Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Hoenke, Sophie
Serbian, Immo
Deigner, Hans-Peter
and
Csuk, René
2020.
Mitocanic Di- and Triterpenoid Rhodamine B Conjugates.
Molecules,
Vol. 25,
Issue. 22,
p.
5443.
Mansour, Shaimaa T.
Hashem, Ahmed I.
Abd‐El‐Maksoud, Mansoura A.
El‐Hussieny, Marwa
El‐Makawy, Aida I.
Abdel‐Aziem, Sekena H.
and
Soliman, Fouad M.
2022.
The synthesis and antineoplastic activities of thiaziridine, sulfidometylphosphonium, and dithiaphosphitane‐sulfide against the Ehrlich ascites carcinoma.
Fundamental & Clinical Pharmacology,
Vol. 36,
Issue. 3,
p.
536.
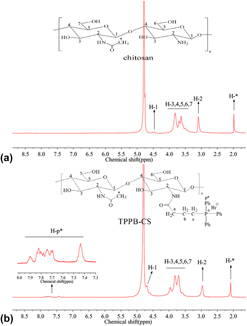
Arafa, Kholoud K.
Hamzawy, Mohamed A.
Mousa, Shaker A.
and
El-Sherbiny, Ibrahim M.
2022.
Mitochondria-targeted alginate/triphenylphosphonium-grafted-chitosan for treatment of hepatocellular carcinoma.
RSC Advances,
Vol. 12,
Issue. 34,
p.
21690.
Pashirova, T. N.
Nemtarev, A. V.
Souto, E. B.
and
Mironov, V. F.
2023.
Triarylphosphonium compounds as effective vectors for mitochondria-targeted delivery systems: decoration strategies and prospects for clinical application.
Russian Chemical Reviews,
Vol. 92,
Issue. 10,
p.
RCR5095.
Dahifale, Akanksha
Agnihotri, Tejas Girish
Jain, Ankit
and
Jain, Aakanchha
2024.
Quality-by-design-engineered mitochondrial targeted nanoparticles for glioblastoma therapy.
RSC Advances,
Vol. 14,
Issue. 46,
p.
34100.
Iskandar, Athirah
Kim, Se-Kwon
and
Wong, Tin Wui
2024.
“Drug-Free” chitosan nanoparticles as therapeutic for cancer treatment.
Polymer Reviews,
Vol. 64,
Issue. 3,
p.
818.
Batheja, Sanya
Gupta, Shruti
Tejavath, Kiran Kumar
and
Gupta, Umesh
2024.
TPP-based conjugates: potential targeting ligands.
Drug Discovery Today,
Vol. 29,
Issue. 6,
p.
103983.
Alfei, Silvana
Giannoni, Paolo
Signorello, Maria Grazia
Torazza, Carola
Zuccari, Guendalina
Athanassopoulos, Constantinos M.
Domenicotti, Cinzia
and
Marengo, Barbara
2024.
The Remarkable and Selective In Vitro Cytotoxicity of Synthesized Bola-Amphiphilic Nanovesicles on Etoposide-Sensitive and -Resistant Neuroblastoma Cells.
Nanomaterials,
Vol. 14,
Issue. 18,
p.
1505.
Alfei, Silvana
Zuccari, Guendalina
Athanassopoulos, Constantinos M.
Domenicotti, Cinzia
and
Marengo, Barbara
2024.
Strongly ROS-Correlated, Time-Dependent, and Selective Antiproliferative Effects of Synthesized Nano Vesicles on BRAF Mutant Melanoma Cells and Their Hyaluronic Acid-Based Hydrogel Formulation.
International Journal of Molecular Sciences,
Vol. 25,
Issue. 18,
p.
10071.