1. Introduction
In 1903, a JAMA editorial entitled “Suicides of physicians and the reasons” alerted about suicide among physicians in the United States of America. It noted that “they far exceed the average ratio of suicides in the general population.” [1] After more than a century, physicians’ suicides remain a major public health issue. A 2004 meta-analysis reported suicide ratio to be 1.41 (95% CI = 1.21–1.65) among male physicians and 2.27 (95% CI = 1.90–2.73) among female physicians [Reference Schernhammer and Colditz2], compared to the general population. Suicides are multifactorial, but severe mental illnesses account for 47%–74% of the population attributable risk of suicide [Reference Swanson, Bonnie and Appelbaum3]. Better understanding of the contributing factors, such as affective disorders and work-related stress, could help prevent suicide.
Several contributing factors seem to appear early in medical studies. In a meta-analysis [Reference Mata4] of 54 studies and 17,560 subjects, the prevalence of depressive symptoms in residents was estimated to be 28.8% (CI = 25.3–32.5). Rotenstein et al. [Reference Rotenstein5] explored medical students before residency and found 167 cross-sectional studies totaling 116,628 individuals and 16 longitudinal studies totaling 5728 individuals from 43 countries. The prevalence of current depression or depressive symptoms was 27.2% (CI, 24.7–29.9%) and the prevalence of suicidal ideation was 11.1% (CI 9.0–13.7%). The prevalence did not significantly differ between studies of either preclinical or clinical students. Using the CIDI scale [Reference Kessler and Ustün6], a European epidemiological study [7] found a 12-month prevalence of depression in the general population to be 3.9% (CI 3.6–4.2%). In the US general population, the same scale estimated the 12-month prevalence of a major depressive episode to be 9.3% among 18–25 and 7.2% among 26–49 year-olds [Reference Kessler8]. In the student population, a study including totaling 17,348 students from 23 countries estimated the prevalence of current depression (BDI score >8) to be 19% in men and 22% in women [Reference Steptoe, Tsuda, Tanaka and Wardle9].
Thus, a reasonable hypothesis is that medical students are more depressed than the general population, even before residency. Such early onset of distress could affect the mental health of physicians. Limited cross-sectional data suggest that the prevalence of psychological distress is higher among more advanced students. One longitudinal study followed medical students as they transitioned from Medical School into residency. It found that those who worry extensively are more likely to develop exhaustion 6–10 months after graduation [Reference Dahlin, Fjell and Runeson10]. Students experiencing psychological distress may be more vulnerable to mental health problems after graduation. Suicide prevention among physicians requires managing early stress during medical studies.
Rotenstein et al. hypothesized that possible causes of current depressive and suicidal symptomatology in medical students likely include stress and anxiety associated with the competitiveness of medical school. Exploring the potentially deleterious impact of medical studies on mental health, Brazeau et al. believe that, before embarking on their studies, medical students experience less burnout (27.3 vs 37.3, p < 0.001) and have fewer depressive symptoms (26.2 vs 42.4, p < 0.0001) than the general population [Reference Brazeau11]. The same team reported more symptoms of depression in medical students during their studies and early career than in the general population [Reference Dyrbye12]. Actually, the notion of burnout could partly explain the emergence of depressive and suicidal symptoms. Burnout is a multifaceted work-related construct created by Freudenberger [Reference Freudenberger13]. It was developed for health professions [Reference Maslach and Jackson14] by Maslach et al. in the eighties. Burnout occurs when three categories of symptoms combine - ‘Emotional Exhaustion’ (EE), ‘Depersonalization’ (DP), and ‘Personal Accomplishment’ (PA). Emotional Exhaustion is defined as an extreme fatigue due to continuous exposure to stressors, with the feeling of being drained of emotional resources. Depersonalization occurs when the attitude becomes negative, cold and detached. Gradually, the affected workers disengage from their work, as well as their relations with co-workers, and develop pejorative cynical conceptions. The Personal Accomplishment category refers to a low self-esteem, reflecting both the feeling of being ineffective in the work and not being up for the position.
Though originally developed for medical professions, the burnout syndrome was subsequently extended to all workers. It has been routinely used over the past decade. Still, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders does not consider burnout a disease. Yet, burnout has been established as a legitimate cause for sick leave in several countries, including Sweden [Reference Friberg15]. It has been identified as a factor influencing health status and help-seeking with health services in the 10th edition of the International Classification of Diseases (ICD-10) where burnout is coded Z73.0 and defined as a state of vital exhaustion [16]. The emergence of the burnout concept has led to new studies among physicians, residents, and medical students. Burnout is shown by a continuous measure that can be evaluated by dedicated scales over one year. The Maslach Burnout Inventory (MBI) is the most widely used scale in the world and exists in several versions to suit the populations studied: the original HSS (1981) for health professionals, GS (1996) for the general population and SS (2002) for students [Reference Schaufeli, Martinez, Pinto, Salanova and Bakker17]. Since the beginning of the 2000’s, other scales have appeared: the Oldenburg Burnout Inventory (OLBI) [Reference Demerouti, Bakker, Vardakou and Kantas18] and the Copenhagen Burnout Inventory (CBI) [Reference Kristensen, Borritz, Villadsen and Christensen19]. The MBI is used to classify enduring burnout into low, intermediate, and high levels. To assess an individual's burnout level, the authors recommend comparing his scores to the country's standard cut-off point established in epidemiological studies [Reference Maslach, Jackson and Schwab20, Reference Maslach, Jackson and Leiter21]. The strength of the MBI lies both in its 30-year-long use and validation - especially in students [Reference Schaufeli, Martinez, Pinto, Salanova and Bakker17]- in many languages. The CBI is considered very similar to the MBI with construct validity equivalence : one study [Reference Maroco and Campos22] compared the 3 scales (MBI-SS, CBI-SS and OLBI-SS) and found that the validity related to the construction can be accepted for CBI-SS and MBI-SS but not for OLBI-SS.
Previous reviews, both in residents and in medical students [Reference Ishak23, Reference Fares, Al Tabosh, Saadeddin and El Mouhayyar24], have identified the prevalence of burn-out to be between 17.6% and 82%. This broad range could be explained by the different versions of the MBI assessment and cut-off scales. Moreover, medical studies differ across countries and work environments have been changing. Evolutions have included lower mortality rate, emerging specialties (palliative care, anti-pain teams, or rehabilitation units), new medical tests and therapies, fewer paramedical staff, hospital beds reduction, and more administrative tasks. New technologies, like smartphones, have also weakened the boundaries between private and professional lives. Thus, our aim is to precisely evaluate the current prevalence of burnout. In this article, we conduct a meta-analysis of published studies and several meta-regressions to identify potential confounding factors. We propose to use the most widely validated scales and to focus on the past eight years for clinical relevance and homogeneity. Thus, living (mobile phones, social networks, or emails), working, and studying (including exams) environments are more homogeneous. We then examine the effects of year, gender, and geographic area.
2. Material and methods
2.1 Data sources
Two independent investigators (AF and BC) performed systematic bibliographic Medline searches using the following queries ("burnout, professional"[MAJR] OR ("burnout, professional"[TI] OR "professional burnout"[TI] OR "physical and emotional exhaustion state"[TI] OR "occupation-related stress disorder, nos"[TI])) AND ("students, medical"[MAJR] OR ("students, medical"[TI] OR "medical students"[TI] OR "student, medical"[TI] OR "medical student"[TI]). The search was conducted in January 2018. The bibliography of the selected articles was subsequently screened to identify other studies which had not been identified during the initial search.
2.2 Study selection
We only retained the studies which reported on the burnout of medical students before residency (undergraduate students) and included prevalence data in this specific population. Studies including students in other medical fields (as nurses) were removed. The language of the publication was restricted to English, because we needed to deeply understand the methodology used. Based on our aim to assess the recent evolution of students' mental health, we only retained the articles published between January 1, 2010 and December 31, 2017. Burnout had to have been assessed using one validated scale (MBI or CBI). The flow-chart is shown in Supplementary Fig. 1. Excluded articles and the reasons for exclusion are given in Supplementary Table 1.
2.3 Data extraction
We systematically extracted and recorded data about diagnostic assessment, sample size, sample characteristics (especially about gender), country, year of publication, average burnout prevalence as specified by the authors, and response rate.
2.4 Statistical analyses
To conduct the meta-analysis, we applied the DerSimonian–Laird method and used the OpenMetaAnalyst software [Reference Wallace, Schmid, Lau and Trikalinos25]. As we expected great between-study heterogeneity, we elected to use a continuous random-effects method. Then, data were split according to continents and clinical scales to conduct subgroup meta-analyses. A meta-regression was performed to detect a gender impact or an effect of response rate. Biases and outliers were detected using sensitivity analysis (leave-one-out method). A funnel plot was constructed using the metaphor R package [Reference Viechtbauer26], and a bilateral alpha-risk of 0.05 was assumed.
3. Results
3.1 Prevalence of current burnout in medical students between 2010 and 2018
The systematic review found 24 studies [Reference Brazeau11, Reference Dyrbye12, Reference Cecil, McHale, Hart and Laidlaw27–Reference Al-Alawi48] totaling 17,431 medical students worldwide (Table 1). Among them, 8060 suffered from burnout. We estimated its prevalence to be 44.2% [33.4%–55.0%] (Fig. 1). Information about the prevalence of each subset of symptoms was given in nine studies including 7588 students. The prevalence of ‘emotional exhaustion,’ ‘depersonalization,’ and ‘personal accomplishment’ was estimated to be 40.8% [32.8%–48.9%], 35.1% [27.2%–43.0%], and 27.4% [20.5%–34.3%] respectively (Supplementary Fig. 2).
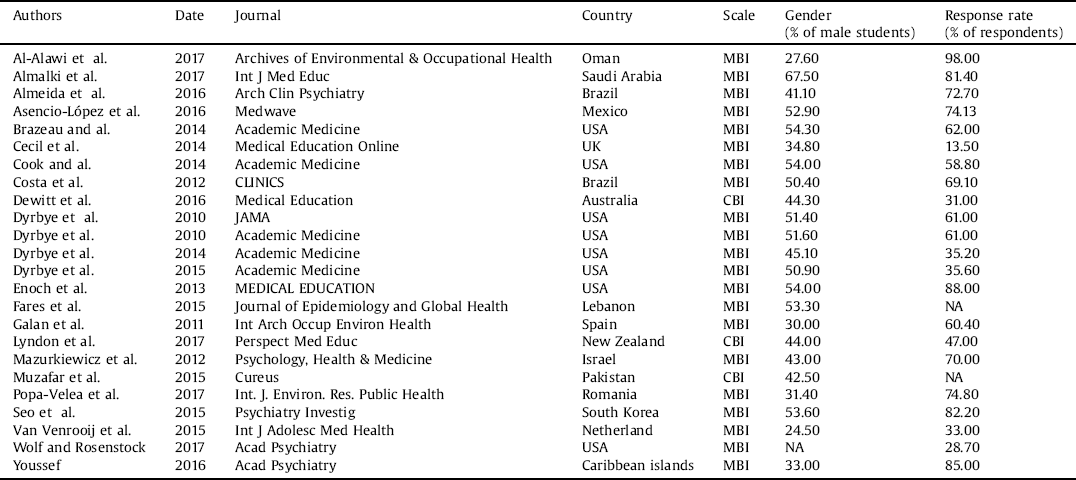
Table 1 Studies of burnout in medical students.

MBI: Maslach Burnout Inventory – CBI: Copenhagen Burnout Inventory – NA: not available.
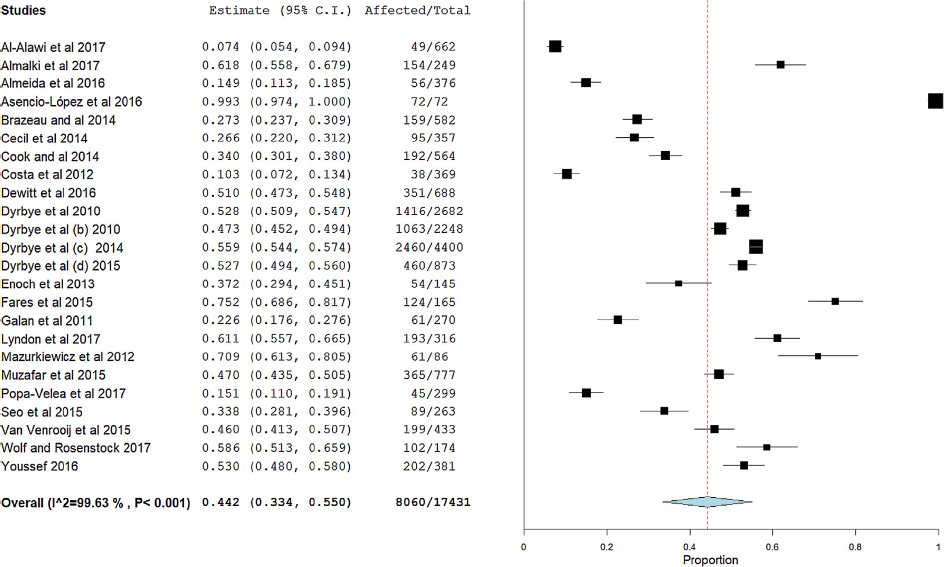
Fig. 1. Forest plot showing the prevalence of burnout in medical students.
3.2 Factors affecting the prevalence of current burnout
As great heterogeneity was detected (I2 = 99.63 and p < 0.001), we tested for different sampling biases. Leave-one-out analysis was conducted to detect any publication bias (Supplementary Fig. 3). A funnel plot was constructed (Supplementary Fig. 4). One study lay outside the funnel plot, with burnout prevalence estimated to be 100% [Reference Asencio-López49]. This study was excluded from the meta-regression and subgroup analyses. Twenty studies used the Maslach Burnout Inventory (MBI) and three used the Copenhagen Burnout Inventory (CBI). Though CBI total scores were slightly higher, the difference was not significant (p = 0.45) (Supplementary Fig. 5).
As medical studies and mental health differ across countries, we searched for geographic disparities in prevalence. Countries were grouped into continental regions: North America, Asia, Europe, Oceania, the Middle East, and South & Central America. No studies were available for Africa. Prevalence in each continent is given in Fig. 2. Oceania and Middle East students exhibited the highest prevalence of burnout whereas students from South & Central America exhibited the lowest prevalence. The prevalence of burnout in the Middle East and Oceania significantly differed from Europe (p = 0.022; p<10−3 respectively) and South & Central America (p = 0.024; p = 0.03 respectively).

Fig. 2. Forest plot showing the continent-based prevalence of burnout in medical students.
We detected no effect of gender on the prevalence of burnout (Omnibus p-value = 0.07 – Fig. 3). The result of the meta-regression is shown in Fig. 3. The effect of the publication year was not significant (Omnibus p-value = 0.93; Supplementary Fig. 6). Effect of the response rates was also not significant (Omnibus p-value = 0.29 – Supplementary Fig. 7).

Fig. 3. Gender-based meta-regression of burnout in medical students.
4. Discussion
The present meta-analysis found the prevalence of current burnout to be 44.2% [33.4–55.0] among medical students. Several factors have been examined. Notably, we found no significant difference in prevalence between men and women. There were no longitudinal changes in prevalence during the past eight years. Such findings may result from insufficient statistical power and from the limited eight-year time span. However, we should keep in mind that attention to burnout among medical students has only relatively recently led to measuring and evaluating. Indeed, in their 2006 systematic review, Dyrbye et al. [Reference Dyrbye, Thomas and Shanafelt50] found no study about burnout among medical students in North America. Furthermore, the publication date imperfectly reflects the time of assessment, a parameter that is not always mentioned in the ensuing articles and therefore could not be included in the meta-regression. More longitudinal studies are needed to address the question of the gradual change of prevalence.
Finally, we found that geographic localization significantly affected the prevalence of current burnout. Oceania and, in a less extend, the Middle East, have higher levels of current burnout compared to South & Central America and Europe. Burnout does not occur as the result of a single cause. The main factors contributing to burnout in medical students include the curriculum with stress related to the competition, the exams or the cost of the studies, as well as hospital conditions with workload, exposure to patients’ suffering and death, style of management. Other external reasons could explain the variations between countries, notably the living conditions (war, terrorism, poverty,…). Additionally, we decided to group all the countries from Europe, despite a certain economic and politic heterogeneity between East and West European countries. However, since the Bologna agreements, a diploma acquired in one of the countries of the European union is valid throughout the union. Moreover, with the Erasmus program, there are many students exchange between the different European countries.
Our estimate is consistent with Ishak et al.'s estimate from their systematic review – between 45 and 71%. It is also consistent with Prins et al.'s [Reference Prins51] results in residents – 18 to 82% – and with Fares et al.'s [Reference Fares, Al Tabosh, Saadeddin and El Mouhayyar24] findings in preclinical medical students – 25 to 75%. The high prevalence of current burnout in medical students is not surprising and highlights medical students' high level of suffering before embarking on their residency. Burnout is related to depression and anxiety [Reference Bianchi, Schonfeld and Laurent52] and could explain the high prevalence of these psychiatric symptoms in medical students [Reference Rotenstein5]. It has been suggested that burnout may be a risk factor for depression and anxiety in the following years. Several studies have pointed that burnout seems to predict and increase depression [Reference Armon, Melamed, Toker, Berliner and Shapira53–Reference Shin, Noh, Jang, Park and Lee55]. Others have found that depression predicts burnout [Reference Campbell, Prochazka, Yamashita and Gopal56, Reference Salmela-Aro, Aunola and Nurmi57]. In brief, it has been proposed that burnout and depression were reciprocally related [Reference Salmela-Aro, Savolainen and Holopainen58, Reference Toker and Biron59]. Burnout has also been associated with anxiety [Reference Molina-Canales, Le Barbier, Brunel and Lasfargues60–Reference Pereira-Lima and Loureiro62], tobacco and alcohol consumption, antidepressants use, and suicidal thoughts [Reference Soler63, Reference Galam, Komly, Le Tourneur and Jund64]. As stated in the report by the French Academy of Medicine, burnout may appear before the development of a psychiatric disorder, including anxiety or depression [Reference Olie and Legeron65].
Consequently, comorbidity between depression or suicidal thoughts in medical students and burnout implies that prevention of mental health disorders should target students' working and studying environments. The competitiveness of medical school has been questioned [Reference Rotenstein5]. However, though forms of training and selection differ around the world, the relative stability of world prevalence contradicts this hypothesis. Other factors have been proposed to explain the high prevalence of current burnout, such as quantitative work overload, conflicting levels of dependency, the balance between responsibility and autonomy, young age, or the confrontation with suffering and dying patients. A recent French report from Dr Donata Marra [66] has proposed some suggestions to address this issue. The first step is to take into consideration the students and to recognize their emotions and suffering; in consequence, structures providing psychological support and help for orientation (choice of medical specialty) and warranting confidentiality should be available to each student in all faculties. A second step would be to reduce the workload and to adapt the modalities of evaluation with reducing the importance of ranking. Several studies have found a correlation between the number of hours worked and burnout. Reducing the workload has been associated with a decrease in burnout prevalence [Reference Barrack, Miller, Sotile, Sotile and Rubash67–Reference Jovanović69], an effect depending on the medical specialties [Reference Ferrari70]. The third recommendation provided by the Marra’s report is to train supervisors for teaching and management as well as for recognizing the distress symptoms of students. Finally, specific interventions should be considered to help students suffering from burnout symptoms. A meta-analysis of interventions for burnout in medical doctors has been published [Reference West, Dyrbye, Erwin and Shanafelt71]. It comprised 15 randomized trials of interventions to prevent burnout. Though there are not as many studies into medical students, interest has been growing [Reference Williams, Tricomi, Gupta and Janise72] and some attempts should be reported. Changes in the management, practices, and conceptions of students' well-being have been ongoing, mostly in North America. For instance, since 2011, Saint Louis University School of Medicine has been pursuing a multipronged strategy to address these issues in the preclinical years. These efforts have successfully decreased the level of depression and anxiety symptoms in students [Reference Slavin and Chibnall73]. For medical residents, several studies have shown that limiting weekly working hours reduced the risk of burnout [Reference Barrack, Miller, Sotile, Sotile and Rubash67–Reference van Vendeloo, Brand and Verheyen74]. A recent systematic review [Reference Wasson75] found 28 articles describing empirically evaluated interventions to improve medical students' emotional well-being. They included randomization focused on pass/fail grading systems (3 articles), mental health programs (n = 4), mind-body skill programs (n = 7), curriculum structure (n = 3), multicomponent program reform (n = 5), wellness programs (n = 4), and advising/mentoring programs (n = 3). An essential component of these interventions is the ongoing measurement of mental health outcomes across all four years of the curriculum. Efforts directed at changing the educational and clinical environments are also needed to reduce unnecessary stressors and create more positive settings for learning and clinical care. Peer support and companionship appear to be protective. Some students report humiliations and bullying in the hospital [Reference Auslender76]. It has been demonstrated that supervisors' types of leadership play a critical role in the well-being of the physicians they supervise [Reference Shanafelt and Noseworthy77]. Improvement of the relationships between students and supervisors is attainable.
Destigmatizing psychologic distress, promoting prevention, and recognizing the symptoms are crucial factors to encourage medical students to seek help. Thus, the growing number of studies over the past decade has increased professionals' and students' burnout awareness. Early interventions targeting students' suffering, should be viewed as a mean to prevent the development of any future psychiatric disorder. In addition, improving the well-being of medical students is also necessary to provide better care to patients, as a recent meta-analysis [Reference Shoji78] has found a clear impact of current burnout on work efficiency.
Our meta-analysis has some limitations. First, our methodology to review only articles written in English may have excluded some relevant articles from non-English speaking countries. Additionally, burnout remains an entity to better define across countries. Initially defined as a continuum [Reference Schaufeli, Leiter and Maslach79], burnout is nowadays refers as a dichotomous entity but cut-off to define it is variable. Schaufeli recommended to employ “only nation-specific and clinically derived cut-off points” [Reference Schaufeli and Van Dierendonck80]. Whereas it has been recommended to adapt the cut off for burnout based on the continuous score provided by the scales in some countries [Reference Schaufeli and Van Dierendonck80–Reference Dion and Tessier82], the cross national validity has been demonstrated [Reference Enzmann, Schaufeli and Girault83–Reference Bakker, Le Blanc and Schaufeli87]. For example, Popa-Velea et al [Reference Popa-Velea, Diaconescu, Mihăilescu and Jidveian Popescu45] considered “the criteria of burnout to be met if the participants had a score above 30 on the EE scale and if at least one of the scores of the other two dimensions were above the recommended cut-off points (DP: 11; PA: 35)”. Some included studies did not report their cut off for the 3 subscales of the MBI, so we cannot estimate their reliability [Reference Schaufeli and Van Dierendonck80]. On the 24 studies of the meta-analysis, 3 used CBI scale and 21 MBI scale. However, we provided a funnel plot to estimate this bias and decided to exclude a study [Reference Salmela-Aro, Aunola and Nurmi57] with obvious deviation from the others.
Another limitation is that the scales measuring burnout have been designed for enduring state. Consequently, they are relatively insensitive to minor fluctuations. Finally, the choice of a limited and short period may have decreased the number of studies included in our meta-analysis but warranted a better homogeneity. The working conditions of the medical student are time-dependent. Last decade has been associated with advances in medical science, development of new teaching and evaluation methods. Since 2010, new ways of communication resulting in an imperative to be always reachable have favored stress during the period of rest. In several private compagnies, the "right to disconnect" has been warranted to alleviate workers to disconnect from work and primarily not to engage in work-related electronic communications such as e-mails or messages during non-work hours but this is not the case in medicine. External conditions have also contributed to changes in hospital environment. The 2008 financial crisis had global impacts on health systems: reduction of budget and staff [Reference Kalafati88], degradation of work conditions for caregivers [Reference Rachiotis89].
The present meta-analysis shows that the current prevalence of burnout among medical students is important. Nearly one medical student out of two suffers from burnout. Awareness of mental health issues during medical studies and before residency is still in its infancy. However, this is the first step towards developing interventional trials to decrease the prevalence of burnout. Some attempts have already been tested, mainly in North America, with positive results. These methods should be evaluated and extended to other countries, including European countries and countries with higher prevalence of burnout.
Funding
No current external funding sources for this study.
Declaration of interest
The authors declare no conflict of interest related to this study.
Acknowledgements
We would like to thank Pascale Eisenberger from the Centre de Langues in Université Paris Descartes (France) for the English language editing. Boris Chaumette receives a postdoctoral fellowship from the Healthy Brains for Healthy Lives project (Talent program).
Appendix A Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.eurpsy.2018.08.006.






Comments
No Comments have been published for this article.