Introduction
An estimated 69 million individuals experience a traumatic brain injury (TBI) worldwide each year.Reference Dewan, Rattani and Gupta 1 The vast majority of these injuries are mild in severity (mTBI) and thus distinguishable from more clinically significant head injuries (i.e., moderate-to-severe TBI). Relative to the general population, athletes are at heightened risk of experiencing mTBI, also known as concussion. A multitude of research examining the sequelae of athletic concussion has drawn increased public awareness and identified numerous signs and symptoms, including dizziness, headache, nausea, and vestibular dysfunction.Reference Laker 2–Reference Shirazi, Cusimano, Di Michele and McFaull 4 While most athletes recover from concussion within 2–4 weeks, as many as 33% of individuals continue to experience cognitive and/or behavioral symptoms even 1–3 months post-injury.Reference Willer and Leddy 5, Reference Rimel, Giordani, Barth, Boll and Jane6 Athletes who are symptomatic, continue to practice or compete and experience a subsequent blow to the head are at increased risk for second impact syndrome, which may have severe consequences (e.g., brain swelling, death).Reference McCrory and Berkovic 7 – Reference Scramstad, Ellis and Del Bigio 9 As a result, it is recommended that athletes who are suspected as having experienced a concussion be removed immediately from participation.Reference McCrory, Meeuwisse and Johnston 10 , Reference Giza, Kutcher and Ashwal 11 This approach is consistent with the “best practices” put forward by the National Collegiate Athletic Association (NCAA), which indicates that athletes’ education and recognition of concussion symptoms are central to adequate concussion management.
Extant literature regarding knowledge among those involved in athletics about the signs and symptoms of concussion has largely emphasized coaches, athletic trainers, and parents of athletes.Reference McLeod, Schwartz and Bay 12 – Reference Hunt, Michalak and Johnston 15 High school athletes have also recently been the focus of many concussion knowledge and symptom-reporting studies.Reference Hunt, Michalak and Johnston 15 – Reference Eagles, Bradbury-Squires, Powell, Murphy, Campbell and Maroun 20 This work has highlighted that underreporting of concussion may be attributed partially to poor recognition of concussion-related symptoms, a desire not to be removed from play following injury, and negative attitudes toward reporting symptoms (e.g., not recognizing the seriousness of concussion symptoms, being embarrassed about reporting symptoms).Reference Register-Mihalik, Guskiewicz, McLeod, Linnan, Mueller and Marshall 17 , Reference McCrea, Hammeke, Olsen, Leo and Guskiewicz 21
In contrast to the literature as it relates to high school samples, relatively little work has explored these topics among college student-athletes. This is surprising given that rates of concussion are higher in college than high school athletes.Reference Gessel, Fields, Collins, Dick and Comstock 22 One of the earliest college athlete concussion knowledge studies found that half of athletes indicated having no knowledge of the possible consequences of concussion, despite nearly one third of respondents self-reporting at least one prior blow to the head which caused dizziness.Reference Kaut, DePompei, Kerr and Congeni 23 While evidence suggests that college student-athletes’ understanding of the symptoms and consequences of concussion has improved in recent years, as many as one in four college student-athletes still experience a concussion without recognizing it.Reference Llewellyn, Burdette, Joyner and Buckley 24 This may partially be due to college athletes’ incomplete understanding of the full range of symptoms that can follow concussion (e.g., emotional symptoms) as well as false beliefs about the severity of a single concussion on cognitive abilities (e.g., 70% of athletes report that forgetting the names or faces of familiar individuals is a common sign of concussion).Reference Fedor and Gunstad 25 In at least one study of college student-athletes, concussion knowledge was directly shown to predict attitudes about reporting concussions in the future.Reference Kroshus, Baugh, Daneshvar, Nowinski and Cantu 26 Within this limited literature, knowledge has been linked to sex, years in school, and sport played.Reference Kroshus, Baugh, Daneshvar, Nowinski and Cantu 26 , Reference Kroshus, Garnett, Hawrilenko, Baugh and Calzo 27
Preliminary work has also explored the impact of prior concussion educational experiences on student-athletes’ knowledge and attitudes regarding concussion, although this work has largely been limited to high school samples. Bramley et al. noted that athletes who receive concussion education report being more likely to notify their coach if they experience symptoms of concussion.Reference Bramley, Patrick, Lehman and Silvis 28 However, after controlling for demographics (e.g., sport, sex), Kurowski et al. failed to identify a relationship between previous education and concussion-related knowledge.Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 In the only intervention study conducted in a collegiate sample to-date, Miyashita et al. found that an educational lecture intervention conducted prior to the beginning of the athletic season resulted in increased post-season concussion knowledge in a sample of Division II men’s and women’s soccer and basketball players.Reference Miyashita, Timpson, Frye and Gloeckner 29
Researchers have developed a greater appreciation for the full range of signs and symptoms that may follow concussion, and the NCAA has made it a priority to educate student-athletes about these signs and symptoms in order to promote safety.Reference Baugh, Kroshus, Bourlas and Perry 30 However, several gaps in the literature are in need of addressing in order to further improve efforts to improve student-athletes knowledge and symptom-reporting behaviors. Firstly, previous studies exploring collegiate student-athletes’ concussion knowledge have primarily explored a limited set of symptoms (e.g., headache, fatigue). Given the heterogeneity of symptoms that athletes may experience following concussion (e.g., impaired sleep, emotional changes), an examination of athletes’ knowledge regarding a larger set of symptoms is warranted. Previous studies have also explored a limited set of demographic predictor variables, and rarely assess knowledge differences across sports. Addressing this topic in a large sample of athletes that span different sports, ages, and other variables will allow for future educational efforts to be tailored to individuals who have demonstrated a lower amount of knowledge with regard to various aspects of concussion. Finally, prior studies regarding concussion knowledge have largely been descriptive by design, and do not attempt to explicitly increase student-athletes’ knowledge. Preliminary educational intervention work in a collegiate sample has been limited to only two sports (i.e., soccer and basketball) and did not assess changes in attitudes or concussion-reporting behaviors.Reference Miyashita, Timpson, Frye and Gloeckner 29 As such, further work exploring the effects of an intervention on collegiate student-athletes’ knowledge and attitudes toward concussion symptoms reporting appears necessary. The present study aimed to elucidate student-athletes’ concussion-related knowledge and attitudes toward symptom-reporting, explore demographic predictors of knowledge and attitudes, and determine whether responses to the survey changed following an online educational intervention.
Methods
Design
In this follow-up study, all participants completed three measures: a baseline questionnaire, a brief knowledge intervention, and a follow-up questionnaire. All three measures were administered using Qualtrics software (www.qualtrics.com). The baseline and follow-up questionnaires were identical in content and format. They were designed to take approximately 10–15 min each to complete. The intervention was administered 1 to 2 days following the baseline questionnaire and took approximately 10 min to complete. The follow-up questionnaire was administered approximately 1 week following the intervention. At the beginning of completing any of the three study measures, participants provided their unique student identification number. This number was used to link all measures to a participant prior to analyses. Participants were informed at the time of study enrollment that their identification number would solely be used to link their data across the three measures and their responses would be confidential. Participants completed a computerized, institutional review board-approved consent form prior to completing any questionnaires.
Participants
Participants were collegiate varsity student-athletes recruited from a large, Division I university in the southeastern United States. Participants were recruited during the Spring 2018 semester. All participants were required to be at least 18 years of age in order to participate. Participants of all different amounts of collegiate varsity experience (i.e., varying number of years on the team’s roster) were invited to participate (see Table 1). Nearly all varsity sports teams at the university were represented in the sample, including contact/limited contact (e.g., football, basketball) and non-contact sports (e.g., swimming and diving, cross-country). Participants were initially recruited via an email sent from their team’s lead athletic trainer, which included a hyperlink to the baseline questionnaire. The athletic trainer sent similar emails with hyperlinks to the intervention and follow-up questionnaires at appropriate intervals.
Table 1: Demographic variables
Measures
Concussion Questionnaire
A questionnaire was developed to assess knowledge about concussion and concussion-related attitudes and reporting behaviors. The questionnaire was derived from the one administered by Kurowski et al. to a sample of high school athletes, which included items administered by the Center of Diseases Control (CDC) heads-up program as well as a questionnaire used in Arizona to assess concussion knowledge of high school athletes.Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 The questionnaire also included information regarding demographics, previous concussion-related education, and concussion history (i.e., a computerized adaptation of the Ohio State University Traumatic Brain Injury Identification Method (OSU TBI-ID)).Reference Corrigan and Bogner 31
The questionnaire included 73 items and was comprised of 2 content sections: (1) concussion knowledge, and (2) concussion reporting attitudes/behaviors. Consistent with the Kurowski survey, the concussion knowledge section included two subsections: (1) signs and symptoms of concussion, and (2) typical course of recovery and accepted concussion management practices (see Table 2).Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 Items in the former subsection were formatted as a checklist, while items in the latter subsection were formatted as true/false questions. A total of 18 items were added to the signs and symptoms subsection in order to better reflect the full range of symptoms that college student-athletes may experience after concussion, and a total of 20 items were added to the recovery and concussion management subsection to evaluate a wider array of knowledge about recovery. A Seven-item concussion terminology section was also added to the knowledge section in order to evaluate participants’ familiarity with words that are medically equivalent to the term “concussion.” The 11-item concussion-reporting attitudes/behaviors section consisted of statements that participants answered using a three-point Likert scale with choices of “never,” “sometimes,” or “always” (see Table 3).
Table 2: Baseline knowledge questions
* Item not included in the Kurowski et al. (2014) questionnaire
Table 3: Baseline behavior and attitudes questions
Three validity check items were embedded throughout each of the questionnaires to ensure adequate effort (e.g., “If you are reading this, select ‘Always’”). Individuals who chose the wrong selection on any of the validity items at baseline were excluded from baseline analyses (see below). Individuals who chose the wrong selection on any validity items at baseline or follow-up or who did not complete all three components of the study (i.e., baseline questionnaire, follow-up questionnaire, or intervention) were excluded from intervention-related analyses.
Intervention
The concussion intervention consisted of a brief written presentation administered via Qualtrics (qualtrics.com) that participants read on their electronic device. The intervention was designed to match the content assessed in the baseline and follow-up questionnaires. Topics addressed in the intervention included, in order of appearance: (1) a medical definition of concussion (2) terms that are (e.g., mild traumatic brain injury) and are not (e.g., moderate-to-severe traumatic brain injury) equivalent to “concussion” (3) signs and symptoms that are (e.g., slower reaction time) and are not (e.g., decreased ability to read and write) typically experienced after concussion (4) actions that should be taken if a concussion is suspected (e.g., symptom-reporting immediately after experiencing symptoms and the importance of receiving an evaluation by a physician), and (5) how concussion is treated (e.g., time off from mental exertion, abstinence from alcohol, gradual return-to-play).
In total, the presentation included seven slides: one slide for an introduction to the intervention component of the study, one slide each for the five topics described previously, and one slide thanking the participant for completing this component of the study. The intervention included solely text (i.e., no pictures, videos, or other media was used).
Statistical Analyses
To explore common areas of misconception about concussion at baseline, descriptive statistics were used to examine accuracy in concussion-related knowledge broadly (i.e., percent correct across the full knowledge section), as well as accuracy within the three knowledge subsections (i.e., concussion terminology, signs and symptoms of concussion, typical course of recovery and accepted concussion management practices). Within the concussion symptoms portion of the knowledge section, descriptive statistics were used to determine which symptoms were most and least recognized as being associated with concussion. Descriptive statistics were also used to evaluate the extent to which responses on the reporting attitudes/behaviors section matched best practices. Pearson correlation coefficients were used to examine associations between baseline scores on the concussion knowledge section and concurrent scores on the reporting attitudes/behaviors section.
Multivariate analysis of variance (MANOVA) was used to detect associations between categorical demographic variables (i.e., sex, race, contact vs. non-contact sport, underclassman vs. upperclassman year in school) and scores on the knowledge section and the reporting attitudes/behaviors section. Follow-up t-tests were used to assess differences for any comparisons that emerged significant in the MANOVA. Paired samples t-tests were used to examine changes subsequent to the intervention in scores on the knowledge and attitudes/behaviors sections, as well as specific knowledge portions.
Results
A flow chart depicting study recruitment may be found in Figure 1. A total of 188 participants completed the baseline questionnaire. Of these, 179 provided valid responses and were included in baseline analyses. Demographic information regarding participants whose data were included in baseline analyses may be found in Table 1. Of these participants, 133 completed the intervention. From this subset of participants, 103 participants completed the follow-up questionnaire. Of these participants, 96 provided valid responses and were included in intervention-related analyses. No demographic differences were found between participants included in all analyses and those not included in any analyses or solely included in baseline analyses, all p > 0.05. No differences on baseline measures were found between participants included in all analyses and those solely included in baseline analyses, all p > 0.05. Participants took an average of 14.2 min (SD = 2.4) to complete the baseline questionnaire, 5.0 min (SD = 4.5) to complete the intervention, and 11.3 min (SD = 3.4) to complete the follow-up questionnaire. Cronbach’s alpha coefficients for individual subsections were adequate (0.73–0.91).
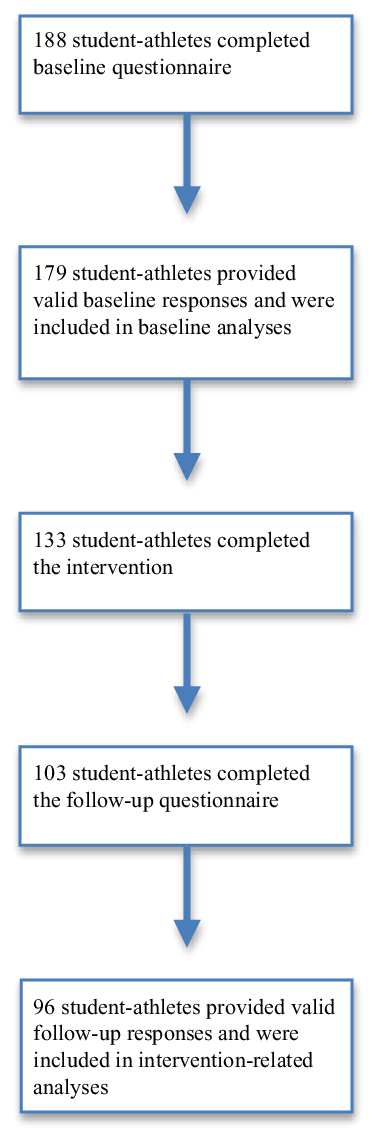
Figure 1: Sample recruitment.
Baseline Questionnaire Descriptive Statistics and Associations among Sections
Data regarding baseline performance on the questionnaire may be found in Table 2. Overall, the average percent correct on the knowledge section of the questionnaire was 72%. Average percent correct on the concussion terminology subsection was 60%. Among items within this subsection, participants most frequently correctly identified concussion as being a head injury followed by either brief loss of consciousness, dizziness, or amnesia (81.6% correct response rate). Items that were less likely to be correctly responded to included indicating that moderate-to-severe traumatic brain injury is not equivalent to concussion (36.3%).
The average percent correct on the signs and symptoms of concussion subsection was 73%. Participants most frequently correctly identified headache (96.1% correct response rate), sensitivity to light or noise (93.9%), and difficulty with balance or feeling dizzy (89.9%) as being associated with possible concussion. They least frequently correctly identified neck pain (39.7%) and trouble remembering important life events from their past (41.3%) as not being associated with concussion. Participants also less frequently correctly identified feeling sad, blue or having a loss of interest in normal activities (44.5%), feeling anxious or having difficulty relaxing (46.9%), and feeling irritable or easily angered (50.3%) as possibly being associated with a concussion.
The average percent correct on the recovery and concussion management subsection was 75%. Participants most frequently correctly responded “false” to “A little brain damage does not matter, as people use a small portion of their brains anyway” (98.3% correct response rate), “false” to “A concussion is harmless and never results in long-term problems or brain damage” (98.3%), and “false” to “In sport, concussion almost never happens” (97.8%). They least frequently correctly responded “false” to “If an athlete suffers a concussion, it is important to keep them awake” (19.0%) and “false” to “Majority of symptoms last for at least one month” (39.3%).
Data regarding baseline responses to behaviors/attitudes questions may be found in Table 3. In total, on average, 58% of responses on the reporting attitudes/behaviors sections matched clinical best practices. Responses that were most frequently consistent with best practices included responding “never” to “I feel that getting a concussion is not a big deal and actually proves that I am tough (89.9% of responses consistent with best practices),” responding “never” to “It is OK for an athlete to continue playing in a game in which they have suffered a concussion” (80.4%), and “always” to “I feel that it is important to be thoroughly evaluated by a medical personnel after an injury to make sure I recover completely” (75.0%). Responses that were least frequently consistent with best practices included responding “never” to “I would play through any condition or injury for our team to win” (11.2%) and responding “never” to “I would continue playing a sport while having a headache that resulted from a minor bump to the head” (16.3%).
Pearson correlation coefficients revealed that symptom scores were associated with recovery and concussion management subsection scores, r(169) = .30, p < 0.01, and with terminology subsection scores, r(169) = .23, p < 0.001. Recovery and concussion management subsection scores were not associated with terminology subsection scores, p > 0.05. Neither scores on the knowledge section nor scores on knowledge subsections were associated with reporting attitudes/behaviors section scores, all p > 0.05.
Associations between Baseline Questionnaire Scores and Demographic Variables
A one-way MANOVA revealed significant effects of sex (Pillai’s Trace = 0.09, F(4, 152) = 3.77, p < 0.01) and race (Pillai’s Trace = .12, F(4, 152) = 5.39, p < 0.001) on questionnaire sections. Follow-up t-tests revealed that relative to females (m = 44.83, SD = 4.39), males (m = 42.74, SD = 6.05) performed more poorly on the knowledge section, t(169) = –2.55, p < 0.05. Relative to females (m = 19.24, SD = 3.09), males (m = 18.14, SD = 3.33) also performed more poorly on the symptoms subsection, t(169) = –2.16, p < 0.05. Compared to Caucasians (m = 44.88, SD = 4.90), non-Caucasians (m = 42.05, SD = 4.93) performed more poorly on the knowledge section, t(169) = 3.25, p < 0.01. Relative to Caucasians (m = 19.46, SD = 2.99), non-Caucasians (m = 17.28, SD = 3.24) also performed more poorly on the symptoms subsection, t(169) = 4.16, p < 0.001. No effects were found for contact sport or year in school on questionnaire section scores, both p > 0.05.
Changes in Knowledge and Attitudes from Baseline to Post-Intervention
Paired-samples t-tests revealed a modest but significant increase in knowledge regarding concussion terminology from baseline (m = 4.33, SD = 1.34) to post-intervention (m = 5.16, SD = 1.11), t(95) = 5.14, p < 0.001. No significant changes were found for other knowledge sections or the attitudes/behaviors section, all p > 0.05.
Discussion
Efforts to evaluate athletes’ knowledge about concussion have increased substantially in recent years.Reference Hunt, Michalak and Johnston 15 – Reference Eagles, Bradbury-Squires, Powell, Murphy, Campbell and Maroun 20 This work has important implications for educational interventions, such as identifying specific student-athlete sub-groups who may be in need of greater attention by educators and particular gaps in student-athletes’ knowledge more broadly that should be focused on via educational efforts.Reference Kroshus, Baugh, Daneshvar, Nowinski and Cantu 26 , Reference Kroshus, Garnett, Hawrilenko, Baugh and Calzo 27
Prior studies indicate that both high school and collegiate student-athletes demonstrate considerable knowledge about the symptoms and effects of concussion.Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 , Reference Miyashita, Timpson, Frye and Gloeckner 29 However, direct comparisons between these groups have historically been difficult given the use of differing questionnaires. At baseline, student-athletes in the present study correctly answered 72% of all content included in the knowledge section of the survey. This proportion is similar to that of Kurowski et al., whose sample of high school athletes correctly answered 68% of a similar survey.
At baseline, among the three knowledge subsections, participants obtained the highest scores on the recovery and concussion management subsection (75%) followed closely by the symptom subsection (73%), while scores on the terminology subsection (60%) were somewhat lower. These results may hint at the significant emphasis that NCAA education programs place on the former two domains, and indicate that student-athletes are generally familiar with symptoms of concussion, as well as what to expect over the course of recovery and how to manage symptoms post-injury. However, concussion terminology appears to be an area in need of greater attention. In particular, student-athletes appeared to have difficulty differentiating moderate or severe TBI from more mild injuries. At baseline, less than 40% of participants accurately indicated that moderate-to-severe TBI is not equivalent to concussion. In comparison to concussion, moderate-to-severe TBI is relatively rare in sports and is associated with significantly greater implications for individuals’ cognitive and functional abilities.Reference Jordan 32 As such, educational efforts should more clearly articulate that concussion represents solely one portion of the clinical spectrum of TBI. Doing so would likely help student-athletes become better informed about the symptoms they can expect and not expect to experience following injury.
Student-athletes displayed good recognition at baseline for many of the hallmark cognitive and somatic symptoms of concussion, including headache, difficulties concentrating, slowed reaction time, nausea, and sensitivity to light or noise. These symptoms were identified at a similar or higher rate than did high school athletes in a prior study,Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 suggesting that this trend holds true across young adulthood. Most student-athletes also acknowledged the high frequency of concussion in sport, the medical seriousness of experiencing brain damage, and the fact that a concussion may have effects on an individual without their realization or observable signs. However, consistent with the Kurowski high school sample, most student-athletes also erroneously believed that symptoms typically last for a month or more post-injury. Thus, educational efforts should better communicate the transient nature of most symptoms post-concussion.
Several of the symptoms that were least commonly correctly identified at baseline pertained to emotional symptoms, namely anxiousness, depressiveness, and irritability. Of all symptoms included in their survey, Kurowski et al. found that emotional symptoms broadly were the least frequently recognized symptom, with only 40% of high school athletes identifying it as characteristic of possible concussion.Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 The current study mirrors those results and suggests both that this misconception is true at the collegiate level and is not limited to solely one aspect of emotional functioning (e.g., anxiety), but rather extends across domains. Given the effects that concussion-associated emotional symptoms may have on other aspects of functioning (e.g., academic, social),Reference Rapoport, Mccullagh, Streiner and Feinstein 33 it is important that student-athletes are made aware of the normalcy of such symptoms post-injury, the generally transient nature of such symptoms, and the mental health resources available to them. Most student-athletes also incorrectly reported that difficulties recalling important life events were characteristic of concussion, which is similar to a finding from Fedor and Gunstad (2015) regarding names and faces of familiar individuals.Reference Fedor and Gunstad 25 These results provide further indication that discrimination between mild and more severe head injuries during educational programming is warranted.
At baseline, student-athletes’ responses on the reporting attitudes/behaviors section were consistent with clinical best practices as outlined by the NCAA in 58% of instances. Agreement between self-reported attitudes/behaviors and best practices were highest when a concussion had unquestionably been experienced (i.e., when the item explicitly noted the occurrence of a concussion) and lowest when the term “concussion” was not noted. As such, student-athletes may view hits to the head that result in more “mild” symptoms (e.g., headache) or for which the effects are somewhat ambiguous less seriously. Alternatively, student-athletes may believe that the need for a removal from play might vary on a case-to-case basis and is not their decision to make, as evidenced by many student-athletes responding that they “sometimes” would take steps to leave play under these circumstances. This would be consistent with best practices as put forth by the NCAA, which highlights the need for an athletic trainer or team physician to make the final removal from play determination. In order to remedy such cases, educational interventions should make clear that a removal from play to screen for signs of concussion does not by definition imply that a student-athlete will be diagnosed with said injury, and may still return to the game if symptoms aren’t detected.
Relative to females at baseline, male student-athletes performed more poorly on the symptom subsection as well as noted reporting attitudes/behaviors less consistent with best practices. High school male student-athletes have demonstrated lower knowledge and reporting attitudes/behaviors that are more incongruent with best practices,Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 , Reference Bagley, Daneshvar and Schanker 34 and the present study suggests that this difference holds true in college as well. Student-athletes of non-Caucasian race also fared more poorly on the knowledge section than did Caucasians, a relatively novel finding likely due to the limited literature on racial differences in post-concussion cognitive performance and outcomes more broadly.Reference Kontos, Elbin, Covassin and Larson 35 Although some have identified individuals with different ethnic and cultural ancestry (e.g., Indigenous Canadians) as having relatively limited knowledge regarding concussion,Reference Hunt, Michalak and Johnston 15 ours is among the first studies to directly compare Caucasians and non-Caucasians’ concussion-related knowledge and behaviors in a single study. Results of the present study suggest that males and non-Caucasians may be in particular need of receiving concussion-related education. However, it is important to note that racial and sex differences were modest in size, and all student-athletes irrespective of sex or race would likely benefit from education about concussion.
In comparison to their baselines, student-athletes demonstrated a modest increase in concussion terminology scores post-intervention. These results suggest that student-athletes became more familiar with terms that are and are not equivalent to “concussion” over this period. However, in contrast to a prior study,Reference Miyashita, Timpson, Frye and Gloeckner 29 knowledge about concussion did not improve following the intervention. Furthermore, despite increased knowledge regarding concussion terminology, student-athletes’ responses on the reporting attitudes/behaviors section did not change, and neither the knowledge section score nor the terminology, symptom, or recovery and concussion management subscores were associated with reporting attitudes/behaviors. These findings are consistent with past work utilizing a similar survey, which indicated that knowledge about concussion did not correlate with reporting attitudes/behaviors.Reference Kurowski, Pomerantz, Schaiper and Gittelman 18 As such, the creation of interventions that are specifically designed to alter student-athletes’ reporting attitudes and behaviors, rather than solely their knowledge about concussion, may be warranted.
Limitations
The present study was limited by its sample size; while the overall sample is comparable or larger than several prior studies in this area, it is also predominantly female and Caucasian. As such, sex and racial differences in performance on the survey may be the result of chance findings rather than true contrasts. A control group (i.e., student-athletes who did not complete the educational intervention) was not recruited due to concerns about limited power, given the sample size. Future studies utilizing this educational intervention should either include a control group in order to compare post-intervention performance between participants who do and do not receive the educational component, or administer the baseline questionnaire twice prior to the intervention in order to determine the effect that simply answering questions regarding concussion has on knowledge and reporting behaviors.
Given that all participants were recruited from a single, southern university, it is possible that findings may differ at other institutions and in other regions, particularly since colleges and universities may differ in the concussion educational programs they provide. As such, further work that examines this topic in a multisite sample representative of the makeup of collegiate student-athletes nationally would be beneficial. Responses on the reporting attitudes/behaviors section were also self-reported, and thus may differ from how student-athletes would act in an actual game or practice setting. Additionally, as study measures were administered online and thus frequently completed without an athletic trainer or study administrator present, it is possible that some participants may have looked up answers to items.
Although an attempt was made to utilize a questionnaire that reflected the current consensus of concussion research, other investigators may have come to different conclusions about some items where there have been mixed findings. For example, whereas some have identified an increase in depressive symptoms following concussion,Reference Kontos, Covassin, Elbin and Parker 36 others suggest that the strongest predictor of these symptoms is baseline depression severity.Reference Yang, Peek-Asa, Covassin and Torner 37 Additionally, although the questionnaire itself was based on those used in prior studies, it also included items added by study investigators. These additions allowed for examination of a broader knowledge base, however also meant that a measure identical to ours has not been utilized in prior studies, thus limiting our ability to compare performance to other samples. Finally, post-intervention performance was measured at 1-week follow-up, an interval chosen due to logistical considerations (e.g., likelihood of losing some student-athletes to follow-up due to graduation or the conclusion of their athletic season). Future work that includes this intervention should employ a longer timeframe post-intervention in order to better assess the longer-term effects of the intervention.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
JPKB was involved in study design and recruitment as well as drafting, editing, and submission of the manuscript. MC was involved in study design and editing of the manuscript. SM was involved in study recruitment and editing of the manuscript.





