The recent joint statement published by the Canadian Association of Gerontology (CAG) and the Canadian Journal on Aging (CJA) (Meisner et al., Reference Meisner, Boscart, Gaudreau, Stolee, Ebert and Heyer2020) highlighted the potential and real impact of the pandemic on the aging population in Canada and beyond. Multiple and competing areas of concern for this population, from psychological health to long-term care, were profiled alongside the need for multidisciplinary and collaborative approaches to address a range of health and social issues in the wake of the global health emergency. For example, Middleton (Meisner et al., Reference Meisner, Boscart, Gaudreau, Stolee, Ebert and Heyer2020) warned how increases in sedentary behaviour among community-dwelling seniors resulting from ongoing public health restrictions put in place to deal with the COVID-19 pandemic could lead to adverse health outcomes, such as higher rates of cardiovascular disease. With such restrictions expected to be in place for the foreseeable future, investigating the effects of the pandemic and associated public health measures on our aging population is a growing concern.
Prior to the pandemic, our multidisciplinary team composed of national and international experts, alongside older adults and other stakeholders, including not-for-profits and industry, was poised to launch a large-scale cohort study of 2,000 community-dwelling older adults. Using the latest technology, the principal aim of this research was to identify precursors to early changes in mobility with aging. Unfortunately, our study came to a sudden and complete stop on March 24, 2020, when McMaster, similar to other Canadian universities, halted all human research with the exception of specially approved clinical and interventional trials (New Directives for McMaster Researchers, 2020). Although most research-intensive institutions have since eased restrictions, non-pandemic research involving face-to-face contact with older adults and other high-risk groups remains prohibited (Phased Increase of On-Campus Research Activity – Phase 2, 2020). Hence, our research team faces a number of ongoing challenges as to how we might conduct our intended study without endangering the health of our participants, staff, and the general public.
In these pandemic times, we expect many investigators involved in aging research to be facing similar challenges. As such, we see merit in sharing how our research team, even at this early stage, has pivoted our study platform to adhere to current public health policies while still maintaining the integrity of our original aims. While the pandemic highlights the importance of cross-disciplinary research to navigate the complexities of conducting large-scale studies, it has also exposed existing limitations in how we typically conduct in-person data collection for some older adults. For example, if an older adult has existing comorbidities that affect their cognition and/or mobility, being able to physically access a research site can be challenging. Participation in research can also increase caregiver burden. Studies should be designed to provide choice of in-person or remote data collection, where possible, as well as ensuring that an appropriate level of support is provided to caregivers, if needed. Early lessons from planning and conducting research involving older adults under the current circumstances will no doubt inform ongoing and future studies in developing innovative ways to support the participation of our aging population in research. Even with the development of a vaccine, the effects of the pandemic are likely to persist for years to come. Hence, the objectives of this article are two-fold: (1) to discuss considerations for conducting aging research during the COVID-19 pandemic that ensures that broader contextual elements, such as public health measures, are considered and, (2) to outline pragmatic strategies for studies involving older adults in the face of such measures. We have all been forever changed by COVID-19, including our participants and our research programs. The intention of this research note is to spark both discussion and debate about conducting aging research in the COVID-19 era and beyond.
Aging Research is Now, and Has Been Forever Changed, by the COVID-19 Pandemic
Since the World Health Organization convened its first meeting in early February to set research priorities specific to COVID-19 (World Health Organization, 2020), many scientists quickly shifted their focus and corresponding research to combat this virus. Given this rapid shift, some have voiced concerns that the pandemic “…diverted the time and resources of investigators, funders, regulators and delivery teams away from non-COVID-19 research” (Richardson et al., Reference Richardson, Carroll, Close, Gordon, O’Brien and Quinn2020, p. 4). These concerns reflect a potentially contentious issue as to whether non-COVID-19 research should continue, or be curtailed, in light of the global health emergency. We contend that all aging research is now, and will continue to be, influenced by COVID-19. As such, best practices for involving older adults in studies during this (and future) times of major risk are warranted.
There are a number of issues with framing research as non-pandemic without considering the pervasive impact of COVID-19 across studies involving older adults. The potential dichotomization of studies as “pandemic” or “non-pandemic” could lead to unintended consequences whereby some investigators might assume that their area of study is somehow unaffected by current events. Although such dichotomization could prioritize important issues, such as limiting the spread of the virus as well as studying its acute impact, there is a possibility that the specific needs of our aging population may not be readily identified if their data are merged with others, or not considered at all.
As illustrated in Figure 1, we propose a continuum of pandemic research in which the research question and corresponding methodologies, analyses, and potential application of the results are situated in accordance with the stage of the pandemic. For example, if data collection for a study occurred just prior to COVID-19, then the potential application of the findings should be situated in the current context; that is, how might study results and conclusions be interpreted today in light of the current pandemic or public health restrictions? Similarly, even studies with older adults that are not directly focused on those diagnosed with COVID-19 need to consider how their research participants may be affected by the ongoing pandemic and associated public health restrictions. For example, the effects of reduced physical activity levels, increased anxiety, or limited access to and use of health care services, such as reduced frequency and characteristics of visits with health care providers, are all areas that could have methodological implications for recruitment and outcome measure selection. By using a continuum approach, we can avoid the dichotomization of aging research, as pandemic or non-pandemic in focus.

Figure 1. Aging research using a pandemic continuum. Components of the research process are impacted by the pandemic and, as such, should be situated accordingly. For example, if data collection for a study occurred just prior to COVID-19, then the potential application of the findings will need to be interpreted in accordance with current context in which consideration is given to the stage of the pandemic as well as to the public health restrictions in place.
Prior to the pandemic, there was also growing interest in developing best practices for engaging older adults in remote data collection using telecommunication approaches. However, such approaches can pose major ethical challenges for the aging population, as they often lack a user-centric design, and can neglect the complexities of obtaining consent remotely, as well as privacy and confidentiality (Magnusson & Hanson, Reference Magnusson and Hanson2003). Recent recommendations emphasize that older participants need to feel comfortable with the technology employed and be offered scaled levels of participation that are congruent with their diverse needs, as well as that there should be consideration for caregivers who often assist care recipients with remote engagement in research (Foley et al., Reference Foley, Welsh, Pantidi, Morrissey, Nappey and McCarthy2019). Such recommendations apply to any program of research going forward, not just those that are pandemic focused.
To a certain extent, the pandemic can be viewed as having a “period effect” (Blanchard, Bunker, & Wachs, Reference Blanchard, Bunker and Wachs1977; Rudolph & Zacher, Reference Rudolph and Zacher2020) such that large swaths of the population are living under the same public health restrictions. Although some may view this time period as an opportunity to investigate the impact of the pandemic on differential segments of the population, we must proceed with caution, particularly in studies involving older adults. Emerging evidence highlights the heterogeneity of the aging population and the importance of considering intra-individual differences, such as race and socio-economic status, which are known to influence health trajectories in later life (Lin & Kelley-Moore, Reference Lin and Kelley-Moore2017). Given this heterogeneity as well as the situational complexity imposed by the pandemic, the need for “cross-unit knowledge-sharing” (Hansen & von Oetinger, Reference Hansen and von Oetinger2001) is even more critical in aging research.
Our research team includes members from different disciplinary backgrounds. Although we have done our best to circumvent the challenges imposed by the pandemic on our planned cohort study, we know that there are researchers who have pivoted their studies using various strategies. We want to learn from these researchers. As a first step, our team has outlined proposed modifications to our study alongside pragmatic strategies that may be of benefit to others currently pivoting their aging research programs. By discussing the modifications enacted by our research team early in the process, our aim is to catalyze conversations among Canadian researchers and beyond through which we can learn from each other through a virtual consortium or network as we move forward in our respective and collective efforts to conduct research on aging in COVID-19 era.
Early Lessons from Pivoting our Mobility and Aging Cohort Study During the Pandemic
Efforts to develop a “big picture” understanding of mobility changes in older adulthood through large-scale investigations have been challenging (Satariano et al., Reference Satariano, Guralnik, Jackson, Marottoli, Phelan and Prohaska2012), in part because of the broad range of biological, behavioural, social, and environmental factors that can affect mobility in later life (Webber, Porter, & Menec, Reference Webber, Porter and Menec2010). Hence, our proposed cohort study involving 2,000 older Canadians was specifically designed to track not only their health and function but also to consider the different ways in which older people move in everyday life, from getting out of a chair to their use of various modes of transportation. As part of our original plan, a battery of performance-based and self-reported measures of mobility and health were to be administered at baseline and at annual follow-ups. In addition to these more traditional measures, our study also makes use of sophisticated wearable sensors designed to track a range of mobility parameters in daily life. As such, our “Monitoring My Mobility (M3)” cohort study aimed to be one of the largest and most comprehensive research platforms to identify early predictors of mobility limitations in later life.
As previously noted, our research team was forced to take a major step back in mid-March of 2020 when public health restrictions were put in place. In fact, everywhere we turned, it seemed that there was a litany of challenges that required our attention. However, a plan slowly began to emerge, which we attribute, in part, to three major strategies undertaken by our team to pivot our study platform. In the following sections, we elaborate on these strategies with the aim of opening a conversation with others embarking on applied aging research during the pandemic.
Leaning into Collaborations with Older Adults and Other Stakeholders to Address Current and Anticipated Research Challenges through Shared Brainstorming and Problem Solving
Our first step was to engage older adults in virtual and informal conversations that explored the impact of the pandemic on their daily lives. These early conversations with a convenience sample of older adults were instructive as to the varied ways in which pandemic-related restrictions were impacting their health and mobility. From these conversations, we chose to proceed with a longitudinal tele-survey as a viable means to investigate the impact of COVID-19 and associated public health measures on our intended sample of community-dwelling older adults; we also formally engaged an older adult as a partner in our project. This partner was purposely selected, as she had volunteered in previous studies with the lead author (B.V.) as both a research participant and a co-facilitator of focus groups with older peers. In addition to engaging a formal partner as a member of our research team, we also piloted our survey with a convenience sample of older adults and elicited their feedback. At the time of our consultation, our research partner was single, white, 81 years of age, living alone in an apartment, and was bilingual (Portuguese, English). She also had arthritis and an autoimmune disorder that made her more susceptible to the effects of COVID-19. When we shared our research aims and a draft of our survey with our older adult stakeholders, it was clear that our survey, on its own, would not have been adequate to capture personal accounts of everyday life under “quarantine”. Therefore, we made the decision to include follow-up interviews to further understand the lived experience of older Canadians with public health restrictions in place. By consulting a convenience sample of older adults, even informally, as well as having the formal guidance of our research partner during this challenging time, instrumental changes were made to our methodology.
In the CAG-CJA statement (Meisner et al., Reference Meisner, Boscart, Gaudreau, Stolee, Ebert and Heyer2020), van den Hoonaard emphasized the importance of qualitative research to explore the “social meanings” ascribed by older adults to their lived experiences during the pandemic (p. 337). Our team also recognizes the importance of involving older adults and caregivers in the design of health care research and that such involvement requires much forethought and planning. For example, McNeil et al. (Reference McNeil, Elliott, Huson, Ashbourne, Heckman and Walker2016) detail a five-stage approach (consider environmental context, plan, establish, build, transition) for partnering with older people in health-related research. Our research team had to pivot quickly to capture the impact of the different levels of public health measures on the mobility and participation of older adults living in the community. By initiating conversations with older adults at the earliest stages in pivoting our study, our team and our prospective participants benefitted from their insights. For example, preliminary analysis of our survey data suggests that many older adults have reduced their physical activity levels and participation in the community in response to social distancing measures. Given this finding, our team has adapted our cohort study protocol in terms of the frequency with which in-home and out-of-home mobility will be monitored. We have elected for longer monitoring periods (e.g., 10 days vs. 5 days) to capture less frequent bouts of community mobility during the pandemic. Ultimately, findings from both the survey and the interviews will provide important and timely insights regarding both personal and contextual determinants of the health, mobility, and participation of older Canadians during the COVID-19 crisis.
Seeking out Cross-Disciplinary Perspectives to Address the Actual and Potential Complexities of Undertaking Aging Research during the Pandemic
The joint CAG-CJA statement encourages interdisciplinary approaches to aging research, in part because of the “complex and multifaceted ways that COVID-19 is affecting older adults from individual to population levels” (p. 334). Given these complexities, our multidisciplinary research team composed of experts from diverse fields, which was assembled prior to the pandemic, may be considered serendipitous in light of the current circumstances. However, simply having different perspectives at the table does not necessarily mean that collaborations ensue and discoveries abound. Although the lead-in to a special issue of Nature on “interdisciplinarity” (Mind meld, 2015) warned “…research that transcends traditional academic boundaries is still unfashionable and poorly rewarded,” the pay-off of such collaboration, as outlined by those featured in this special issue, suggests otherwise. For example, Brown, Deletic, and Wong (Reference Brown, Deletic and Wong2015) described the process by which they catalyzed cross-disciplinary collaborations to establish their multinational research enterprise (i.e., urban water research centre). Interestingly, when viewing this process through the lens of the current pandemic, the basic principles outlined for catalyzing such collaborations still hold true. Table 1 outlines the congruence between these principles and the steps enacted by our interdisciplinary team in the face of the current pandemic.
Table 1. Reflections on catalyzing cross-disciplinary research prior to and during the pandemic
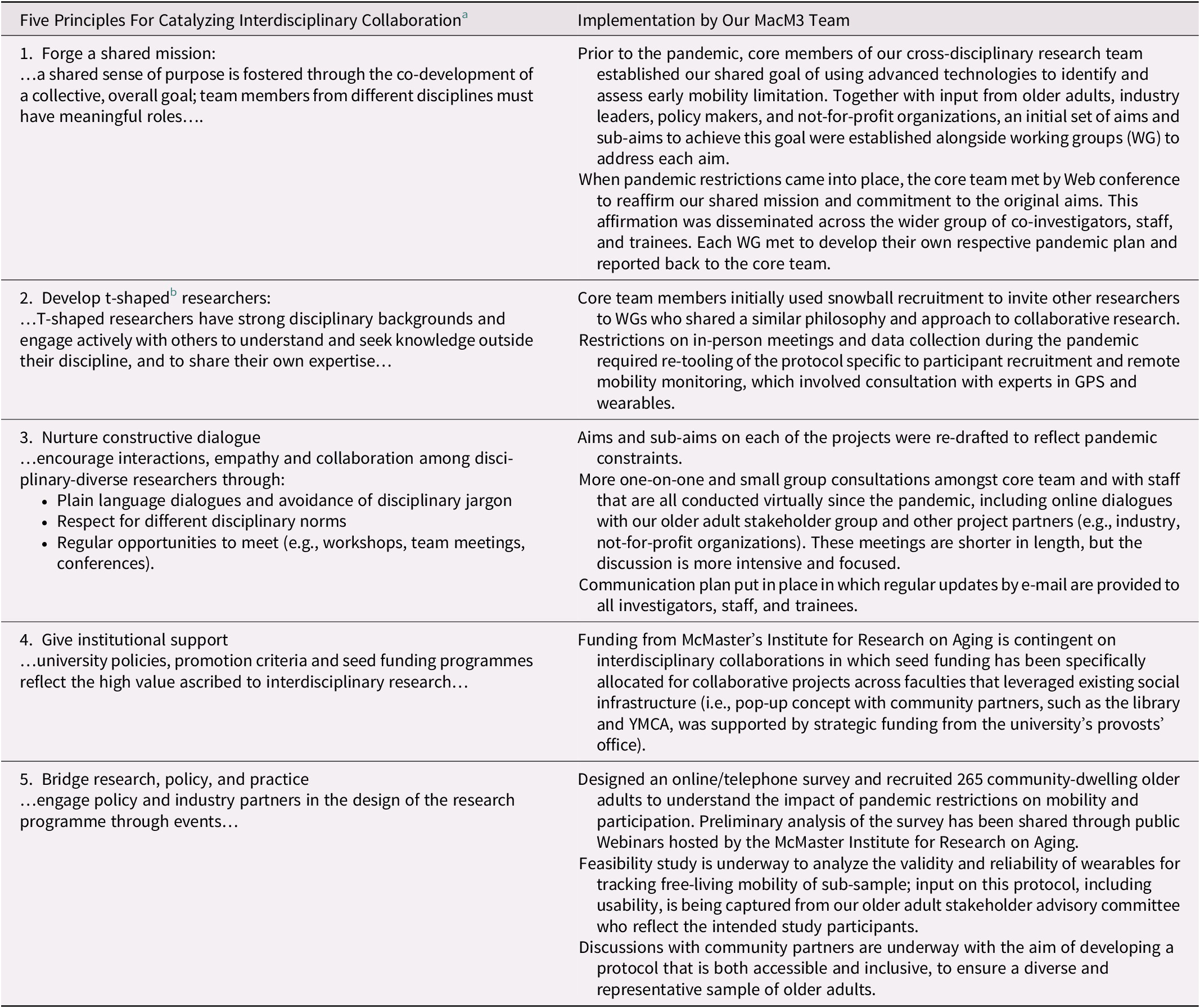
Note.
a Brown, Deletic, and Wong (Reference Brown, Deletic and Wong2015).
b Hansen and von Oetinger (Reference Hansen and von Oetinger2001).
When reflecting on the third principle in Table 1, “nurture constructive dialogue”, which focuses on encouraging empathy and collaboration by using inclusive language and avoiding disciplinary jargon, our team has found since the outset of the pandemic that we hold more one-on-one and small group consultations amongst the core team. Although these virtual meetings tend to be shorter, the agenda items are more action oriented, which encourages more collaborative decision making. For example, determining the wearable device by which the mobility of our participants will be monitored has proven to be a highly collaborative exercise. With input from engineering and geography (e.g., how to deliver, set up, and calibrate the wearable device for in- and out-of-home movement), and social science (e.g., acceptance and usability of wearable), as well as rehabilitation science (e.g., validation of measurement protocols and translational impact of findings to everyday function and health), pilot testing is underway. Regular updates on sub-projects, such as feasibility testing of the wearable device, are provided by e-mail to ensure that team members, staff, and trainees remain current on study progress.
Congruent with the fifth principle, “bridging research, policy, and practice”, our team has also sought innovative ways to ensure that our proposed cohort protocol remains relevant by launching a longitudinal tele-survey that captures the impact of the pandemic on he health and mobility of older adults under quarantine. Members of the core team were also invited to share preliminary results of this survey through a Webinar with community stakeholders. As well, we have sought strategic feedback on our proposed changes to our cohort protocol from leading aging researchers from diverse fields. For example, McMaster University’s Institute for Research on Aging (MIRA) offered a virtual opportunity to present these changes to its international scientific advisory panel. During this presentation, concerns about the potential association among social isolation, mental health, and the ensuing consequences on mobility were raised. As a result of this discussion, we have since added questions specific to mental health and distress from the pandemic to our data collection protocol for our cohort study. By seeking cross-disciplinary perspectives early and often in the study evaluation and redesign process, potential blind spots may be averted. However, if study protocols cannot be adapted per se, the benefits of ongoing dialogues with stakeholders are critical to recognizing possible limitations of the intended research, which ensures that analyses are contextualized in ways that are meaningful to research, policy, and practice going forward.
Transitioning Research Infrastructure to Remote Environments to Promote Participation of Older Adults in Research
Prior to the pandemic, our research team was considering innovative ways to recruit participants as well as to conduct primary data collection in the community. However, when the COVID-19 public health measures were put in place, our research team was forced to reconsider our methods of data collection, including our use of performance-based measures (PBMs). PBMs are important assessments of mobility “capability”, meaning such measures capture an individual’s actual abilities. Hence, many PBMs have been standardized for use in face-to-face settings. Although a few of these measures have been used in virtual settings, further validation is needed. In this way, the pandemic offers a unique opportunity to contribute to research on the emerging role of technology when conducting remote functional assessments for older adults. For example, researchers, such as Lai et al. (Reference Lai, Chiu, Pounds, Tracy, Mehta and Young2020), modified their protocol for a randomized controlled trial by substituting face-to-face assessments with a technology-enabled package of equipment and instructions that support the measurement of mobility among older adults from afar. Our team is adapting and evaluating the validity and reliability of standardized mobility tasks (e.g., 1-minute chair stand test) that aim to reduce risk of falls among unsupervised participants for remote administration. Initially, the pandemic restrictions limited our queries about mobility to certain “tenses” or circumstances (Glass, Reference Glass1998): “capacity” as measured through self-report (what participants can do) and “enacted” performance (what participants actually do) using wearables during everyday activities. By leveraging advancements in mobile technologies, our team has adapted our measures for remote assessment, which will allow us to describe mobility more fully by including “capability”: what participants could do.
During the process of adapting our measures and protocols, our team has concurrently considered how to enhance the accessibility and inclusiveness of our research. Promoting opportunities for older adults to participate in research is critical, particularly those from underserved and under-represented groups. Such groups can include, but are not limited to, women, Indigenous peoples (First Nations, Inuit, and Metis), persons with disabilities, racialized groups, members of 2SLGBTQ+ as well as those from rural and remote geographic locations. Intersectionality across these groups is also an important consideration in both study design and methods. Although improving access to technology is an example of how we might promote study participation thereby improving equity, it can also have the opposite effect whereby those who do not know how to use technology or do not have access to the necessary devices could feel stigmatized or excluded from our research.
In the Coin Model of Privilege and Critical Allyship, Nixon (Reference Nixon2019) highlights how existing approaches, including social structures, can perpetuate “unearned” advantages (top of coin) and disadvantages (bottom of coin) in health. The key, as Nixon emphasizes, is to target change at the “coin”, or social structures, that can produce and maintain inequality (e.g., sexism, ageism, ableism, racism). In terms of our study, equity is not enhanced in the provision or distribution of technology (and/or Internet access), rather it is by disrupting traditional ways of doing research that shift the power dynamic between researchers and participants. By involving older adults and other stakeholders with different lived experiences in the pivot of our platform, we have expanded our protocols to enhance the accessibility and inclusiveness of our research. A key outcome of this approach, is that we are delivering Internet-ready tablets with one-button access for our remote assessments, to help promote inclusion of older adults who may be unfamiliar with technology.
Through our consultations with older adults, our team has further developed our initial concept of creating “pop-up” research sites that leverage existing social infrastructure in both urban and rural areas. These prospective sites include libraries, seniors’ centres, sports complexes, places of worship, and other publicly available spaces. The term “pop-up” has become a popular catchphrase to describe shared spaces that are often temporary in nature. Prior to the pandemic, our intent was to have rotating pop-up sites where we could administer our mobility measures in-person as well as distribute wearables to participants in real time. Since the COVID-19 disruption, we have re-conceptualized these sites to be “virtual”, meaning the focus is on remote data collection, yet still leverages existing community partnerships. For example, our municipal public library has set up remote programming (Web-based and phone-in) specifically aimed at the aging population, including those living in more rural locations (Hamilton Public Library Events, 2020). Leveraging this infrastructure, potential participants will be recruited to attend “virtual” information sessions (phone/online) to learn more about the study. Our team would then work with participants to determine the optimal way to engage in the study by presenting different options, such as providing technology already wired to the Internet for at-home use or setting-up a private, “sanitized” space in the library where they could connect to study personnel through an online portal. We are also considering how we might be able to adapt our measures for administration over the phone. By considering different ways to engage older adults from diverse backgrounds and needs, our research team, including trainees, are learning about inclusive ways to involve study participants that can enhance equity. Initial validation of proof-of-concept, virtual pop-up sites with older adults living in urban locations is already underway. Such an approach also sets the stage for interventions targeting older adults, which is closely aligned with our vision for promoting healthy aging in the everyday spaces and places that people work, live, and play.
Conclusions, Reflections, and Future Considerations: Moving the Aging and Mobility Agenda Forward in the COVID-19 Era
Transitioning our prospective cohort platform to an online and remote environment in the face of the pandemic has been challenging. However, by seeking early input from older adults and other stakeholders as well as by collaborating across disciplinary lines, our team has developed a cohesive plan that maintains the integrity of the intended study without compromising the health and safety of those involved. As Richardson et al. (Reference Richardson, Carroll, Close, Gordon, O’Brien and Quinn2020) noted, studies involving older people in a world with COVID-19 will become even more challenging not only because of the ongoing fear of the contagion but also because of the expected tightening of fiscal resources for such research. Although the authors emphasized the need to find innovative ways to consolidate studies of COVID-19 with important non-COVID-19 research priorities for older people, we argue that such a gap no longer exists. All aging studies going forward must consider the impact of the pandemic. We must ensure that our research is designed in accordance with current and potential high-risk scenarios that mediate hazards by leveraging cross-disciplinary expertise. In this way, our proposed continuum shifts the focus away from whether a study is COVID-19-focused to a more open model of innovation (Lifshitz-Assaf, Reference Lifshitz-Assaf2018) in which multidisciplinary teams work beyond their traditional disciplinary silos. Interestingly, Richardson and colleagues (Reference Richardson, Carroll, Close, Gordon, O’Brien and Quinn2020) highlighted the value of large-scale research platforms in the age of COVID-19: “…doing fewer studies at larger scale pays dividends – duplication is reduced, participants can be recruited, and data collected at speed and results are more robust” (pp. 4–5). We also propose the formation of a Canadian-led consortium or network that brings together researchers and their projects from diverse fields of aging so we can consolidate our efforts and share strategies that ensure that the intersectionality and complex needs of our aging population are addressed. We invite readers to consider where their research fits in the continuum of pandemic research and how we can work together to advance aging research in the face of COVID-19 both locally and globally.