Introduction
Home video visit (HVV), also known as virtual visit or eVisit, is a new means of delivering personalized medical care to patients in their homes via secure video conferencing using personal Internet-enabled devices like smartphones, tablets, and computers. Reference McGrail, Ahuja and Leaver1,Reference Appireddy, Khan and Leaver2 In Canada, the COVID-19 pandemic has resulted in the temporary cancellation of all nonurgent clinical visits to prevent exposure to patients and to reinforce physical distancing measures. Virtual care modalities like HVV have become rapidly implemented across the country to meet healthcare needs and challenges in the midst of the pandemic. Reference Webster3,4
In comparison to in-person visits, HVVs are ideal for providing follow-up care, advising on symptom management, conveying diagnostic results, and collaborating in therapeutic decision-making. The goal of HVV is to provide patient-centered care, reduce per capita healthcare cost, improve healthcare efficiency and healthcare provider satisfaction, and increase accessibility by allowing patients to remain in the comfort of their homes. Reference Verma and Bhatia5 As accessibility, cost, and availability are considered to be ongoing concerns to Canada’s senior population, particularly for those with complicated health conditions, virtual care solutions may serve to alleviate problems to healthcare access. Reference Ganesh, King-Shier, Manns, Hill and Campbell6,Reference Appireddy, Jalini, Shukla and Lomax7 On the flip side, as health literacy and technological familiarity are varied amongst the senior population, virtual care may exacerbate problems to health access.
In the Kingston Health Sciences Centre’s Stroke Prevention Clinic, Appireddy et al. detailed a successfully piloted HVV project. The project met numerous metrics of success and demonstrated a 40% conversion of scheduled in-person follow-up visits to HVVs. Importantly, the patient satisfaction survey showed broad acceptance of this alternative, with >95% reporting savings on time, travel, and money and >90% reporting better or same experience with HVVs compared to in-person care. The pilot project results also demonstrated shorter wait times with HVVs versus in-person appointments (mean 59.98 [SD 48.36] days vs. mean 78.36 [SD 50.54] days; P < 0.001). The estimated savings (opportunity cost for in-person outpatient care) from the HVV pilot study was CAN $23,832–$28,584 using ambulatory care case costing data. 8
While quantitative studies have already noted the benefits of telemedicine modalities like HVVs, the authors of this paper sought to investigate the lived experiences of patients with HVV in order to provide insight into the various social and environmental determinants which may intersect to impact health access in senior stroke patients. Reference Appireddy, Khan and Leaver2 This paper details a qualitative study that sought to explore the experiences of senior stroke patients with HVV for follow-up visits and is one of the first studies examining the “digital determinants” of health in stroke patients from a qualitative perspective.
Social Determinants of Health and Intersectionality Theory
The social determinants of health (SDoH) framework posits that health is determined by the conditions shaped by political, social, and environmental systems in which one is born, grows, works, lives, and ages. Reference Marmot, Allen, Bell, Bloomer and Goldblatt9 The importance of incorporating the SDoH into the healthcare system to address the diverse needs of varying patient population groups unequivocally suggests that SDoH has more impact on inequity in health outcomes than medical care itself. Reference Woolf, Johnson, Phillips and Philipsen10 The SDoHs contribute to health inequities that people experience due to the fact that determinants often intersect to compound and exacerbate health outcomes. Intersectionality theory provides insight into the ways social factors do not work in isolation but in tandem with one another but also with biological and environmental factors to affect health outcomes. Reference Morrison11 Intersectionality is attentive to the individual, institutional, and structural determinants that impede health equity in access and care and rejects the idea that individuals themselves are responsible for their own health. Using both theories, this paper explores the various factors that simultaneously and collectively work to impact or impede health.
Methods
Study Design
We conducted semi-structured interviews with 23 participants in the city of Kingston, as well as the surrounding Frontenac, Lennox, and Addington county who have (1) been affected by stroke and (2) used HVV for follow-up in the Kingston General Hospital. Semi-structured interviews are widely used in qualitative research. Reference Warren, Gubrium and Holstein12 Semi-structured interviews are “interview[s] with the purpose of obtaining descriptions of the lifeworld of the interviewee in order to interpret the meaning of the described phenomena.” Reference Kvale and Brinkmann13 Semi-structured interviews are employed to obtain information about the lived experiences of interviewees without guiding the interviewee into providing a limited or preset answer. Resultantly, semi-structured interviews provide researchers and clinicians with an opportunity to explore at greater depth the responses, themes, and concerns expressed by patient–participants.
As the study team sought to capture the perspectives of participants in rich detail, an ethnographic approach was used as the main methodological approach for conducting the semi-structured interviews. An ethnographic approach privileges narrative retelling and attempts to capture as much detail as possible regarding the experiences, perceptions, and opinions of the participants. To maintain a strong level of rigor in the data collection and analysis, the study team opted to interview a smaller sample of participants in the study. All participants were contacted by phone call to participate in a qualitative study and consented to the study. The medical secretary of the Stroke Prevention Clinic contacted patients who had conducted HVVs between May 2019 and February 2020 and invited them to participate in an interview over the phone.
All HVVs were administered through a secure web platform provided by the Ontario Telemedicine Network. Prior to their visit, the medical secretary would email an instruction sheet to all patients detailing the process involved with conducting an HVV. Specifically, a link would be sent to the patient’s inbox. A few days before the patient’s first HVV, the medical secretary called the patients over the phone to explain the process verbally and to answer any questions that the patient may have. No registration is involved. The selection criteria for this study include patients (aged >64) who have had at least one virtual video visit following stroke. A screening log was however not maintained. The study was approved by the Queen’s University Health Sciences Research Ethics Board.
Data Collection and Analysis
Using the responses of the survey from Appireddy et al.’s (2019) study, the research team created an interview guide that sought to gather insight and descriptive information about patients’ experiences with HVV. Specifically, we sought to collect descriptions about the (1) costs and time associated with in-person visits, (2) facilitators and barriers to in-person and virtual visits, and (3) their values attached to traditional and virtual forms of patient care. The interview guide was created iteratively with input from Kingston Health Science Centre’s Patient Family Advisory Council (PFAC). The involvement of the PFAC in the co-creation of the interview guide was significant as members not only had grounded expertise in patient experiences but also the patients’ best interests in mind. As a result, this process helped to increase knowledge translation and participation between multiple parties with shared interests within the research process.
We collected data using face-to-face interviews at the locations of the participant’s choosing, such as their homes or in other public venues, or phone interviews following physical restrictions during the COVID-19 pandemic. Participants provided informed written or verbal consent. The face-to-face interviews were conducted by a volunteer Patient Family Experience Advisor who was also a member of the hospital’s PFAC (AOR) to build trust and rapport with patients. A member of the research team accompanied each interview and took notes, making comments only when necessary. We sought to conduct the interviews in this format to facilitate trust and openness between the participant and the research team. The phone interviews were conducted by a study team member (SC) or a research assistant. All interviews were captured by an audio recorder and transcribed verbatim by a hired transcriptionist.
Each transcribed interview was subsequently analyzed using NVivo 10 software by a study team member (SC) and a PhD student research assistant using an iterative process. Thematic coding, otherwise known as the identification of major themes from the transcripts, was conducted by a member of the research team. Following every seventh transcript, the codes would be reviewed and refined using a consensus process. Coding was done in two subsequent rounds with the revision of codes in between. Smaller themes identified in the first stage of coding were eventually sorted into broader themes in the second stage of coding.
Results
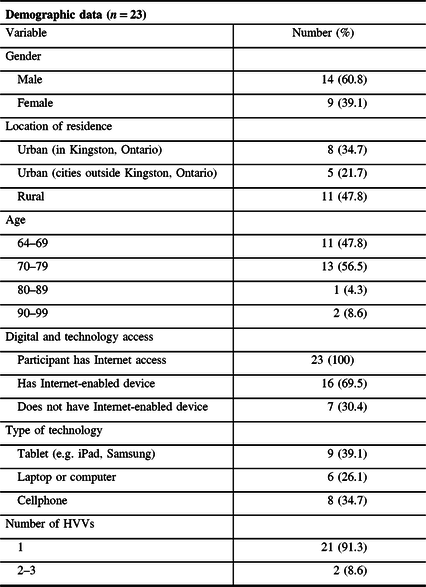
Twenty-three participants were interviewed over the course of a 1-month period. Patients between the ages of 64 and 91 years participated in the study. Fourteen men and nine women participated in the study. All participants were Caucasian. Participants ranged in geography: some lived in the Kingston urban area while others lived in surrounding urban areas and rural areas. All participants lived with at least one caregiver or with their families. The demographic data of the participants can be found in Table 1. In what follows, we explore several overarching themes that emerged from our analysis. We describe the themes and use verbatim quotes from the interview transcripts to support our findings.
Table 1: Demographic data and information about digital access of all participants
Participants Perceived that HVV Was Time-Saving and Convenient for Both Themselves and Physicians
Throughout the interviews, participants were consistent in explaining that simple tasks, like applying make-up or putting on clothes, became difficult to coordinate or do following their stroke. These tasks would become even more difficult if participants were to attend an event at a scheduled time, such as a follow-up visit at the hospital. This is because these difficulties were compounded by various geographical, economic, and biological factors:
It’s saving a lot of time and effort, a lot of time and trouble because if I had to go back down to the Kingston General Hospital, I would’ve been still in the same situation, having to look for parking and having to walk and feeling stressful about what happens if I can’t find parking, am I going to be late for my appointment. That’s all stressful when you’re 70 years of age.
In comparison to traditional forms of in-person visits, some participants noted that HVVs offered greater clarity in terms of verbal communication, guaranteed punctuality, and provided the same services as in-person visit in the comfort of the patient’s homes:
I didn’t have to come in [to the hospital] and I could understand [the doctor] better and it was on time. I knew that 10:30 was 10:30 when he was gonna be there. So it’s all positive as far as I’m concerned. It couldn’t be much better than that, you know. I mean, if there’s any questions I have, I can ask them same as if I’m standing in front of him. And I don’t have to be examined which is a plus for my case.
Other participants noted that HVVs helped them save time and energy in comparison to an in-person visit which is particularly salient given the physical difficulties of having to adjust and heal from stroke:
I have stopped driving, and so [son and caregiver] takes me. Now I – to get up in the morning and make the bed and get in the shower – I’m very slow. It’s at least an hour and a half before I’m ready to come down… I felt that it [HVV] was a way of saving me time and effort. Physical effort.
Participants Perceived that HVVs Increased Physical Accessibility to Healthcare Access
One of the participants in this study lived in a rural area that required a 30-minute drive to the Kingston Health Sciences Centre. While they often did not mind the drive to the hospital, they expressed that HVVs gave them an option to stay safe during the winter or other unsafe weather conditions.
It would be different if you had to go and visit and had to fit in other things [errands] and certainly for the winter it would be a blessing. And if there was something I really felt concerned about I would make an effort to contact his nurse and say, “Could I speak to him either on the computer or live or something or other?” I can see it would be a tremendous advantage to people in the wintertime when your car is covered with snow and you can’t get out it would be tremendous, you know.
Other participants living in rural areas appreciated the ability to stay at home since the drive to the hospital was often tiring, especially when healing from a medical condition:
I had a heart attack after the stroke, so if I had to drive to Kingston, I’d be exhausted when I got there. This way, it was not demanding on me physically because all I had to do was sit in the chair. I didn’t have to drive all the way to Kingston.
The number of participants with aphasia, motor difficulties, comorbidities, and the inability to drive is detailed in Table 2.
Table 2: Disability, motor difficulties, comorbidities, and driving capabilities of all participants

Some Participants Felt Uncomfortable, Unable, or Had Difficulty Using Technology to Conduct HVVs
While most of the participants used handheld Internet-enabled devices such as a smartphone, tablet, or laptop on a daily basis, some participants did not own or use Internet-enabled devices at all. Resultantly, some of the participants had some degree of difficulty navigating or using the technology to conduct the HVVs. In order to overcome challenges, participants often relied on assistance from a younger family member or a caregiver. Take, for example, this participant who was only able to conduct an HVV using their daughter’s iPad.
Participant: I’m really not into electronics [laughs]. That’s because I don’t have a cell phone, you know. I’m not used to doing that. I just have an ordinary phone and… Interviewer: So, what technology did you use to have the e-visit? Participant: Oh, well, my daughter brought her tablet, and she was there. All I had to do was look intelligent and answer the questions, but to me, it was a little unusual because I’m not used to that technology.
Other participants also expressed feeling strange using technology to receive healthcare:
Interviewer: Do you feel it would have been easier to ask a question or to feel comfortable asking a question if you were there in person with the doctor as opposed to on the iPad? Patient: Um, it [in-person visit] probably would have triggered my mind to have asked about so and so, but because I wasn’t used to the computers, it was a little strange.
Participants argued that HVVs would most likely be suitable only for patients who had a strong command of Internet-enabled technology or had help from other family members. A strong Wi-Fi or Internet source is also required, which could pose a problem for residents of the region’s rural areas.
I think for – as long as somebody can understand what’s going on with this [HVV] and follow-through, listen carefully to the instructions and follow through and then wait until a doctor comes on. And it’s just like sitting in your living room basically. Um, I sat in a place where I knew that there was a good connection. That’s the other thing – you can’t be somewhere that doesn’t have a good connection, Wi-Fi or someplace like that. So that would be a concern.
Some Participants Preferred In-person Visits over HVV as It Felt More Reassuring and Personal
While all of the participants noted the benefits of HVVs, many of the participants still preferred to return to the hospital to have a traditional, in-person visit. One participant described feeling more reassured being in the hospital setting:
Interviewer: So, in other words, if your daughter didn’t have one of those things [iPad], you wouldn’t have been able to conduct… [an HVV]? Participant: Oh, no. I would’ve probably found some satisfaction of going back to the hospital to have the visit because hospitals, you feel they know what they’re doing. Just because the hospital gives you that secure feeling. You think they know what they’re talking about.
In comparison to an in-person visit, one participant felt that HVVs were less intimate as the length of the appointment was shorter, and there were less pleasantry exchanges, which the patient valued.
It [HVV] was less personal, you know? It was a little more distant. I felt I had less time to talk to him. Less time to have a conversation. And the other thing is if there had been some issue that had developed, uh, physically and it would’ve been nice to have been there to say, “Oh, Dr. [name of stroke doctor], by the way, you know, I have some discomfort in this arm.” You know what I mean? The physical examination is not there.
Discussion
In Canada, the annual healthcare expenditure and the proportion of seniors are projected to increase in the next two decades, meaning there will be mounting pressure on the healthcare system to meet the specific needs related to the senior populations. 14 Seniors (aged 65+) comprise a significant proportion of the growing number of Canadians with chronic health conditions. 15 It can be anticipated that issues around healthcare accessibility, availability, and acceptability will be at the forefront of public and health policy discussions and innovations. This is a particularly relevant question given the rapid uptake of virtual care to meet healthcare challenges during the COVID-19 pandemic and to prevent exposure to vulnerable populations, such as senior stroke patients. As a result, there is a need to consider the broader implications of virtual care and the ways it has been positioned to address ongoing and impending challenges in healthcare delivery.
Current literature on telemedicine modalities has given insight into the time-saving and accessible nature of telemedicine. Russo, McCool & Davies’ research in the US Department of Veterans Affairs found that telemedicine visits resulted in an average travel savings of 145 miles and 142 min per visit, leading to an average travel payment savings of 18,555 USD per year. Reference Russo, McCool and Davies16 Hatcher-Martin, Anderson, and Factor’s study of teleneurology showed that patients saved 2 hours of travel time on an average per visit. Reference Hatcher-Martin, Andrersen and Factor17 Powell et al.’s qualitative study of patient perceptions of telehealth video visits suggested that reduced costs and the ability to stay at home for those with physical limitations were identified as important components of the video visits. Reference Powell, Henstenburg, Cooper, Hollander and Rising18
Our interviews indicate that HVVs are perceived to be a mode of healthcare that is time-saving, convenient, and an accessible form of medical visit. The results show that HVVs were valued because of their ability to deliver punctual healthcare in the comfort of the patients’ homes, saving particularly those with physical impairment or mobility limitation a trip to the hospital. HVVs were also noted to be time-saving and convenient for all parties involved in a medical visit, such as physicians, hospital staff, and administration. This finding is also consistent with Appireddy et al.’s quantitative study on stroke patients in Kingston, Ontario, which found that the overall time saved by patients per eVisit was 80 minutes, 44 (21–69) minutes of which was travel time, and the travel distance avoided by the patients was 30.1 km. Reference Appireddy, Khan and Leaver2 Further, almost all of the respondents agreed that the eVisits saved them time, money, and avoided traveling to the doctor’s office. In other words, HVV offered a viable option for those who noted that geography, transportation, and intense weather conditions might pose as barriers to healthcare.
However, our study also found that there are some less desirable components of HVVs. Some participants had difficulty using or felt uncomfortable using technology to conduct a medical visit. This is consistent with Kruse et al.’s systematic review noting that lack of technological literacy, lack of high-speed Internet, and issues with application design presented some of the main barriers to the widescale adoption of telemedicine. Reference Kruse, Karem, Shifflett, Vegi, Ravi and Brooks19 Powell et al.’s qualitative study on video visits also identified that some participants had difficulty connecting to the eVisit platform. Reference Powell, Henstenburg, Cooper, Hollander and Rising18
Participants also supported a positive view of traditional forms of in-person visits despite the costs and inconveniences that they may incur. Participants expressed feeling more reassured simply by being present within the hospital setting and having more time to exchange pleasantries or conversation with the physician. Participants expressed that they did not mind the hassle of going to the hospital because their caregiver often drove them or set appointments up for them. Similarly, in Call et al.’s study of attitudes toward telemedicine, they found that 43% of survey participants (n = 3512) were averse to telemedicine despite the advantages of reduced travel and increased convenience. Reference Call, Erickson and Dailey20
There are three takeaways from this study. First, physical accessibility, economic status, and geography are significant determinants that influence healthcare access to in-person visits. Our study reveals that patients are often required to contend with various financial, physical, and geographical costs and barriers in order to attend in-person visits. Such demands may privilege those with social and economic capital, such as a caregiver or those with available cash to pay for transportation costs, and disproportionately disadvantage others who must lose income or time to attend their visits. As patients can receive care in the comfort of their home through HVVs, virtual care makes healthcare more equitable as it eliminates the physical and economic demands of in-person visits.
However, second, HVVs could also serve to exacerbate existing or create new determinants of health inequity. While geographical barriers are addressed by virtual care solutions, virtual healthcare can be inaccessible to those who lack technological literacy and ownership of technology – two barriers common amongst the elderly population. Virtual care may disadvantage those who do not have the financial means to obtain the proper technology needed to conduct HVVs. Individuals who do not know how to use their devices or do not have a caregiver to set up a device may also feel disinclined or discouraged from reaching out to their healthcare provider virtually with some of them opting to go to the hospital despite geographical barriers. As a result, virtual care can serve to exacerbate the barriers already faced by the senior population.
Third, our study shows that senior patients value medical visits as a relationship-building practice between patients and physicians. While the cost and time-efficient nature of virtual care was confirmed by all participants, many individuals expressed their willingness to conduct an in-person visit because they valued the interaction shared with their doctor. Virtual care may serve to shift the nature of the relationship between patients and physicians which may make it more uncomfortable to those senior patients already struggling to set up the technological aspects of their visit. Physicians seeking to use virtual care for prevention and management should take into account the differing needs and goals of each patient. Reference Blacquiere, Gubitz and Yu21
The results of the study were limited by the specific populations from which the participants belonged. As the sample generally reflected the stroke and senior population, the values and perceptions of the usability of HVVs may differ substantially from other populations. Consideration should also be given to the fact that, overall, the technological literacy of the group was low as all participants were from the senior population, meaning that the uptake of HVV may be different in other populations.
While this study gives a cursory glance at the possible intersections that come into play between stroke, aging, and digital health technologies, more studies should be conducted on the ways digital health may be conducive to or impact individuals and their social intersections given that the daily lives and health outcomes of stroke patients are dependent on the various social determinants such as age, housing, education, disability, employment, and geography. Other studies should be done to explore the impact of virtual care on senior stroke patients during and after the COVID-19 pandemic to better understand its usefulness in meeting health challenges specific to vulnerable populations. Further, given that some of our participants relied heavily on their caretakers within their in-person and virtual follow-up routines, future qualitative studies should examine how HVVs may impact the roles and routines of caregivers in comparison to preparations related to a traditional visit.
Conclusion
As healthcare challenges continue to rise in Canada and due to the COVID-19 pandemic, healthcare innovations should be at the forefront of ongoing academic and policy considerations. This study sought to explore the determinants, values, and experiences of stroke patients with HVV in an effort to fill a gap in the academic literature about patient-user experiences with HVV and to foster broader conversations on the social determinants of care. While the uptake of HVVs appears to be heavily dependent on personal preferences to healthcare as well as access or familiarity with technology, HVV shows promise as a form of healthcare that is time-efficient and accessible. HVV provides an option for patients struggling with physical mobility issues or adverse weather conditions to receive healthcare in the comfort of their own homes. This may mean that HVV may be helpful for other patients with chronic health conditions. As virtual care modalities will be at the forefront of mainstream healthcare in and following COVID-19, a greater examination of the ways digital health technologies intersect with the determinants of each patient should also be considered.
Acknowledgements
The authors would like to extend their thanks to all the participants for providing their insightful experiences and time for this study. The authors would also like to thank Mustafa Karacam for assisting with data analysis and coding.
Conflict of Interest
Dr. Appireddy reports grants from CIHR; PSI Foundation, Ontario; Department of Medicine, Queen’s University; Canada Health Infoway; SEAMO; and KGHRI during the conduct of the study. The remaining authors have no conflicts of interest to declare.
Statement of Authorship
SC: Conception, co-creation of data collection tool, interviewing, data analysis, and article writing. AOR: Co-creation of data collection tool, interviewing, and critical review of the manuscript. RA: Conception and critical review of the manuscript.



