In the last 30 years, average BMI has increased annually by about 0·4 kg/m2 worldwide(Reference Finucane, Stevens and Cowan1); the increase has occurred primarily in developing countries along with an alarming rate of increase in overweight and obesity rates(Reference Prentice2–Reference Loret de Mola, Quispe and Valle4). Asian countries are now part of this global trend, where the continuing burden of undernutrition and the emerging problem of overnutrition have created a double burden of malnutrition(Reference Abdullah5–Reference Barquera, Pedroza-Tobias and Medina7). Bangladesh, like many emerging economies of South-East Asia, has started to experience a double burden of continuing high rates of undernutrition and increasing rates of overweight and obesity(Reference Khan and Talukder8,Reference Khanam, Lee and Ram9) .
Bangladesh has been fighting both poverty and undernourishment for a long time and has progressed towards being a low middle-income nation with decreased rates of undernutrition(Reference Nawaz10–Reference Das, Chisti and Malek14). The country has recently shown remarkable improvement in the public health sector, including the achievement of both Millennium Development Goal 4 and Millennium Development Goal 5 ahead of time(15,Reference Vos, Allen and Arora16) and striving to achieve the Sustainable Development Goals(Reference Arifeen, Hill and Ahsan17–Reference Akhter and Dasvarma19). This was facilitated by a consistent, more than 6·0 % annual rate of growth in gross domestic product along with the reduction of poverty by one-third in the last decade(Reference Islam, Khan and Islam20,Reference Gautam and Faruqee21) . The policies regarding nutritional status of women, particularly of mothers, are focused on undernutrition and underweight(Reference White22–Reference Belton, Mariana van Asseldonk and Thilsted24). However, a lack of assessment of the nutritional shift leaves a gap in current policies: the growing overweight and obesity is yet to be addressed(Reference Subramanian, Perkins and Ozaltin25–Reference Black, Victora and Walker27).
Low BMI has a significant association with preterm birth and other adverse birth outcomes. Women in developing countries generally face problems of underweight and undernourishment, to which poverty, food scarcity and illiteracy directly contribute(Reference Barrett28–Reference Headey31). Underweight (BMI < 18·50 kg/m2) during the reproductive age of women is associated with increased risk of low birth weight, preterm birth and intra-uterine growth restriction, as well as neonatal morbidity, mortality and growth failure(Reference Liu, Allen and Fraser32–Reference Khanam, Lee and Mitra35). However, an improvement in the nutritional status and a decreasing trend of underweight are evident in sub-Saharan Africa and South Asia(Reference Ahmed, Hossain and Sanin36,Reference Jaacks, Slining and Popkin37) . Microfinance programmes, growth in gross domestic product, better diet, accessibility to health care and increased female education have contributed to the positive nutritional shift in Bangladesh, which decreased rates of underweight status(Reference Headey31,Reference Ahmed, Mahfuz and Ireen38) .
Bangladesh is experiencing a new health problem of overweight and obesity, which are major risk factors for non-communicable diseases, especially diabetes and CVD, and are estimated to cause 3·8 % of the disability-adjusted life-years worldwide(Reference Ng, Zaghloul and Ali39–Reference Lavie, Schutter and Parto42). Rapid urbanization, decreased physical activity, change in lifestyle and change in dietary intake are the major contributors to this shift in low- and middle-income countries such as Bangladesh(Reference Basu, McKee and Galea43–Reference Kamal, Hassan and Alam46). A policy-based discussion was initiated by Khan and Talukder in 2013(Reference Khan and Talukder8) regarding the double burden of malnutrition in Bangladesh, where they identified the insufficient investment to address overweight and obesity in Bangladesh along with the lack of appropriate health policies.
The present paper investigates the change in nutritional status, particularly the shift in BMI, of Bangladeshi women of reproductive age (15–49 years). With the current policies focusing on undernutrition in rural areas, Bangladesh may have overlooked overweight and obesity, which is expected to be more prominent in urban affluent areas. Therefore the paper further assesses the gap between rural and urban nutritional status to characterize the vulnerable households for both underweight and overweight status for women in Bangladesh. The trend of BMI over a period of 10 years (2004–2014) was analysed using the last four rounds of Bangladesh Demographic and Health Surveys (BDHS) data. These should contribute to reassess the existing nutritional health policies in the region.
Materials and methods
Data description
The Demographic and Health Surveys (DHS) collect data from more than ninety low- and middle-income countries on the demographic and health characteristics of populations approximately at 5-year intervals(Reference Rutstein and Johnson47). The BDHS have been conducted among ever-married women of reproductive age (15–49 years) since 1993(15). These nationally representative cross-sectional surveys are conducted in collaboration with the National Institute of Population Research and Training, Bangladesh, ICF International, USA, and Mitra and Associates, Bangladesh.
Two-stage stratified cluster sampling techniques were adapted for sampling purposes in these surveys(15). The sampling frame for the survey was a complete list of enumeration areas from the most recent census, which were either a village (mouza in rural area and mohalla in urban area) or a part of a village or a group of villages. In the first stage of the sampling, the enumeration areas (clusters) were selected using the probability-proportional-to-size sampling method, where 600 clusters were selected in all the BDHS. In the second stage, an equal-probability systematic sampling method was applied to draw an average of thirty households from each selected cluster. The data for the current study were extracted from the BDHS conducted in 2004, 2007, 2011 and 2014. Only the data of the female respondents were considered; temporary residents (de jure v. de facto) and pregnant women were excluded from the analytic data set. Over 10 000 women were considered as the final sample size for each survey and they were merged together for the current study, constituting an overall sample of size 53 077.
Outcome variable
The present study applied the typical BMI categories constructed by the WHO: <18·50 kg/m2 = underweight, 18·50–24·99 kg/m2 = normal, ≥25·00–29·99 kg/m2 = overweight and ≥30·00 kg/m2 = obese(48). Continuous scaling of BMI at conservative form was used here to ensure all weight/height2 were captured. As the number of obese women was about 0·1 %, those obese were combined with the overweight category of BMI. While analysing the underweight level, a dichotomous variable of underweight v. others (normal/overweight/obese) was created. A similar process was followed for assessing overweight (BMI ≥ 25·00 kg/m2) v. others (normal/underweight).
The present paper discusses the disproportional burden of nutrition in two residencies: urban and rural. Although the variable ‘residency’ was taken from the BDHS, it should be noted that DHS surveys never define the urban–rural in a surveyed country, rather they use the country-specific administrative definition. According to the Bangladesh Bureau of Statistics, urban areas are comprised of ‘a central place having 5000 population with such amenities as metaled roads, improved communication, electricity, gas, water supply, sewerage, sanitation and also having comparatively higher density of population with majority population in non-agriculture occupations’(49). These includes cities, towns, Paurasavas (municipalities) and Cantonments.
Statistical analysis
BDHS provides a range of household-level sociodemographic factors. Four surveys from 2004 to 2014, each in an interval of 3 years, were used in the present study. An overview of the variables was conducted through frequency distribution (Table 1), where changes in sociodemographic factors over the years are displayed as well as the categories of BMI. Bivariate analysis between the BMI categories and sociodemographic factors was conducted. Their primary association was evaluated using the χ 2 test, which was adjusted for the complex survey design (survey weights and cluster-wise variation) using second-order Rao–Scott corrections(Reference Thomas and Decady50). To assess the trend of the nutritional burden, generalized linear mixed-effect models(Reference Rabe-Hesketh, Skrondal, Fitzmaurice, Davidian and Verbeke51) were applied, for both the underweight and the overweight variable. The time variable ‘year’ was considered as a covariate for assessing the trend.
Table 1 Frequency distribution of household sociodemographic characteristics and BMI of women of reproductive age (15–49 years, n 53 077), Bangladesh Demographic and Health Surveys (BDHS), 2004–2014
† Continuous variable.
The generalized linear mixed-effect models were fitted separately for urban and rural areas with year as their covariate (Tables 3 and 4). Each model was adjusted for age, parity, education, wealth index, division and marital status. The final model included urban and rural areas as a covariate. The sociodemographic factors were selected based on the previous studies that focused on the BMI of Bangladeshi women, particularly using the BDHS(Reference Balarajan and Villamor52–Reference Mohsena, Goto and Mascie-Taylor55). Age was a continuous variable, whereas parity (0, 1, 2, 3, ≥4), education (none, primary, secondary, higher), wealth index (poorest, poorer, middle, richer, richest), division (Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Sylhet), marital status (married, not married (i.e. divorced, widowed, separated, not living together)) and residence (urban, rural) were categorical variables. Rajshahi division was separated into two divisions (Rangpur and Rajshahi) in 2010. Hence, seven divisions were listed in BDHS 2011 and 2014. However, we merged these two into one division (Rajshahi) in the combined data set to be consistent with BDHS 2004 and 2007. The DHS created a household wealth index with five groups corresponding to poorest, poorer, middle, richer and richest from the reported households’ asset variables using principal component analysis(Reference Howe, Hargreaves and Gabrysch56).
Ethical approval
The present paper does not contain any studies with human participants performed by any of the authors. The Bangladesh Medical Research Council and the Institutional Review Boards of ICF International approved the BDHS protocols, questionnaires and verbal consent forms for the respective years. All respondents were de-identified before publishing the data. The secondary data sets analysed during the current study are freely available upon request from the DHS website (https://dhsprogram.com/data/available-datasets.cfm).
Results
Over the 10-year study period, the proportion of overweight women increased and the proportion of underweight women decreased (Fig. 1). The percentage of overweight increased during 2004–2014 from 10·7 to 25·1 % (Table 1). In that period, the underweight percentage decreased almost by half, from 32·6 to 18·2 %.
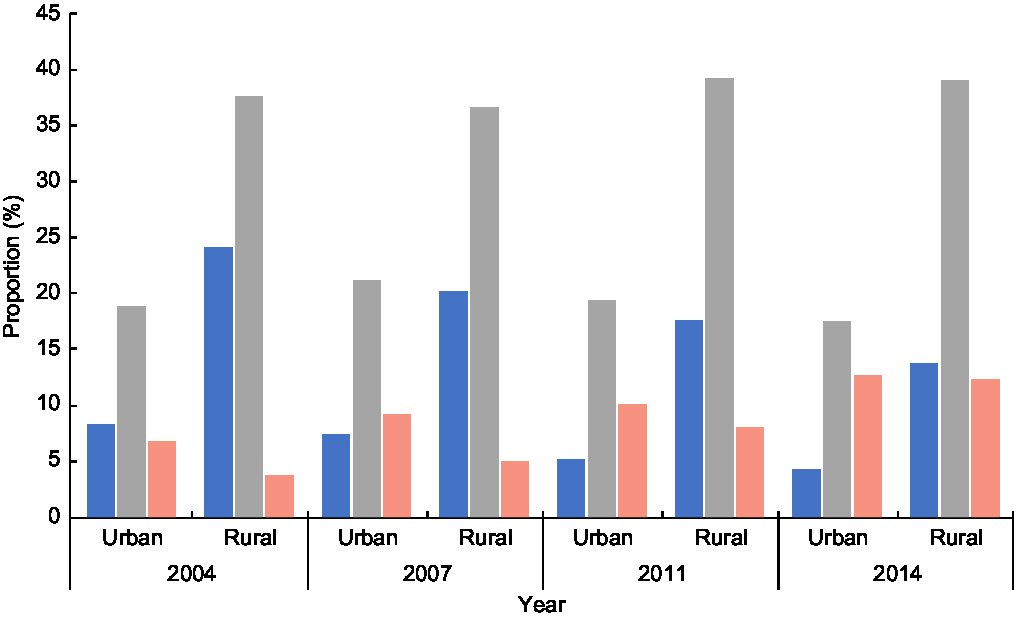
Fig. 1 The proportion of underweight (![]() ), normal (
), normal (![]() ) and overweight (
) and overweight (![]() ), by urban–rural residence and year, among women of reproductive age (15–49 years, n 53 077), Bangladesh Demographic and Health Surveys, 2004–2014
), by urban–rural residence and year, among women of reproductive age (15–49 years, n 53 077), Bangladesh Demographic and Health Surveys, 2004–2014
The average age of women in the last four surveys were similar, about 31 years (Table 1). Households with one or two children increased, whereas those with four or more children decreased. The proportion of ‘not married’ women in the four samples was 6–8 % and the major portion of each sample (approximately 60 %) was from rural areas. The percentage of uneducated women decreased from 40·1 % (2004) to 24·5 % (2014). As the wealth index was a simulated variable that classified household possessions into five levels, its values were proportionally equal for each survey.
The proportion of underweight women was much lower and the proportion of overweight women was nearly six times higher for the richest households (38·1 %) than the poorest households (5·9 %; Table 2). Only about 9 % of highly educated women were underweight compared with 32·3 % of uneducated women. In contrast, only about 11 % of the women with no education were overweight, whereas 38·8 % of the highly educated women were overweight in the combined sample. The highest percentages of overweight women were in Dhaka and Khulna divisions and the highest proportion of underweight women was from Sylhet division. Only 12·5 % of residents in the rural areas were overweight compared with 28·8 % in the urban areas. All of the categorical variables showed a significant association with underweight and overweight categories in the bivariate analysis χ 2 test (Table 2).
Table 2 Bivariate analysis of BMI category by household sociodemographic characteristics of women of reproductive age (15–49 years, n 53 077) in four combined Bangladesh Demographic and Health Surveys, 2004–2014
† P value of the χ 2 test between BMI and sociodemographic factors after adjusting the complex survey design (survey weights and cluster-wise variation) using second-order Rao–Scott corrections.
‡ Continuous variable.
The generalized linear mixed-effect model fitted to the underweight category compared with the other BMI categories in both urban and rural areas showed a significant (P < 0·01) trend over the years. In comparison to 2004, women living in urban areas of Bangladesh had 54 % less chance of being underweight in 2014, when adjusted for other covariates (Table 3). In the combined model, where both urban and rural residents were studied, we reached a similar conclusion with women becoming less prone to underweight as the years have gone by. Age, education, wealth index, division and marital status showed a significant association with women’s underweight status. Highly educated women were half as likely to be underweight compared with the illiterate, and women belonging to the richest class had 75 % less chance of being underweight compared with those in the poorest households. Compared with Barisal division, women in Sylhet were 1·4 times more likely to be underweight in both urban and rural areas. As per Table 3, there was hardly any difference between urban and rural areas in the magnitude of trend in their underweight status. However, the combined model found that the urban women were 17 % less likely to be underweight than the rural residents.
Table 3 Binary generalized linear mixed-effect models for the association of underweight (v. normal/overweight/obese; reference) with household sociodemographic characteristics, according to urban–rural residence and overall, among women of reproductive age (15–49 years, n 53 077), Bangladesh Demographic and Health Surveys, 2004–2014
Ref., reference category.
* OR and 95 % CI significant at 1 %.
† Age (15–49 years) was scaled (min = 0, mean = 0·5, max = 1) in the model convergence.
The trend in the overweight category was different for urban and rural areas (Table 4). In the urban model, the urban residents were over 2·4 times more likely to be overweight in 2014 compared with 2004. However, the magnitude of change in odds was higher in rural areas, as the women living there were over 3·9 times more likely to be overweight in 2014 compared with 2004 (rural model, Table 4). This indicates that the extent of nutritional shift was greater for rural residents. Age, parity, education, wealth index and marital status played a significant role in these models. The highly educated women were 2·35 (urban) and 1·75 times (rural) more likely to be overweight in 2014 compared with 2004. Similarly, the wealthier the household, the more likely (OR = 7·25 for urban and OR = 5·66 for rural) that a woman from that household would be overweight compared with those from the poorer quintiles. The non-married (e.g. divorced, widowed or separated) women were less likely to be overweight in reference to the married women. Although the volume of shift was higher for the rural women, the urban residents still showed 50 % more chance of being overweight, compared with the rural women, in 2014 v. 2004 (combined model, Table 4).
Table 4 Binary generalized linear mixed-effect models for the association of overweight/obesity (v. normal/underweight; reference) with household sociodemographic characteristics, according to urban/rural residence and overall, among women of reproductive age (15–49 years, n 53 077), Bangladesh Demographic and Health Surveys, 2004–2014
Ref., reference category.
* OR and 95 % CI significant at 1 %.
† Age (15–49 years) was scaled (min = 0, mean = 0·5, max = 1) in the model convergence.
Discussion
The current study demonstrates that there has been a substantial change in the BMI status of reproductive-age women in Bangladesh. Between 2004 and 2014, there was a 15 % increase in the prevalence of overweight status and a similar decrease in underweight status. The reduction in underweight status was of similar magnitude in both urban and rural areas; whereas there was a greater relative change in overweight status in the rural areas, which is congruent with recent review findings(57). The underweight prevalence in rural areas remained relatively high, as did the overweight prevalence in the urban residents. These findings of the shift of nutritional burden are an extension of previous findings depicting consistency with literature from Bangladesh(Reference Balarajan and Villamor52,Reference Khan and Kraemer58,Reference Hoque, Hasan and Rahman59) . Apart from the year-wise change and variation by urban–rural residence, the current study also finds that education, family income level, marital status of the women and geographic divisional locations played significant roles in the double burden emergence in Bangladesh.
Women’s level of education was a significant predictor of nutritional shift. The higher rate of overweight in women with higher education is presumably because these women are more likely to be in sedentary jobs with less physically intensive activities such as construction works(Reference Balarajan and Villamor52). Occupational sitting time is high for educated persons, who prefer desk jobs, which in turn increases the risk of overweight and obesity(Reference Mummery, Schofield and Steele60). On the other hand, the economic activities of illiterate women, who generally do not have adequate technical skills, are mostly confined to labour-intensive work(Reference Kabeer, Mahmud and Tasneem61,Reference Kumar, Hossain and Gope62) . However, the BDHS provides neither the daily physical activity counts of the respondents nor sitting times. Another possible explanation could be that the educated women have less time to prepare home-cooked meals and tend to use the more convenient options (processed foods) that could lead to increased weight(Reference Schmidhuber and Shetty63,Reference Baker and Friel64) . In the study period (2004–2014), the findings suggest that the secondary or higher educated women were over 1·5 times more likely to be overweight, whereas only 10·5 % of the illiterate women were overweight (Table 4).
Economic solvency affected the shift of BMI scales from underweight to overweight in Bangladesh as purchasing capacity of the general mass increased. The poor uneducated were mostly undernourished, while the rich educated were overweight. This leads to the assumption that women living in well-off families had access to surplus income and consequently increased their intake of nutritious (and/or processed) foods, whereas poor families could not afford them and remained underweight and undernourished(Reference Das, Fahim and Islam65). Another possibility in the urban setting could be the overconsumption of fast (or junk) foods, which are more accessible to the wealthier sections of society, that brings a change in the traditional dietary intake that elevates weight in general(Reference Rahman66,Reference Morgan and Sonnino67) . Thus, from the surveys between 2004 and 2014, it can be observed that 73 % of the overweight women were from above middle wealth quintiles.
From the divisional variation, it is eminent that underweight status increased significantly only in Sylhet compared with Barisal, and in other divisions the overall BMI increased with a significant decrease in underweight status. These divisions also experienced an increase in overweight status compared with Barisal division. This could be explained by the educational status and income of households, as Sylhet division lags behind in education and Barisal in economy(Reference Islam, Angeles and Mahbub68–Reference Tareque, Begum and Saito70). Marital status in all models showed that women, who were not living with their partners and were divorced, seemed to be leaning towards underweight compared with currently married women. This could be because childbirth leads to gain of weight (parity in Tables 3 and 4) and married women are less likely to care about their weight increase(Reference Kutob, Yuan and Wertheim71–Reference Chowdhury, Adnan and Hassan73). One other possibility could be that single women are relatively more economically disadvantaged than married ones where the husband contributes to income.
Urbanization creates a fast-paced economic paradigm where population density increases and food consumption follows the global trend, which currently refers to processed foods or ‘western’ diets more often filled with fats and refined carbohydrates(Reference Schmidhuber and Shetty63,Reference Popkin74,Reference Neiderud75) . In the current context of Bangladesh, various restaurants, food parks and supermarkets are gaining popularity in the urban areas, serving as places for recreational family activities, further fuelled by media publicity(Reference Harun, Ahmed and Maniruzzaman76,Reference Ashraf, Akhter and Noor77) . This changes the everyday food intake of the urban residents. Moreover, with continuous urban migration towards already crammed cities, increased housing and infrastructures have dried up the open spaces, which eventually results in an opportunity cost for the residents’ physical activities(Reference Reardon, Boughton and Tschirley78–Reference Melby, Orozco and Ochoa80). Thus, outdoor activity-based recreations are replaced by home-based entertainments (e.g. televisions, computers, board games), which ultimately lead to increased sitting time(Reference Goryakin and Suhrcke81). These could explain why the current study finds that, compared with rural residents, more than twice the proportion of overweight women were urban residents in Bangladesh.
Bangladesh has recently been classified as a low middle-income country following strong growth rate in gross domestic product in recent times, and it aims to become a middle-income country by 2021(Reference Feldman82,83) . In the process of economic development, Bangladesh has shown commendable success in the public health sector, including rapid reduction of undernutrition(Reference Taylor84,Reference Headey, Hoddinott and Ali85) . Bangladesh’s Integrated Nutrition Program 1995–2004 and the subsequent National Nutritional Program had debatable, limited impact on existing nutritional status(Reference Hossain, Duffield and Taylor86–Reference Sack, Roy and Ahmed89). However, foreign investment paired with the efforts of local non-governmental organizations has improved maternal health care, which has reduced the underweight and undernutrition scenario in distant corners of Bangladesh, decentralizing the health benefits(Reference Headey, Hoddinott and Ali85,Reference Islam90,Reference Hasan, Soares Magalhaes and Williams91) . The findings of the present study support that the proportion of underweight women of reproductive age has declined over the last decade, even in the rural areas, to which growth in household economic status and increased female education have contributed.
This observed growth in gross domestic product was found to be associated with the double burden of malnutrition in recent literature, both in Asia and worldwide(Reference Gillespie and Haddad92,Reference Kraak, Swinburn and Lawrence93) . Economic growth has reached the rural areas with much developed road infrastructure and that brought application of commercial products for agriculture and day-to-day household tasks(57). This has led to a decreased need for manual labour and with the additional availability of processed carbohydrates all over the country, to higher energy intake(Reference Reardon, Timmer and Barrett94,Reference Reardon, Timmer and Minten95) . Although our discussion is focused on urban and rural differences, previous studies on nutrition in Bangladesh have found differences between adult men and women(Reference Hoque, Hasan and Rahman59). It has already been observed that such double burden is affecting children (e.g. stunting) in low- and middle-income countries(Reference Tzioumis, Kay and Bentley96). Thus, economic development demands a revisit to the existing nutritional policies to address the double burden of malnutrition.
While the current health policies focusing on nutrition generally emphasize the cases of undernutrition and underweight, multifaceted national policies from evidence-based experimental interventions are required to address the double nutritional burden(Reference Headey, Hoddinott and Ali85,Reference Motlagh, Kelishadi and Amirkhani97) . Similarly, the UN Decade of Action on Nutrition has already addressed the double burden as an emerging problem worldwide and called for cross-cutting and coherent policies and programmes(Reference Demaio and Branca98). Such intervention strategies are tricky given that both ends of the nutritional spectrum are affected by the same covariates with a varied range. For example, the wealth index was found to be a significant factor for both nutrition statuses; however, the richest households are more likely to be overweight and poor households tend to be underweight. As a part of the UN Decade of Action on Nutrition, in 2016 the WHO suggested six areas of policy action including promoting sustainable diets by encouraging local production, setting up social protection programmes with awareness campaigns, and applying national cross-government, multisectoral, multi-stakeholder mechanisms to incorporate international guidelines on healthy diets in local communities(99). However, all these would require intervention pilot studies in the context of Bangladesh prior to national policy implementation.
There were some limitations to the present study. First, there is no particular set of BMI levels for women in Bangladesh, which undermines the proper weight/height quantification as BMI tends to vary with a number of factors: racial group, ethnicity, geographic location, gender, age, hormone levels and other socio-economic measures(Reference Gray, Yates and Davies100–Reference Bahat, Tufan and Saka102). More importantly, the typical threshold for overweight (≥25·00 kg/m2) might underestimate the current problem of overnutrition in Bangladesh(Reference Razak, Anand and Shannon103). This could be one of the reasons why we found only 0·1 % of obese women in the study period. Second, the study was limited to females in their reproductive age. Hence, generalization of the results and interpretation of the findings must be cautiously done. Third, respondents’ food intake, physical condition and sitting time, as well as national-level factors such as food prices and quality of nutrition are important components while analysing nutritional status, which were not available in BDHS data sets. Fourth, the sample size varied across the data sets over the years, which might compromise the interpretation across surveys; however, consistent methodologies were followed in all the surveys. Finally, the trend analysis would be more substantial with longitudinal data, particularly if the same respondents could be followed from rural–urban migration to assess their changes. Future studies could consider these issues and adjust the models for further precise findings.
Conclusions
Bangladesh is transitioning from a low-income to a middle-income country, and its sociodemographic changes are influencing the public health sector. Generally, in Bangladesh, the primary concern for maternal health has been undernourishment and underweight. However, the current study argues that the nutrition scale is shifting; overall, the prevalence of underweight status is decreasing and there has been a consequent increase of overweight status. Prevalence of underweight status has remained high in the rural areas and the prevalence of overweight is increasing rapidly in both rural and urban areas. The significant contributors to this double burden were the change in women’s level of education, increased household wealth, divisional location and rapid urbanization. Women with higher education from well-off families living in urban areas seem to be overweight, whereas uneducated women from poor households residing in the rural areas are underweight. To characterize these changes in the context of Bangladesh, health policies focusing only on undernutrition need to be revised and consider the new double burden. Revised policies, however, would require application of multiple area-based intervention studies in line with the UN Decade of Action on Nutrition to address the double nutritional burden in Bangladesh.
Acknowledgements
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: There is no conflict of interest among the authors. Authorship: R.K.B. conceptualized the study, compiled the data, synthesized the analysis plan and drafted the manuscript. N.R. conducted the statistical analysis and interpreted the findings. R.K. and A.H.B. provided expert opinions and critically reviewed the manuscript. S.A. overviewed the statistical analysis and revised the manuscript. All authors read and approved the manuscript. Ethics of human subject participation: This article does not contain any studies with human participants performed by any of the authors. The Bangladesh Medical Research Council and the Institutional Review Boards of ICF International approved the BDHS protocols, questionnaires and verbal consent forms for the respective years. All respondents were de-identified before publishing the data. The secondary data sets analysed during the current study are freely available upon request from the DHS website (https://dhsprogram.com/data/available-datasets.cfm).







