Singh54–Reference Ruissen, Regeer and Landstra59) . This was due to the limitations of outdoor activities and in-gym activities(Reference Di Renzo, Gualtieri and Pivari20,Reference Ozden and Parlar Kiliç42,Reference Giustino, Parroco and Gennaro52) . In addition, there has been more sedentary behaviour with increased screen time(Reference Pellegrini, Ponzo and Rosato22,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Keel, Gomez and Harris37,Reference Chagué, Boulin and Eicher46) which has been associated with weight gain.
Changed working habits, whether furloughed or working from home during the lockdown or those who had their job suspended(Reference Di Renzo, Gualtieri and Pivari20,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Malkawi, Almhdawi and Jaber57) , having children aged < 18 years at home(Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51), urban residence and attaining a lower educational level(Reference Pellegrini, Ponzo and Rosato22) were associated with weight gain.
Patients with pre-existing psychiatric co-morbidities had weight gain during COVID-19 lockdown(Reference Di Santo, Franchini and Filiputti34,Reference Keel, Gomez and Harris37,Reference Jimenez, de Hollanda and Palou43,Reference Marchitelli, Mazza and Lenzi44,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Gentile, Torales and O’Higgins61) , and stress(Reference Mitchell, Yang and Behr21,Reference Zachary, Brianna and Brianna25,Reference Marchitelli, Mazza and Lenzi44,Reference Chopra, Ranjan and Singh54,Reference Cransac-Miet, Zeller and Chagué55,Reference Cransac-Miet, Zeller and Chagué55,Reference Malkawi, Almhdawi and Jaber57,Reference Ahmed60,Reference Gentile, Torales and O’Higgins61) , anxiety and/or depression(Reference Pellegrini, Ponzo and Rosato22,Reference Malkawi, Almhdawi and Jaber57,Reference Ahmed60,Reference Gentile, Torales and O’Higgins61) , eating in response to stress(Reference Mitchell, Yang and Behr21,Reference Zachary, Brianna and Brianna25) , boredom(Reference Pellegrini, Ponzo and Rosato22), living alone(Reference Pellegrini, Ponzo and Rosato22), emotional eating(Reference Mitchell, Yang and Behr21,Reference Ozden and Parlar Kiliç42,Reference Marchitelli, Mazza and Lenzi44) or weight or body shape concerns(Reference Keel, Gomez and Harris37) were associated with an increase in body weight during confinement. Decreased sleeping time(Reference Zachary, Brianna and Brianna25) or poor quality sleep(Reference Martínez-de-Quel, Suárez-Iglesias and López-Flores45,Reference Dragun, Veček and Marendić50,Reference Romero-Blanco, Rodríguez-Almagro and Onieva-Zafra62) was further associated with weight gain.
Socio-economic factors such as urban residence(Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Ahmed60) , lack of access to garden(Reference Rogers, Roberts and Waterlow53), lower socio-economic level(Reference Shah, Karguppikar and Bhor47) or lower education levels(Reference Pellegrini, Ponzo and Rosato22) and residence in a macroeconomic region(Reference Drywień, Hamulka and Zielinska-Pukos36) were associated with significant gain in the weight.
Patients with chronic illness such as diabetes, hypertension, lung disease, chronic CHD, congestive heart failure, depression or disability affecting one or more activities of daily living or lower levels of physically activity had an increase in weight(Reference Di Santo, Franchini and Filiputti34,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Marchitelli, Mazza and Lenzi44,Reference Chagué, Boulin and Eicher46,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Rogers, Roberts and Waterlow53,Reference Cransac-Miet, Zeller and Chagué55,Reference Gentile, Torales and O’Higgins61,Reference Onmez, Gamsızkan and Özdemir64) .
Those who were previously underweight before the lockdown tended to lose more weight(Reference Sidor and Rzymski24,Reference Sidor and Rzymski24,Reference Drywień, Hamulka and Zielinska-Pukos36) . Those whose diet included more fruits and vegetables, pulses and drank more water lost weight(Reference Drywień, Hamulka and Zielinska-Pukos36).
Discussion
This systematic review highlights contrasting effects of pandemic confinements on body weight, and we identified specific factors associated with change in body weight during the lockdown periods.
A BMI of > 25 kg/m2 was identified as an independent risk factor for increased food intake during lockdown(Reference Huber, Steffen and Schlichtiger68). Other influences were inadequate sleep, decreased physical activity, emotional eating in response to stress, lack of control in dietary habits(Reference Di Renzo, Gualtieri and Pivari20,Reference Sidor and Rzymski24,Reference Rogers, Roberts and Waterlow53) and increased alcohol consumption and smoking(Reference Di Santo, Franchini and Filiputti34,Reference Drywień, Hamulka and Zielinska-Pukos36,Reference Kriaucioniene, Bagdonaviciene and Rodríguez-Pérez38,Reference Dragun, Veček and Marendić50,Reference Cransac-Miet, Zeller and Chagué55,Reference Dogas, Kalcina and Dodig63,Reference Blaszczyk-Bębenek, Jagielski and Boleslawska67) . The impact of these influences is more significant in the obese population.
Eating habits as well as diet composition are linked to weight gain(Reference Newman, O’Connor and Conner69). Increased snacking after meals, particularly post dinner, was associated with weight gain(Reference Newman, O’Connor and Conner69). Jakubowicz et al. also concluded that increased energy content at dinner increased the subjects’ weight(Reference Jakubowicz, Barnea and Wainstein70). Thus, decreasing food consumption during and post dinner should be recommended.
Social networks, neighbourhood social activities and physical activity can influence an individual’s opportunity to make better choices contributing to protection from obesity(Reference McNeill, Kreuter and Subramanian71). The absence of these influences during extended lockdown periods may facilitate a more obesogenic environment, thus encouraging weight gain(Reference Swinburn, Egger and Raza72).
By contrast, not all effects of pandemic confinement resulted in weight gain. In an Italian study, 38 % of participants adhered to a Mediterranean diet. This may have been assisted by the Italian Ministry of Health publishing online materials regarding favourable lifestyle choices during the lockdown in April 2020 and providing practical guidelines on healthy behaviours(Reference Gallè, Sabella and Da Molin73,74) .
Pandemic confinements undoubtedly increase stress(Reference Ismail, Osaili and Mohamad33,Reference Cransac-Miet, Zeller and Chagué55,Reference de Matos, Aidar and Almeida-Neto58–Reference Ahmed60) , 73 and 83 % of respondents experienced an increase in anxiety and depression, respectively, with 70 % reporting weight management issues, stock-piling food and stress eating(Reference Pellegrini, Ponzo and Rosato22,Reference Athanasiadis, Hernandez and Hilgendorf40,Reference Almandoz, Xie and Schellinger75) . Weight loss was reported in three studies by 13–19 % of participants(Reference Di Renzo, Gualtieri and Pivari20,Reference Sidor and Rzymski24,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51) . Two studies showed stress-related weight among working professionals and university students(Reference Kivimäki, Head and Ferrie76,Reference Serlachius, Hamer and Wardle77) . The mechanism is twofold and results from decreased, unchanged or increased energy intake coupled with adaptive adrenergic stimulated thermogenesis involving brown adipose tissues(Reference Razzoli and Bartolomucci78). The weight loss observed in this systematic review may also be attributed to the negative effect of stress(Reference Di Renzo, Gualtieri and Pivari20,Reference Sidor and Rzymski24,Reference Zachary, Brianna and Brianna25,Reference Deschasaux-Tanguy, Druesne-Pecollo and Esseddik51,Reference Dallman79) .
The link between weight changes and stress has been studied extensively(Reference Adam and Epel80,Reference O’Connor, Jones and Conner81) . Behavioural and physiological explanations suggest that the sensation of eating is associated with a psychological escape from emotional distress(Reference Heatherton and Baumeister82) and that the consumption of high energy foods alleviates stress(Reference Adam and Epel80). During a pandemic, where cities and even entire nations were locked down, fear and anxiety related to COVID-19 induced an over eating behaviour. However, management of this associated condition is difficult(Reference Haddad, Zakhour and Bou Kheir83). The adverse effects of lockdown on the psychological and social well-being of society emphasise the need for strong public health interventions to support particularly at-risk people.
The associations between health outcomes, exercise and physical activity are well-established. The results from studies that we included in this review were mixed; some participants engaged in increased physical activity, while others had lower levels of physical activity. Confinement did not induce many sedentary participants to increase their physical activity. Other unhealthy behaviours such as increased screen time were noted which are similar to previous studies(Reference Khan, Shah and Shehab84). Stress may impair efforts to become physically active; conversely, those who already participate may do so to reduce stress(Reference Stults-Kolehmainen and Sinha85), which may explain the variation in physical activity observed. Seigel et al. describe this as stress-related behavioural activation or inhibition(Reference Seigel, Broman and Hetta86).
Other unhealthy behaviours were noted during the confinement. There was a 14·6 % increase in the consumption of alcohol in participants who had issues with alcohol(Reference Sidor and Rzymski24). In the acute post-disaster period of the September 11 attacks in Manhattan, New York City, the prevalence of alcohol consumption and marijuana use among New York City residents increased over a 5–8-week period(Reference Vlahov, Galea and Resnick87). These results mirror our findings, suggesting shared responses to intense community stresses. Although these activities may not directly affect weight, alcohol consumption and obesity are common risk factors for chronic illnesses leading to increased morbidity and mortality(Reference Chiolero, Faeh and Paccaud88). Furthermore, in a study conducted in the Netherlands, it was reported that overweight and obese individuals found it more difficult to make healthy food choices. More savoury snacks and non-alcoholic beverages were purchased and consumed at home (35·6 %) because of more leisure time (31·5 %) and boredom (21·9 %) during the lockdown(Reference Poelman, Gillebaart and Schlinkert89).
Positive outcomes from confinement have also been reported(Reference Ruiz-Roso, de Carvalho Padilha and Mantilla-Escalante90). These behaviours may result from the increased availability of time to cook, health risk perceptions, lack of negative social distractions(Reference Ferrer and Klein91) and socio-cognitive ideation towards a healthier lifestyle(Reference Raude, Lecrique and Lasbeur92). Long-term studies are necessary to determine whether these constructive and preventive behaviours can be sustained after confinement is over.
Food security, which involves food availability, accessibility and affordability, is another important factor in the relationship between pandemic confinement and body weight changes(Reference Adams, Caccavale and Smith93). Global non-pharmaceutical interventions, such as lockdowns and quarantines, implemented to limit the spread of the virus have seriously impacted food security systems(Reference Micha, Mannar and Afshin94), with the greatest burden affecting communities in which nutritional health is fragile(95). Communities with precarious budgeting practices were destabilised by food price inflation and product shortages. Additional influences on food security included movement restrictions of workers, changes in consumer demand, closure of food production facilities, restricted food trade policies and financial pressures in the food supply chain. As dependence on food banks grew with an exponential increase in demand, basic survival needs presided over healthy dietary choices(Reference Huizar, Arena and Laddu17). Prior to 2020, 690 million people were already food insecure and hungry(96). By the end of 2020, the COVID-19 pandemic had created an additional 270 million food-insecure people(97,Reference Paslakis, Dimitropoulos and Katzman98) . Unfortunately, vulnerable populations are not restricted to under-resourced countries; developed nations are suffering as well. In the USA alone, food insecurity more than doubled as a result of the economic crisis brought on by the outbreak, impacting as many as 23 % of households(Reference Schanzenbach and Pitts99).
Serious ethical and health-related issues hinder healthcare providers working with vulnerable populations. In general, differences in weight status and dietary intake reveal that a trend in obesity increases as the degree of food insecurity increases(Reference El Zein, Colby and Zhou100). The COVID-19 crisis has highlighted food insecurity as a significant factor in nutritional poverty(Reference Micha, Mannar and Afshin94). This awareness of food insecurity may provide nations with the impetus to robustly tackle food-related epidemics, such as obesity and diabetes.
COVID-19 has challenged us to consider the role and balance of healthcare, personal health and holistic well-being. Redefining these dynamics in preparation for future pandemics is imperative to minimise severe impacts to health and resources(Reference Sheth101). It was previously observed that consumerism is affected by internal factors, such as personal character, and external factors, such as economic crises. The pandemic served as an external factor that altered consumer behaviour(Reference Mehta, Saxena and Purohit102).
Relief efforts by governmental and non-governmental agencies achieved temporary solutions without significant public pressure(Reference Baraniuk103), but the demand for aid from all sectors of society is mounting. National governments should take the lead in providing strategic directions that will ensure the continuity of food accessibility to all, particularly the most vulnerable. Focus must be on coordinated and integrated public health programmes through legislative action to end sub-standard dietary conditions endured by those most in need. By collaborating with key stakeholders, health professionals must provide aggressive nutritional counseling to improve dietary habits, and concerted efforts across the board are paramount.
Recent research has shown obesity to be an independent risk factor for severe complications and increased mortality from COVID-19(Reference Hajifathalian, Kumar and Newberry104,Reference Ho, Celis-Morales and Gray105) . The evidence suggests a linear relationship with obesity increasing the risk of severe disease and death among COVID-19 patients(Reference Huang, Yao and Huang106). The co-existence of both pandemics, COVID-19 and obesity, along with the emergence of obesity evolving from lockdown has caused a ‘syndemic’ or a symbiotic pandemic(Reference Hill, Sowers and Mantzoros107). Researchers must address the significant knowledge gaps that have become apparent during this pandemic regarding preparedness and response to such a crisis. Moreover, COVID-19 has disproportionately affected certain populations, and future research should focus on such vulnerable populations to ensure better outcomes.
Strengths and limitations
To our knowledge, this is the first systematic review evaluating the effects of pandemic confinement on body weight. Our study highlights major determinants that can have an impact on body weight during confinement and those that can be targeted in future pandemics to effectively manage body weight during pandemics via public health initiatives. Moreover, confinements are not solely related to pandemics and can also occur during natural disasters or calamities and in prisons. Determinants identified could be modified via appropriate public health measures to reduce negative impacts.
The present study has limitations. First, there was limited evidence from past pandemics related to obesity and morbidity or mortality. This may reflect the recent evolution of worldwide obesity(Reference Eknoyan108). Second, within the common research theme of body weight changes during pandemic confinements, our systematic review found marked heterogeneity in the determinants and measured outcomes. This variation could be explained by differences in the study population and types of outcome measurements(Reference Gagnier, Moher and Boon109). Nevertheless, in our systematic review, we followed a rigorous protocol with clear objectives and inclusion and exclusion criteria. This allowed for the identification and pooling of the determinants of body weight changes during pandemic confinements (Table 4). A thorough and complete identification of the different determinants related to pandemic confinements could guide decision makers. Furthermore, our study calls for further research into the level of impact of each determinant. Third, given the contemporary nature of the pandemic, the literature was primarily related to countries where COVID-19 had an early ‘first wave’ impact. Findings from other continents, particularly from Africa and South America, are yet to emerge. Fourth, online surveys using social media platforms were the predominant data collection method, which has recognised strengths and biases. Although the researchers used this form of data collection to reach a wider population, the likelihood of a bias towards a younger population should be noted. Fifth, although this analysis provides evidence for the effects of confinement on body weight, we are unable to comment on the potential for interventions such as lifestyle changes to attenuate the phenomenon. Sixth, because of the limited number of studies included, we were unable to correct for influences, such as pre-existing diets, and could not quantify the impact of possible factors in isolation. Although we know that weight gain is likely during confinement, further research using more sophisticated data collection techniques is necessary to determine the holistic impact of confinement to provide evidence-based practical solutions for future eventualities.
Conclusion
This systematic review highlights the significant effects that pandemic confinements can have in the short term on body mass. Poor sleep, snacking post dinner, lack of dietary restraint, pre-existing overweight status, emotional eating due to stress and decreased physical activity are risk factors for weight gain.
Preparing for the next ‘wave’ is challenging given the multitude of factors that must be tailored to the local situations and available resources. Planning for future episodes requires a strong, evidence-based national policy in conjunction with clear guidelines to ensure that the negative sequelae of lockdowns are minimised.
Acknowledgements
We thank Gamila Hassan at the National Medical Library at UAEU for her strategic support in locating and uploading full-text articles to Covidence.
The authors received no specific funding for this work.
M. A. B. K., P. M., R. G., L. Ö. and H. M. formulated the research question and designed the study. M. A. B. K., P. M., R. G., K. K. A. and A. M. B. A. S. extracted and reviewed the data independently. L. Ö. and M. A. B. K. performed the literature search. M. A. B. K., P. M., R. G., A. M. B. A. S. and J. N. performed the literature review and data analysis. M. A. B. K., P. M., K. K. A., H. M., R. G, A. M. B. A. S., J. N., L. Ö., J. E. M. S. and J. K. contributed to drafting the paper. M. A. B. K., R. G., P. M., A. M. B. A. S. and K. K. A. equally contributed to all of the work as co-first authors.
We declare that there are no conflicts of financial and commercial interest that could be perceived as prejudicing the impartiality of the present study.
This article was not plagiarised and had not previously been published in other journals.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114521000921