Persons with mental illness often have to struggle with a double problem. First, they have to cope with the symptoms of the disease itself; depending on the particular mental disorder they may have problems such as recurrent hallucinations, delusions, anxiety, or mood swings. These symptoms can make it difficult for someone with a mental illness to work, live independently or achieve a satisfactory quality of life. Second, the misunderstandings of society about the various mental disorders result in stigma. Some persons who manage their mental illness well enough to work still have tremendous difficulties finding a job because employers discriminate against them. Thus, mental illness results not only in the difficulties arising from the symptoms of the disease but also in disadvantages through society's reactions. As a further complication, some people with mental illness may accept the common prejudices about mental illness, turn them against themselves, and lose self-confidence. The latter is referred to as ‘self-stigma’ and will be discussed further below.
In this paper we want to give a conceptual background of public and self-stigma, discuss how stigma of mental illness interferes with empowerment of persons with mental illness and with service use, review strategies to reduce stigmatization of persons with mental illness and give examples of current initiatives. We believe that it is important to review conceptually relevant work in the field of mental illness stigma to provide a framework for a better interpretation of various empirical findings. Therefore, in this review we wish to summarize conceptually driven work and research on mental illness stigma from different countries. We focussed on two concepts that have been most relevant in research on mental illness stigma: Stigma as conceptualised by Link and Phelan Reference Link and Phelan[63] and the concept of Corrigan and coworkers Reference Corrigan[28]. In this paper, we will first conceptualise stigma using an integrative conceptualisation, combining the two mentioned concepts. We will then discuss differences between these two concepts and their consequences for research and interpretation of results.
This review may be of help to readers from different backgrounds: It may be useful for researchers as a framework to generate and test hypotheses; for clinicians who work with people with mental illness to recognise public stigma and self-stigma more easily and help people with mental illness to cope with the consequences; for mental health professionals to question their own possibly stigmatising attitudes towards people with mental illness; for teachers and students to establish educational and other anti-stigma initiatives in their schools or universities; last not least for people with mental illness to better understand stigma and self-stigma and to actively fight stigma and its consequences in their environment.
1. What is stigma?
Stigmatizing attitudes contain some core assumptions. Media analyses of film and print have identified three common misconceptions about people with mental illness: they are homicidal maniacs who should be feared; they are rebellious, free spirits; or they have childlike perceptions of the world that should be marveled [40,50,103]. Independent factor analyses from Canada, England and Germany confirm these findings by identifying the following factors: First, fear and exclusion: persons with severe mental illness are to be feared and, therefore, kept out of communities; second, authoritarianism: persons with severe mental illness are irresponsible, so life decisions should be made by others; and third, benevolence: persons with severe mental illness are childlike and need to be cared for [7,11,101]. Although stigmatizing attitudes are not confined to mental illness, the general public seems to disapprove of persons with psychiatric disabilities more than of persons with physical illness [83,97,105]. Persons with mental illness are more likely to be seen as responsible for causing their illness [22,105]. This assumption of responsibility is less pronounced for schizophrenia than for substance addiction and eating disorders Reference Angermeyer and Matschinger[4]. These attitudes lead to corresponding discriminatory behavior. Citizens are less likely to hire persons with mental illness Reference Bordieri and Drehmer[9], less likely to rent them apartments Reference Page[79], and more likely to falsely press charges for violent crimes [98,99].
As an example of a person suffering from stigma, consider what happened to Anne. Anne is 25years old and has been hospitalised several times with acute symptoms of schizophrenia. For two years, she had been symptom-free, living on her own, working in a local tourist information office and enjoying an active social life. Recently though, she had a relapse of her mental illness. She again was hospitalised and it took her two months to recover and to get ready to go back to work again. However, after recovery she realised that getting over the symptoms of her disease did not suffice: Her employer discharged her because he believed she could have a dangerous outburst in the office due to her mental illness. In addition, her family convinced her that it was too risky to live on her own and made her move back to her parents’ home. Since her family lived in another town, that made her lose her friends. In summary, despite a good recovery from the symptoms of her mental illness, within a month after discharge from the mental hospital Anne had lost her job, appartment and friends. Imagine in comparison a person with a chronic somatic illness like diabetes. Similar to schizophrenia, diabetes can lead to severe relapses and hospitalisations. However, unlike a person with schizophrenia, a person with diabetes is unlikely to encounter comparably consequential public stigma related to her illness.
2. Public and self-stigma
2.1. A social cognitive model of public stigma
Public stigma comprises reactions of the general public towards a group based on stigma about that group. Although we are used to distinguishing between groups in society and to label these groups with different attributes, this is not a self-evident process. Most human differences are mainly ignored and socially irrelevant in Western societies of our time. For example, the color of one's car or the size of one's shoes do not matter for most people under most circumstances. However, other personal features like skin-color, sexual orientation or income are often relevant to one's social appearance. There is obviously a social selection of which human qualities matter socially and which do not.
It is often taken for granted to distinguish between different groups in society and to label human differences accordingly. However, every demarcation of groups requires an oversimplification. Even with obvious attributes like skin-color, there is no clear demarcation line between, for example, 'black' and 'white'. Even more so, there is no sharp line between mental health and mental illness Reference Link and Phelan[63].
That cultural attitudes to behavior and (mental) illness change substantially over time is another aspect of the social selection of human differences in creating groups Reference Conrad and Schneider[13]. Whether patterns of behavior, thinking and feeling are being noticed at all and if so, whether they are described in moral, psychosocial or medical terms is influenced by societal discourse and usually varies over time. Attention deficit hyperactivity disorder is an example of a label that was unknown a few decades ago and is likely to change again Reference Seidler[95].
It is further important to note that labeling often implies a separation of 'us' from 'them'. This separation easily leads to the belief that 'they' are fundamentally different from 'us' and that 'they' even are the thing they are labelled. 'They' become fundamentally different from those who do not share a negative label, so that 'they' appear to be a completely different sort of people Reference Link and Phelan[63]. Our use of language is revealing regarding the use of labels to distinguish 'us' from 'them'. For example, it is common to call someone a 'schizophrenic' instead to call her or him a person with schizophrenia. For physical illness, things are often handled differently and people usually say, a person has cancer. The person afflicted with cancer remains one of 'us' and has an attribute, while the 'schizophrenic' becomes one of 'them' and is the label we affix to the person Reference Link and Phelan[63]. In this way, language can be a powerful source and sign of stigmatization.
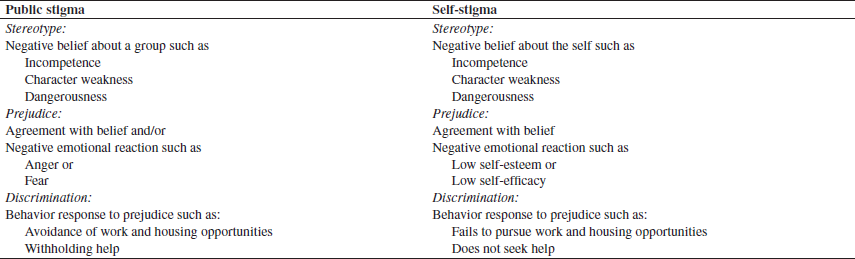
Given this background of distinguishing between groups, labeling and separating 'us' from 'them', social psychology has identified different cognitive, emotional and behavioral aspects of public stigma: stereotypes, prejudice, and discrimination (see Table 1). It is important for both theoretical research and practical initiatives to understand these components. Stereotypes are knowledge structures known to most members of a social group [48,53]. Stereotypes are an efficient way to categorize information about different social groups because they contain collective opinions about groups of persons. They are efficient in the sense that they quickly generate impressions and expectations of persons who belong to a stereotyped group Reference Hamilton, Sherman, Wyer, RS and Srull[45].
Table 1 Components of Public and Self-Stigma
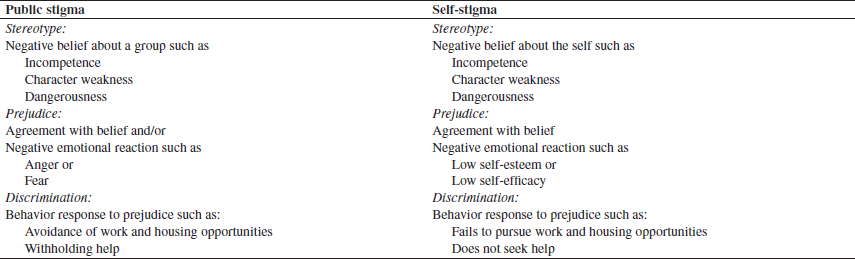
People do not necessarily agree with the stereotypes they are aware of Reference Jussim, Nelson, Manis and Soffin[54]. Many persons may, for example, be aware of stereotypes of different ethnic groups but do not think these stereotypes are valid. Prejudiced persons, on the other hand, endorse these negative stereotypes (“That's right! All persons with mental illness are violent“) and have negative emotional reactions as a consequence (“They all scare me“) [35,36,48]. Prejudice leads to discrimination as a behavioral reaction Reference Crocker, Major, Steele, Gilbert and Fiske[32]. Prejudice that yields anger can lead to hostile behavior. In the case of mental illness, angry prejudice may lead to withholding help or replacing health care with the criminal justice system Reference Corrigan[28]. Fear leads to avoidant behavior. For example, employers do not want persons with mental illness around them so they do not hire them. This association between perceived dangerousness of persons with mental illness, fear, and increased social distance has been validated for different countries, including Germany Reference Angermeyer and Matschinger[3], Russia Reference Angermeyer, Buyantugs, Kenzine and Matschinger[1] and the United States Reference Corrigan[15].
Stereotypes and prejudice alone are not sufficient for stigma. In addition, social, economic and political power is necessary to stigmatize. For example, if individuals with mental illness form stereotypes and prejudices against staff in a mental health service, this staff is unlikely to become a stigmatized group because the persons with mental illness simply do not have the social power to put serious discriminatory consequences against the staff into practice Reference Link and Phelan[63].
In summary, public stigma consists of these three elements - stereotypes, prejudice and discrimination - in the context of power differences and leads to reactions of the general public towards the stigmatised group as a result of stigma.
2.2. A social cognitive model of self-stigma
Self-stigma refers to the reactions of individuals who belong to a stigmatized group and turn the stigmatizing attitudes against themselves Reference Corrigan and Watson[25]. Like public stigma, self-stigma comprises of stereotyping, prejudice and discrimination (Table 1). First, persons who turn prejudice against themselves agree with the stereotype: “That's right; I am weak and unable to care for myself!” Second, self-prejudice leads to negative emotional reactions, especially low self-esteem and self-efficacy Reference Wright, Gronfein and Owens[106]. Also self-prejudice leads to behavior responses. Because of their self-prejudices, persons with mental illness may fail to pursue work or independent living opportunities. If they fail to reach this goal this is often not due to their mental illness itself but due to their self-discriminating behavior Reference Link, Cullen, Struening and Shrout[66]. How can self-stigma arise? Many persons with mental illness know the stereotypes about their group such as the belief that people with mental illness are incompetent Reference Hayward and Bright[47]. But, as in public stigma, knowledge alone does not necessarily lead to stigma, if persons are aware of the stereotypes but do not agree with them Reference Crocker and Major[33]. Thus, fortunately for many persons with mental illness, awareness of stereotypes alone does not lead to self-stigma.
3. Different conceptualizations of stigma
The conceptualization of mental illness stigma given above combines two leading current concepts, i.e. the one of Corrigan and coworkers Reference Corrigan[28] and the concept of Link and colleagues Reference Link and Phelan[63].
Corrigan and colleagues focus on the cognitive and behavioral core features of mental illness stigma: Stereotypes (cognitive knowledge structures), prejudice (cognitive and emotional consequence of stereotypes) and discrimination (behavioral consequence of prejudice). Focussing on these core components, their model allows one to examine different elements of stigmatizing attitudes and behaviors and their modifiability by anti-stigma initiatives. It is a merit of this model that it makes it feasible to disentangle different phenomena underlying stigma and to make them accessible to empirical research.
In the definition of Link and Phelan, “stigma exists when elements of labeling, stereotyping, separation, status loss, and discrimination co-occur in a power situation that allows these processes to unfold” Reference Link and Phelan[63]. In their concept, stereotypes, separation, and status loss/discrimination parallel Corrigan's stereotypes, prejudice and discrimination. Since Link and colleagues deal with various stigmata, although focussing on mental illness stigma, they stress that no definition of stigma can be universally applicable. Therefore, Link and colleagues emphasize that definitions of stigma should always be made transparent by the respective researchers, and dictionary definitions alone such as “a mark of disgrace” are by no means sufficient. Writing from a sociological perspective, in comparison to the model of Corrigan and colleagues, Link and Phelan put more stress on two societal aspects: First, as a precondition of stigma differences between persons have to be noticed, to be regarded as relevant and to be labeled accordingly. This labeling process is at the core of Link's modified labeling theory Reference Link, Cullen, Struening and Shrout[66]. Second, for stigma to unfold its deleterious consequences, the stigmatizing group has to be in a more powerful position than the stigmatized group. Therefore, for instance, jokes about powerful groups such as politicians may be stereotyping but do not normally lead to discrimination and therefore are not ‘stigmatizing’ in a strict sense of the word. This sociological perspective does not contradict the model of Corrigan and colleagues, but helps to connect it with societal aspects. A further focus of the approach of Link and Phelan is the subjective expectation and experience of being labeled and discriminated because of one's mental illness.
Although the two models are well compatible, they still seem to show slightly different consequences in methodology, results and interpretation of studies. Link and colleagues in their research focussed on the expectations and experiences of being labeled and stigmatized, which was usually measured by Link's Perceived Devaluation and Discrimination Scale, and on the consequences of stigma on self-esteem (e.g. [62,64,67]). Thus the emphasis here is on what we call self-stigma including recent work that operationalises their concept how stigma affects individuals Reference Ritsher and Phelan[86]. In the field of anti-stigma initiatives, the sociological focus on the complexities of discriminating mechanisms in a society seems to lead to a more sceptical approach towards anti-stigma initiatives because effects at an individual level may be outweighed by other paths of discrimination (see our discussion below).
The research of Corrigan and colleagues focussed on the central features of Corrigan's model: Stereotypes, prejudice and (discriminating) behavior of the public towards people with mental illness. Several studies examined these elements and their interrelationship, especially perceptions of dangerousness, fear and social distance Reference Corrigan, Green, Lundin, Kubiak and Penn[18]; authoritarianism, benevolence and social distance Reference Corrigan, Edwards, Green, Diwan and Penn[17]; controllability, responsibility and stability Reference Corrigan, River, Lundin, Wasowski, Campion and Mathisen[22]. As an extension of these studies, the effect of anti-stigma initiatives using the strategies of education and contact (see below) was examined in several studies [21,23]. Thus, the research focuses, slightly different from the research of Link and colleagues, on public stigma. Recently though, Corrigan and colleagues have been bridging the gap to the work of Link and coworkers and have extended their research to include conceptual work on self-stigma Reference Corrigan and Watson[25], to the perception of discrimination by people with mental illness Reference Corrigan, Thompson, Lambert, Sangster, Noel and Campbell[27] and are currently developing a measure of self-stigma in mental illness that operationalises their concept of self-stigma.
4. The consequences of stigma
As far as mental illness is concerned, stigmas seem to be widely supported by the general public. This is true for the United States [61,81] and for other Western nations including Norway Reference Hamre, Dahl and Malt[46], Greece Reference Madianos, Madianou, Vlachonikolis and Stefanis[71] or Germany [2,52] while levels of stigmatisation may differ between nations. Unfortunately, research suggests that public attitudes toward people with mental illness seem to have become more stigmatizing over the last decades: Survey research suggests that a representative 1996 population sample in the US was 2.5 times more likely to endorse dangerousness stigma than a comparable 1950 group, i.e. perceptions that mentally ill people are violent or frightening substantially increased Reference Phelan, Link, Stueve and Pescosolido[81]. A recent German study also found increasing stigmatizing attitudes towards people with schizophrenia Reference Angermeyer and Matschinger[5]. On the other hand, the use of outpatient psychotherapy in the US increased between 1987 to 1997, at least among people about 60years old, among the unemployed and persons with mood disorders Reference Olfson, Marcus, Druss and Pincus[78]. It has been speculated that the increased use of psychotherapy in these groups may be due to decreased stigmatisation especially of mood disorders. However, the link between stigma and use of psychotherapy was not assessed in this study, psychotherapy was very broadly defined including treatments of only one or two sessions, and the overall use of psychotherapy did not change in this period. In addition, being in psychotherapy may not necessarily mean to consider oneself having a ‘mental illness’ or to be considered ‘mentally ill’ by one's environment, so different stigmata may apply and change independently over time. Another sobering fact is that mental health professionals equally support stigmatizing views [44,58,80,92].
Two deleterious consequences of stigma can only briefly be mentioned here. First, public stigma results in everyday-life discriminations encountered by persons with mental illness in interpersonal interactions as well as in stereotyping and negative images of mental illness in the media Reference Wahl[103]. Second, structural discrimination includes private and public institutions that intentionally or unintentionally restrict opportunities of persons with mental illness Reference Corrigan, Markowitz and Watson[19]. Examples of structural discrimination are discriminatory legislation or allocation of comparatively fewer financial resources into the mental health system than into the somatic medical system [26,73]. It is important to note that for example a person with schizophrenia may experience structural discrimination whether or not someone treats her or him in a discriminatory way because of some stereotype about schizophrenia Reference Link and Phelan[63].
In this paper we want to focus on two other negative consequences of stigma that are both related to the way a person with mental illness reacts to the experience of being stigmatized in the society: Self-stigma/empowerment and fear of stigma as a reason to avoid treatment. We focus on these two aspects because both are highly relevant for clinicians working in the mental health field. By this we do not imply that stigma is only an individual problem. In contrast we believe stigma to be primarily a social problem that should be addressed by public approaches Reference Mills[76]. Still, until stigma has been reduced in society, the clinician should be aware of the meaning and consequences of stigma for individuals with mental illness.
4.1. Self-stigma and empowerment
Research has shown that empowerment and self-stigma are opposite poles on a continuum Reference Corrigan[14]. At one end of the continuum are persons who are heavily influenced by the pessimistic expectations about mental illness, leading to their having low self-esteem. These are the self-stigmatized. On the other end are persons with psychiatric disability who, despite this disability, have positive self-esteem and are not significantly encumbered.
Many persons who are discriminated against and suffer from public stigma do not experience self-stigma while others do. Correspondingly, the evidence is equivocal on this point: Some studies suggest that people with mental illness, who are generally well aware of the prejudices against them, show diminished self-esteem [65,66,72,87,102,106]. On the other hand, other surveys did not find that awareness of common stereotypes leads to diminished self-esteem in persons with mental illness Reference Hayward and Bright[47]. Even more amazingly, some stigmatized minority groups show increased self-esteem, including persons of color Reference Hoelter[49] and people with physical disabilities Reference Llewellyn[68]. Being stigmatized may stimulate psychological reactance Reference Brehm[10] so that instead of applying the common prejudices to themselves persons oppose the negative evaluation which results in positive self-perceptions. This fact that some react with righteous anger to stigma, while others are indifferent to stigma and yet another group self-stigmatizes has been called the paradox of self-stigma and mental illness Reference Corrigan and Watson[25]. Why do people react so differently to public stigma? Corrigan and colleagues developed a model of the personal response to mental illness stigma (Fig. 1).
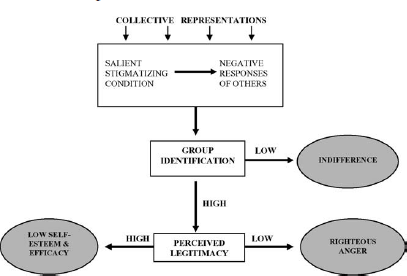
Fig. 1 Model of personal response to mental illness stigma (adapted from Reference Corrigan and Watson[25]).
Persons with a stigmatizing condition like serious mental illness perceive and interpret their condition and the negative responses of others. The collective representations in the form of common stereotypes influence both the responses of others and the interpretation of the stigmatized. Persons with a stigmatizing condition who do not identify with the stigmatized group are likely to remain indifferent to stigma because they do not feel that prejudices and discrimination actually refer to them (Fig. 1). However, those who identify with the group of the mentally ill apply the stigma to themselves Reference Jetten, Spears and Manstead[51]. Their reaction is moderated by perceived legitimacy. If they consider the stigmatizing attitudes to be legitimate, their self-esteem and self-efficacy are likely to be low [91,93]. If, on the other hand, they regard public stigma to be illegitimate and unfair, they will probably react with righteous anger Reference Frable, Wortman and Joseph[41] (Fig. 1). People who are righteously angry are often active in empowerment efforts, targeting the quality of services.
Related to empowerment and self-stigma is the issue of stigma and disclosure. To disclose one's mental illness may have both significant benefits, e.g. possibly increased self-esteem and decreased distress of keeping one's illness a secret, and costs, e.g. social disapproval. Whether or not individuals decide to disclose will depend on context and their sense of identity Reference Corrigan and Matthews[29]. For instance, if a woman with mental illness does not consider her illness a relevant part of her identity, she will be unlikely to tell her relatives about her mental illness, especially if those have repeatedly made stigmatising remarks about mental illness. If, on the other hand, a man with mental illness who is active in self-help groups and regards his mental illness as an important part of his life has trustworthy colleagues that have not shown discriminating behavior against people with mental illness, he is more likely to disclose his mental illness at work.
While the model of self-stigma, originating in social psychological research on other stigmatized groups (e.g. people of color, people with physical diseases), is useful to understand the different ways people react to stigma, three aspects have to be included to take into account the special case of mental illness. First, self-stigma resulting in decreased self-esteem and self-efficacy must be distinguished from decreased self-esteem during depressive syndromes that are common not only in affective disorders. Second, reaction to stigmatizing conditions depends on the awareness of having a mental illness, which may be impaired during episodes of, for instance, a psychotic condition Reference Rüsch and Corrigan[90]. Third, the reaction to a stigmatizing environment is dependent on one's perception of the subtle stigmatizing messages from other people. This social cognition may be impaired in serious mental illness such as schizophrenia Reference Corrigan and Penn[20].
4.2. Fear of stigma as a barrier to use health services
Psychiatric symptoms and life disabilities of many persons living with mental illness can be significantly improved by various psychiatric and psychosocial treatments. Unfortunately, many persons who are likely to benefit from that kind of treatment either choose to never start treatment or opt to end it prematurely. This low rate of participation is not only the case in minor mental illness such as adjustment disorders; less than two thirds of persons with schizophrenia take part in treatment Reference Regier, Narrow, Rae and Manderscheid[85] and generally people with serious mental illness do not participate in treatment more often than those with minor disorders Reference Narrow, Regier, Norquist, Rae, Kennedy and Arons[77]. While many persons do not start treatment, even more do not fully adhere to prescribed interventions once they are begun. On average, almost half of persons on anti-psychotic medication fail to comply with the prescribed medication fully Reference Cramer and Rosenheck[31]. This is a major reason for the high rate of relapse that causes almost a billion dollar increase in hospital costs per year world wide Reference Weiden and Olfson[104].
Health belief models explain why persons choose not to take part in treatments. These models assume that humans act rationally in ways that diminish perceived threats (disease symptoms) and enhance perceived benefits (improved health following treatment) Reference Rosenstock[88]. Key elements in the equation that produce health related behavior are negative effects of treatment, such as side-effects of medication. But of major importance is also the effect on the social environment; i.e. being labeled and stigmatized as a person with a mental illness after treatment.
Persons with mental illness who try to avoid stigma by not pursuing psychiatric services are called “potential consumers”. They consider themselves part of the public, are aware of the common prejudices against persons with mental illness and do not want to be seen as part of the “mentally ill” minority and thus avoid public stigma. They also avoid decreased self-esteem resulting from being mentally ill, i.e. self-stigma. Unlike other stigmatized groups, like those of color, persons with mental illness do not share a readily visible condition. Therefore the greatest single cue that produces public stigma is the label Reference Link[61]; this label usually stems from participating in psychiatric services. Potential consumers may opt not to access care as a way to avoid this label.
There are some data to support our assertion that stigma limits service use. Persons in a large epidemiologic study were less likely to use services if they expected negative reactions of family members Reference Leaf, Bruce and Tischler[59]. In addition, there are other variables that interact with stigma and service use. Demographics may play a major role; in a study of outpatients with depression, only older persons showed a significant association between perceived stigma and disruption of treatment Reference Sirey, Bruce, Alexopoulos, Perlick, Raue and Friedman[96]. Also social status appears to influence service use because less educated and poorer people express more concern about family reactions Reference Leaf, Bruce, Tischler and Holzer[60]. The vocational background of potential consumers is also relevant. Contrary to what one might expect, those who should know better do avoid treatment due to fear of stigma: Only a third of medical students with clinical levels of distress sought help because they were concerned about stigma [12,39].
Further research needs to confirm the link between stigma and service use. But the data available so far are sufficient to suggest that the reduction of public and self-stigma will be an important means to increase treatment participation (for an overview see Reference Corrigan and Rüsch[24]).
5. Ways to reduce the stigma towards mental illness
In Germany, the US and many other countries, consumer groups have actively targeted stigma in an attempt to improve the lives of persons with mental illness. Due to the large number of successful programmes, the following examples are by no means meant to be comprehensive. As a particularly successful example in the US, the National Alliance of the Mentally Ill, a group of family members and persons with mental illness, has been educating the public in order to diminish stigmatizing conditions; e.g. by pressing for better legal protection for persons with mental illness in the areas of housing and work. Called ‘stigmabusters’, the NAMI-programme has been successfully used to protest against media representations of stigma in all 50 states of the US. In Germany, there are various anti-stigma campaigns, two of which should be mentioned here: BASTA – The alliance for mentally ill people (previously called ‘Bavarian Anti-Stigma Action’; ‘basta’ also meaning ‘stop’ in Italian and German), based in Munich, is active in various fields, including protest campaigns using email alerts, extensive education programmes in schools and police academies with active participation of mental health consumers, education of the media, and exhibitions of art by people with mental illness and other cultural activities (www.openthedoors.de). Another major German initiative is Irrsinnig Menschlich (engl. ‘Madly Human’), based in Leipzig. Here, too, various educational anti-stigma activities are undertaken, both locally and nationwide: These include the school project “Crazy? So what!” which raises students' awareness of mental health, and the international film workshop “Against the images in our heads”, a practical programme to reduce stigma and improve the lives of persons with mental illness (www.irrsinnig-menschlich.de). Other successful examples include the Like Minds, Like Mine Campaign in New Zealand (www.likeminds.govt.nz) that involves a vast number of local, regional and national initiatives, including active participation of persons with mental illness at all levels, and Sane Australia (www.sane.org), a nationwide anti-stigma campaign active for 20years and particularly successful in educating journalists and fighting stigmatising media messages.
In 1996, the World Psychiatric Association (WPA) started an international programme to fight the stigma and discrimination related to schizophrenia (www.openthedoors.com). Schizophrenia was chosen as the focus of this programme because it is a serious condition with symptoms that the public typically associates with mental illness, often of long duration. Rehabilitation of persons with schizophrenia is often hampered by stigma-associated difficulties Reference Sartorius[92]. The WPA-initiative tries to increase the awareness and knowledge of the nature of schizophrenia and treatment options, to improve public attitudes about individuals with schizophrenia and their families and to generate action to eliminate discrimination and prejudice.
Three main strategies have been used to fight stigma: protest, education, and contact Reference Corrigan and Penn[30].
5.1. Protest
Protest is often applied against stigmatizing public statements, media reports and advertisments. Many of these protest interventions have successfully changed such public statements. A German example is the above mentioned ‘BASTA – the alliance for mentally ill people’ that uses email to quickly alert members about stigmatizing advertisements or media messages. About 80% of the discriminating cases that BASTA took action against were successfully stopped and the respective companies or media institutions apologised. Usually, these campaigns were most effective if several actions coincided: if many people wrote to the public relations department and to the managing director or owner of the respective company or media institution; if BASTA turned to a national surveillance commission, e.g. one that was responsible for supervising advertising messages, and this commission supported BASTA's campaign; and if all these simultaneous activities and the responses of the respective company or media institution were documented on BASTA's website (Kerstin Wundsam, personal communication). There is evidence also from the US that these initiatives are effective in diminishing negative public images of mental illness Reference Wahl[103]. However, little is known about the effect of protest against people's prejudices. Social psychological research has found that protest leads to suppression of stereotypic thoughts and discriminating behavior. Unfortunately, there are two major problems with suppression. First, suppression is an effortful, resource-demanding process that reduces attentional resources, so that people are less likely to learn new information that would disconfirm the old stigmatizing stereotype Reference MacRae, Bodenhausen, Milne and Wheeler[70]. Second, there seems to be a rebound effect to suppressing minority group stereotypes. Subjects, asked to suppress thinking in a stereotypic way, after a while actually had more stigmatizing thoughts than before Reference MacRae, Bodenhausen, Milne and Jetten[69]. Thus, protest seems to be a useful way to reduce stigmatizing public images of mental illness. It may be less apt to change people's prejudices. As a reactive strategy, it may help to reduce stigmatizing public behavior, but it is likely to be less effective in promoting positive, new attitudes. However, effects of repeated protests on behavior should be further investigated. Furthermore, by reducing stigmatising public behaviour protest improves the quality of life for people with mental illness.
5.2. Education
Education tries to diminish stigma by providing contradictory information. Different forms like books, videos, and structured teaching programmes have been used to convey this kind of information. Brief educational courses on mental illness have proved to reduce stigmatizing attitudes among a wide variety of participants (police officers Reference Pinfold, Toulmin, Thornicroft, Huxley, Farmer and Graham[84]; industrial workers and government employees Reference Tanaka, Ogawa, Inadomi, Kikuchi and Ohta[100]; high school students Reference Esters, Cooker and Ittenbach[38]). However, research on educational campaigns suggests changes of behavior are often not assessed, effect sizes are limited, and programmes are more effective for participants who have a better knowledge of mental illness before the education or had contact with persons with mental illness beforehand. Thus, educational programmes tend to reach those that already agree with the message Reference Devine and Tesser[35]. Since stigmatising behaviors and attitudes are common among mental health care professionals Reference Gray[44], effective anti-stigma interventions for this group are important, but are, to our knowledge, rarely available so far and have not yet been evaluated.
It is further important to note that the content of education programmes seems to matter. Nowadays neurobiological models of mental illness are predominant in Western psychiatry. Therefore biological causes of schizophrenia, for example, are a main part of the message in educational programmes. The hope underlying this approach is that to view mental illness as a biochemical, mainly inherited problem will reduce shame and blame associated with it. On the other hand, the focus on neurobiology could, in the eyes of the public, turn people with mental illness into 'almost a different species' Reference Mehta and Farina[74]. The sense of separation between 'us' and 'them' could be increased by pointing out a genetic, unchangeable aetiology and the hope for recovery could be reduced. Mehta and Farina Reference Mehta and Farina[74] found describing mental illness in medical instead of psychosocial terms actually led to harsher behavior towards people with mental illness. A recent international study of public beliefs on causality of mental illness had similar results. Among over 7000 subjects interviewed in Germany, Russia and Mongolia, the view of schizophrenia as being of biological origin led to greater desire for social distance from persons with schizophrenia Reference Dietrich, Beck, Bujantugs, Kenzine, Matschinger and Angermeyer[37]. Given these findings and the complexities of interactions between genes and environment, the message of mental illness as being 'genetic' or 'neurological' may not only be overly simplistic but also of little use to reduce stigma Reference Phelan[82].
5.3. Contact
Contact with persons with mental illness may help to augment the effects of education on reducing stigma. Research has shown that members of the majority who have met minority group members are less likely to stigmatize against members of this minority [6,43]. Hence, contact may be an important strategy to decrease stereotypes and mental health stigma. Research shows that contact both during undergraduate training Reference Kolodziej and Johnson[55] and in an experimental situation Reference Desforges, Lord, Ramsey and Mason[34] reduced stigma and improved positive attitudes. In a number of interventions with secondary school students education and contact have been combined [8,84,94]. Results suggest that contact may be the more efficacious part of the intervention. Particularly interesting in this respect is an Austrian study that compared education without contact with a combination of both education and contact. A positive change of students’ attitudes was observed only when a consumer was involved in the intervention (contact and education Reference Meise, Sulzenbacher, Kemmler, Schmid, Rössler and Guenther[75]).
There are a number of factors that create an advantageous environment for interpersonal contact and stigma reduction. This includes equal status among participants, a cooperative interaction as well as institutional support for the contact initiative. For example, a school programme will be more successful if its efforts find support from the principal and if it allows for informal discussions between consumer and students instead of a consumer lecturing in front of a silent audience of students. Cooperation during work also offers a good opportunity to achieve equal status of consumers and members of the majority if both participate in the same task.
Also of importance are minority members who mildly disconfirm the stereotype towards this minority. Contact seems to be effective by changing stigmatizing knowledge structures. After contact, a person's natural stereotype of a minority group may be replaced by another, more positive image of that group Reference Rothbart and John[89]. For instance, after working with a person of equal status and with mental illness at one's new job, one may discard stereotypes about this person being dangerous or incompetent. The strength of the effect of change in stereotypes depends on the level of disconfirmation by the contacted minority group member. Contact experiences with persons who do not at all resemble stereotypes about the minority group are unlikely to have a major effect on those stereotypes Reference Kunda and Oleson[56]. For example, contact during work with a woman with mental illness who is also highly attractive and successful in her professional and personal life may not only fail to diminish stigma but even lead to a boomerang effect Reference Kunda and Oleson[57]. The information about this woman may not be used to disconfirm the stereotype about the minority of people with mental illness, but the woman will likely be subtyped as unusual. She may even be reclassified as belonging to 'us' instead of 'them' Reference Gaertner, Mann, Dovidio and Murrell[42]. This kind of subtyping can in fact corroborate stigma according to the saying that the exception proves the rule.
To sum up our overview of different methods to reduce stigma, contact combined with education seems to be the most promising avenue. To end on a more cautious note, though, one has to bear in mind a limitation of every anti-stigma initiative that focuses on a specific behavior of a certain group, e.g. local employers and their not offering jobs to persons with mental illness. On the one hand, prejudices and behavior of one group are an appealing target, because it reduces the complexity of the stigma-phenomenon and focuses on a target that matters Reference Corrigan[16]. On the other hand, the areas of individual discrimination, structural discrimination and self-stigma lead to innumerable mechanisms of stigmatization. If one discriminating mechanism is blocked, a powerful stigmatizing group can always create new ways to discriminate Reference Link and Phelan[63]. If for example persons with mental illness are protected by new work-legislation, employers can find new, informal ways not to employ or to fire them. Therefore, to substantially reduce discriminating behavior, stigma-related attitudes of power groups have to be fundamentally changed.
6. Conclusions
In this review we gave a conceptual overview of stigma, its main components - stereotypes, prejudice and discrimination - , and its consequences, focussing on self-stigma and empowerment and on fear of stigma as a barrier to use health services. We then discussed different avenues to reduce stigma and gave examples of anti-stigma initiatives. Since stigma is a complex phenomenon, much more research is needed on public stigma, self-stigma, the impact of stigma on families of persons with mental illness and on structural discrimination of persons with mental illness, especially inside the health care system. We also lack information on the different effects stigma has on persons with different mental disorders. It is unlikely that people with various disorders face the same stigmatizing attitudes and react to discrimination in the same way. While current anti-stigma initiatives certainly have a good intention, further empirical work is necessary to find out what strategy and content is best to reduce stigmatizing attitudes and behavior in what target group. We also still need to find out whether, in addition to public approaches, psychotherapeutic approaches might support people with mental illness to better cope with stigma until public stigma has been substantially diminished. In this context we also need more information on the relationship between stigma, emotions such as shame, and self-esteem.
Public stigma has a major impact on many people with mental illness, especially if it leads to self-stigma, and may interfere with various aspects of life, including work, housing, health care, social life and self-esteem. In order to support people with mental illness, successful long-term anti-stigma campaigns are necessary to reduce public stigma in society.
Acknowledgements
The authors are grateful to Christoph Nissen and Roland Zahn for their comments on an earlier draft of this paper.




Comments
No Comments have been published for this article.