Herpes zoster ophthalmicus (HZO) is defined as herpes zoster involvement of the ophthalmic division of the fifth cranial nerve.Reference Liesegang1 Patients often present with pain, rash, and infrequently ophthalmoplegia. The ophthalmoplegia usually starts about 5 to 7 days after the appearance of the vesicular eruption.2 The most commonly involved cranial nerve is the third, followed by the sixth then the fourth.Reference Park, Yoon, Yoon and Rhee3 Nerve involvement can be partial or complete, and multiple ocular motor nerve involvement can occur infrequently. The ophthalmoplegia can be bilateral, or less frequently, contra-lateral to the side of the rash.Reference Marsh, Dulley and Kelly4 A few cases describing this infrequent finding have been published in the literature up to date, in a pediatricReference Liao, Chu and Hutnik5 and a senior adult patients.Reference Jude and Chakraborty6 The pupil can be affected in isolation (internal ophthalmoplegia) due to dysfunction of the ciliary ganglion.Reference Edgerton7 Clinically, lesions on the tip of the nose resulted from nasociliary branch involvement have been described as Hutchinson’s sign which is a predictor for ocular inflammation and corneal denervation.Reference Zaal, Volker-Dieben and D’Amaro8 Here, we describe a case of HZO that developed unilateral abducens nerve palsy a few days after the onset of the rash.
The proband is a 69-year-old immunocompetent female patient, known for well-controlled hypothyroidism and dyslipidemia. Her past surgical history is significant for sleeve gastrectomy in 2016 and glaucoma and cataract surgeries in 2015. Her list of medications included atorvastatine, levothyroxine, and (dorzalanidine/timolol) eyedrops. She is nonsmoker and has no history of alcohol or drug abuse.
The patient presented to the emergency room with painful red vesicular facial rash in the left V1, and to a lesser extent, V2 distribution of 2-day duration. She was diagnosed clinically with HZO and discharged on oral acyclovir, pregabaline, and celecoxib. Two days later, she woke up with horizontal binocular diplopia. This was more prominent on left gaze and did not fluctuate. She had no headache, dizziness, and sensory or motor symptoms anywhere else. Her varicella zoster virus rash was fading and less painful.
On examination, the patient had medial deviation of the left eye on primary gaze. There was a limitation of left eye abduction resulting in horizontal diplopia, maximal on left gaze. Other extraocular movements were intact. She had normal visual field testing. Pupils were equal and reactive to light. There was a red crusted vesicular rash in the left V1 distribution extending to involve the tip of the nose with normal facial sensation (Figure 1). The rest of the neurological examination was unremarkable.
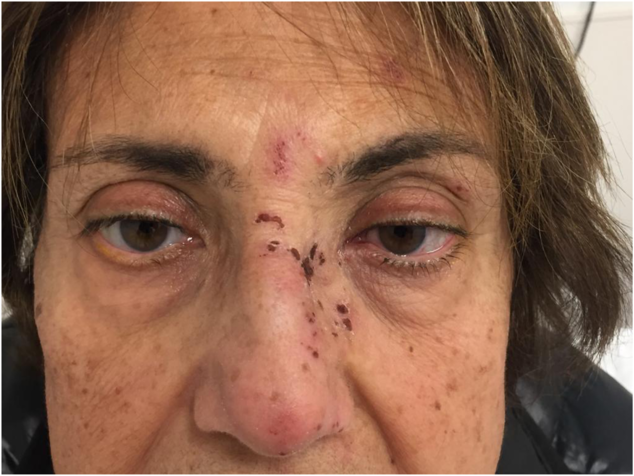
Figure 1: Crusted macules scalloped borders along the ophthalmic division (V1) of the trigeminal nerve with medial deviation of the left eye. Note the tip of nose involvement corresponds to positive Hutchinson’s sign.
Her basic laboratory results were within normal ranges except for slightly elevated sedimentation rate of 24.
Computed tomography of head and the orbit did not show any abnormalities.
Patient was prescribed Prednisone 60 mg orally, to be tapered at a rate of 10 mg every 2 days for a total of 12 days, while continuing her 21-day course of acyclovir. She had an outpatient magnetic resonance imaging head and skull base with contrast done 2 weeks later which did not identify any abnormality along the sixth cranial nerve course with no abnormal enhancement. In follow-up, her symptoms, the rash, and the diplopia were completely resolved within 2 weeks of emergency room visit.
Acknowledgments
The authors thank the anonymous reviewers for their useful suggestions.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Statement of Authorship
KA, a neurology resident, saw and managed the case in emergency department and wrote most of the case. AJ, a dermatology resident, described the dermatological lesion and contributed in writing the manuscript and submitting the documents. RM, a neurology staff, supervised the case management in emergency and reviewed the final manuscript prior to submission.



