Introduction
Inadequate nutrient intakes are recognised as a key immediate cause of maternal and child undernutrition, exacerbated by poor child feeding practices, household food security, and unhealthy environmental factors.(1) This manifests over time as malnutrition and nutrient deficiencies, and is intensified in population groups with higher nutrient requirements, such as breastfeeding women who require more nutrients for their own body functioning, for milk production, and to ensure adequate breastmilk nutrient content to meet their infant’s needs.(2,Reference Allen3) Inadequacies in iron and zinc intake can lead to anaemia in both breastfeeding women and breastfed infants, while inadequate thiamine can lead to motor and cognitive impairment or infantile beriberi in infants.(Reference Smith and Hess4)
Women of reproductive age (WRA) living in Cambodia, a low-middle income country (LMIC), continue to show evidence of poor nutritional status as a result of food insecurity, poor hygiene and inadequate health services.(5) A double burden of malnutrition is increasingly evident in Cambodian WRA, with declining prevalence of underweight (7%) and a rapidly increasing overweight and obese rate (from 6% in 2000 to 33% in 2021)(6) coexisting with micronutrient deficiencies.(Reference Hasan, Ahmed and Magalhaes7,8) Anaemia prevalence has consistently remained high at 45% for WRA and 52% for breastfeeding women,(8) despite targeted iron supplement and iron awareness initiatives.(Reference Lacerte, Pradipasen and Temcharoen9,Reference Cavalli-Sforza10) In 2014, 19% of Cambodian women with young children were found to have folic acid deficiency.(8) The prevalence of some micronutrient deficiencies differs by locality, with significantly higher proportions of rural WRA having anaemia compared to urban (47% vs. 39%; P < 0.0001), and vitamin D deficiency (61% rural vs. 52% urban; P < 0.0001).(8) Reported vitamin A deficiency is relatively low in both rural and urban women (9% vs. 10%).(8)
There are no specific nutrient reference values (NRV) for Cambodian adults. Only 11 Cambodian studies have used nutrient standards,(Reference Windus, Burrows and Duncanson11) either Recommended Nutrient Intakes from the World Health Organization (WHO),(12) Recommended Dietary Allowances for Southeast Asia,(13) or Estimated Average Requirements (EAR) from the Institute of Medicine (IOM).(2) It is recommended that the EAR cut-point method be used to estimate population-level nutrient adequacy,(Reference Gibson14,Reference Allen, Carriquiry and Murphy15) as a shortcut derived from the probability approach that estimates the proportion of a group at risk of inadequate nutrient intakes based on usual intake.(2,Reference Gibson14)
Dietary adequacy is assessed using dietary intake data to identify individual nutrient, food groups or dietary pattern adequacy.(16) A review of dietary assessment studies conducted in Cambodia identified 48 studies with women and children under five years,(Reference Windus, Burrows and Duncanson11) however only three studies involved an individual-level ‘whole diet’ assessment that reported nutrient intakes among adult women.(6,Reference Windus, Duncanson and Burrows17–Reference Bunthang, Nam and Phen19) Studies by Verbowski et al. (2018)(Reference Verbowski, Talukder and Hou18) and Bunthang et al. (2014)(Reference Bunthang, Nam and Phen19) conducted with Cambodian women used single 24-hour recalls and the ASEAN food composition database,(20) but different food record methods, adequacy measures and quality checks. These studies reported that dietary intakes were inadequate for calcium, zinc and vitamin A, whereas iron adequacy differed between the two studies.(Reference Windus, Duncanson and Burrows17–Reference Bunthang, Nam and Phen19) However, these studies were conducted exclusively in rural locations 10 years ago, so may not reflect more recent changes in food availability and consumption driven by economic growth, particularly in urban Cambodia.
The most recent Cambodian demographics and health survey(6) collected dietary intakes via list-based 24-hour recall reporting that higher proportions of urban women consumed items from all dietary diversity food groups compared to rural women. This is consistent with the reported poorer nutritional status of rural Cambodians(8,Reference Horiuchi, Kusama and Kanha21) and reflects similar dietary intake patterns between rural and urban WRA evident in other LMICs (South-east Asia(Reference Lipoeto, Lin and Angeles-Agdeppa22); Lesotho(Reference Rothman, Ranneileng and Nel23); Indonesia(Reference Kosaka, Suda and Gunawan24)). However, no dietary assessment studies to date have reported on nutrient intake and adequacy among breastfeeding (BF) women in Cambodia compared to non-breastfeeding (NBF) women.
The primary aim of this study was to quantify adequacy of nutrient intakes of Cambodian women living in Siem Reap province and compare adequacy by breastfeeding status. The secondary aim was to evaluate differences in nutrient adequacy between rural, semi-rural and urban settings.
Methods
This cross-sectional study quantified nutrient intakes of women in rural, urban and semi-rural areas of Siem Reap province in Cambodia, using image-voice technology. The STROBE-nut checklist informed the reporting of this dietary assessment study (Supplementary Table 1).(Reference Lachat, Hawwash and Ocke25) This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the National Ethics Committee for Health Research in Cambodia (Ref No. 151 NECHR), University of Newcastle (Ref H-2018-0515) and Curtin University (HRE2022-0366) Human Research Ethics Committees in Australia. Verbal informed consent was obtained from all participants to participate in the study and use their data for publication, which was witnessed and formally recorded.
VISIDA project
This study used the Voice-Image Solution for Individual Dietary Assessment (VISIDA) system, consisting of image and voice technologies developed for collecting and analysing individual-level dietary intake data in LMIC.(Reference Rollo, Windus and Stewart26,Reference Saronga, Mosha and Stewart27) A validation paper of the VISIDA system(Reference Rollo, Windus and Stewart26) described the methodology in detail, which is summarised below.
A smartphone application (app) was developed so participants could actively capture both an image and voice recording of a meal, drink or snack at time of consumption. Recipes for mixed dishes were created by capturing images and voice recordings of ingredient quantities and cooking methods. Breastfeeding occasions were also captured using a count feature in the app. Household members were accounted for in the app, with each food or drink item identified as an ‘own plate’ for discrete consumption or a ‘shared plate’ for communal eating, allowing for individual volume quantification. Leftovers were accounted for within the app to ensure an accurate representation of actual intake.
The relative validity of this image-voice method was determined through comparing against three 24-hour recalls, where dietary intakes captured using VISIDA were found to be generally lower than 24-hour recalls, while being consistent across both VISIDA data collection periods.(Reference Rollo, Windus and Stewart26)
Fieldwork
The project fieldwork was conducted through the collaboration between University of Newcastle, Australia and ‘This Life Cambodia’, a local non-government organisation (NGO) based in Siem Reap city, experienced in research and programme assessment. This NGO was commissioned for in-country coordination, participant recruitment and management, data collection and data processing. Weekly Zoom planning meetings and three weeks of in-depth face-to-face training sessions were conducted to upskill eight research assistants (RA) on dietary assessment methods, anthropometry, the VISIDA system, research protocols, participant training and management systems. Each questionnaire was translated from English to Khmer by NGO staff, and checked by a second dual-language reviewer.
Setting and participants
Cambodian women were recruited from rural (Svay Sor; 100 km from the city), semi-rural (Sra-ngae; 8 km from the city) or urban (Siem Reap city) locations in Siem Reap province, in Cambodia’s north-west region. As the sample were not required to represent the national population, recruitment was based on nonprobability purposive sampling, which took place from August 2019 to March 2020, spanning both wet and dry seasons.
Eligible participants were non-pregnant women ≥18 years of age with at least one child under five years. There were no requirements regarding previous smartphone experience, breastfeeding status or whether their child had commenced eating solids. The recruitment target for the study was 150 families, consisting of 50 families per location, a pragmatic and appropriate sample size for assessing the reliability and validity of novel technology in an under-researched population. A commune leader in each location was approached by the NGO’s senior staff member to obtain permission and gain support for inviting community members to an initial research information session. RAs presented participants information in verbal, written and pictorial forms. Verbal consent from eligible women was obtained using a voice recording. Consented participants were also asked to suggest names of other eligible friends and family who may be interested in participating.
Data collection
Demographics: Following enrolment, participating women completed a demographic questionnaire to collect data on age, occupation (primary and secondary), self-reported breastfeeding status, level of education, number of children and nutritional supplement use.
Anthropometrics: RAs collected anthropometric data in duplicate for each participating woman and their child, measuring weight, height and mid-upper arm circumference with portable equipment (Seca-869 standing scales, InBody BSM370 stadiometer), following standardised protocols.
Dietary intake data: RAs trained women to use the VISIDA image-voice food record app on the test day, then observed participants using the app over two eating occasions in their home to monitor technique and provide feedback as required. Participants then used the app to collect an image and voice recording for every food and beverage item consumed during each designated data collection day. A schedule was created for each mother, ensuring three collection days were non-consecutive and included one weekend day, over two collection time periods separated by approximately two weeks. A built-in ‘end-of-day review’ feature on the app ensured a full day’s data was collected. After the month-long study, each participant was remunerated for their involvement (USD5 per collection day).
Cambodian food composition database development
As Cambodia does not have a comprehensive food composition database (FCD), prior to commencing this study the VISIDA research team compiled one using a systematic, stepwise approach recommended by Food and Agriculture Organization’s International Network of Food Data Systems (INFOODS).(28) Food and beverage items regularly consumed in Cambodia were identified through observation and consultation with local women. Items were compiled from ten established international FCD, primarily the FCDs of South-East Asian SMILING (2013)(Reference Sok29) and ASEAN (2014),(20) supplemented by FCDs from Australia, United States, Vietnam, Japan, Bangladesh and Laos. As many commonly consumed items, particularly Khmer-style mixed dishes, were not found in established FCDs these were sourced from Cambodian recipe books, online recipes and directly from Cambodian women. Recipe calculations were applied to account for retention and yield factors. The final Cambodian FCD comprised of 1099 items with complete data for energy and 23 nutrients, which when uploaded into the VISIDA content management system (CMS) provided the nutrient composition for data coding.
Data coding
Following each dietary collection day, an RA conducted a data quality check with the participant for completeness of dietary data, then downloaded the data from the app. This data was then uploaded into a web-based CMS purpose-designed for identifying and quantifying. Tools embedded in the CMS to aid the data coding process included the Cambodian FCD for item identification, a measures database, and reference images with known weights to aid item quantification.
Local RAs identified each food or drink item from images and accompanying voice recordings in the CMS. Item identification was checked by a second Khmer-speaking reviewer (JW). Three Research Dietitians (JW, MR, SS) trained in food quantification techniques estimated item quantities based on the images and translated voice recording, using the CMS embedded tools as required. Two dietitians independently estimated quantities of each item to the nearest gram, each blinded to the other’s estimate. The final quantity was determined by averaging the estimates with <25% difference. For differences ≥25%, a third independent reviewer made the final estimation.
Data analysis
Data cleaning involved removing extra days collected outside the schedule and removing data for participants who collected less than the required minimum of two day’s intake. Under- and over- reporting were assessed by considering the implausibility of extremely high or low energy intakes of participants based on two standard deviations from the mean energy intake for total participants, then assessing the data by removing three outliers to find negligible difference in intakes, and recognising from our observation of Cambodian women and assessments made by other LMIC studies that very low intakes could be considered as being plausible in an LMIC context.(Reference Verbowski, Talukder and Hou18,Reference Loy, Marhazlina and Nor30) Nutrient intake data were downloaded from the CMS into Microsoft Excel then uploaded into SPSS (27.0)(31) for analysis.
The EAR reflects the average daily nutrient intake amount estimated to meet requirements for half of the specified population group.(Reference Allen, Carriquiry and Murphy15) The EAR cut-point method was used to estimate the proportion of participants with nutrient intakes likely to be adequate, identified by the percentage equal to and above the EAR for each nutrient. Two EAR values from IOM(2) were used; participants who self-reported as breastfeeding (BF) were compared against ‘Lactation’ (hereafter referred to as ‘breastfeeding’) values, and non-breastfeeding (NBF) participants were compared against ‘Females 19–50 years’ values. The prevalence of nutrient inadequacy for each respective life stage group is approximated by the proportion with intakes below the EAR.(2) Each participant’s protein EAR was calculated based on grams per kilogram body weight. Energy intake was compared to IOM’s estimated energy requirement equation using mean age, weight and height for BF or NBF women groups, respectively, and a ‘low active’ physical activity level factor of 1.12(32) reflecting their regular household manual tasks of daily living.
Of the 26 nutrients in the Cambodian-FCD, EARs were available for 14, namely protein, carbohydrate, vitamin A (retinol equivalent), vitamin C, thiamine, riboflavin, niacin, vitamin B6, vitamin B12, folate, calcium, zinc, iron and phosphorus.(32–34) Sodium and potassium have no established EAR, so their Adequate Intake (AI) values were used for estimating adequate intake, acknowledging that the AI cannot be used to indicate inadequate intakes.(2) Similarly, fat has no NRV or EAR, however was included to assess total fat intake and its contribution to energy intake. A total of 17 nutrients and total energy (kJ) were included in the analysis. Tolerable upper intake limits were also assessed for six minerals.(2)
Statistical analysis
Descriptive statistical analysis of nutrient intakes and adequacy was conducted in SPSS version 27.0.(31) Demographic data were summarised by frequency and proportions of total, BF and NBF samples. Non-parametric independent median samples significance testing (P < 0.05) was applied to medians of nutrient intakes in SPSS.(31) For adequacy, Pearson’s chi-squared tested statistical significance between proportions (P < 0.05), comparing between BF and NBF women, locations, and younger versus older women.
Nutrient medians and adequate intake proportions were compared by breastfeeding status, location, first or second recording period, age groups and body mass index (BMI).
Results
Of the 148 households recruited, data were collected from 119 Cambodian women (Fig. 1). Overall, 14 women were lost to follow up for reasons such as work, sickness or opted to discontinue. Nine participants were withdrawn early from semi-rural location due to the Covid-19 pandemic declaration in March 2020; four due to poor protocol compliance; and two recorded only one day’s intake. No participants were excluded for under- or over-reporting as all energy intakes were considered plausible for women living in a LMIC.
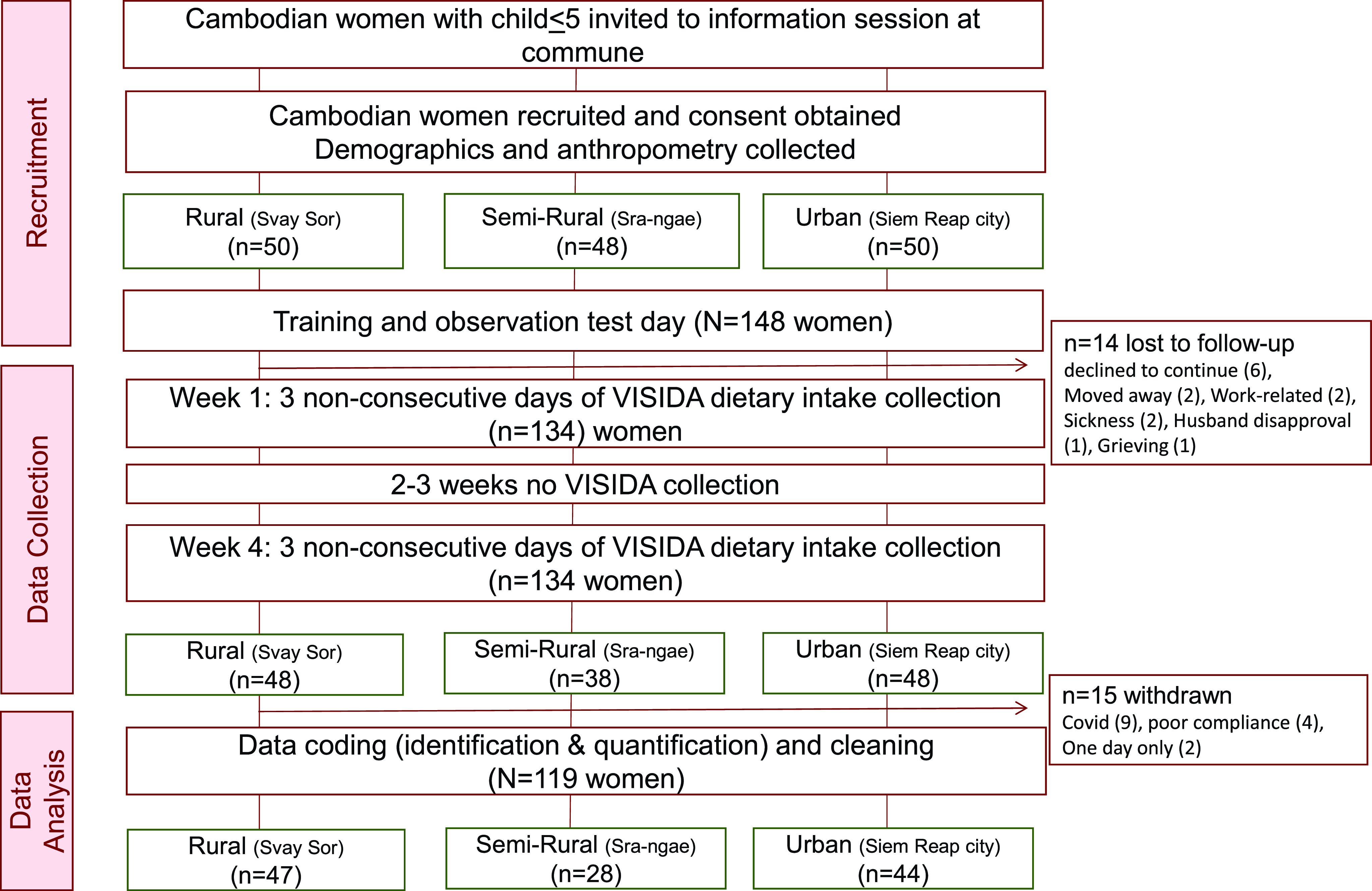
Fig. 1. Participant flow diagram of recruitment, data collection, and analysis for Voice-Image Solution for Individual Dietary Assessment (VISIDA) study conducted in Siem Reap province, Cambodia.
The first recording period represented 51% of collection days, and the second 49%, with seven not participating in the second recording period. Most (94%) participants recorded five or six days of intake. Participant characteristics are shown in Table 1.
Table 1. Participant characteristics of Voice-Image Solution for Individual Dietary Assessment study in Cambodia, by total, breastfeeding, and non-breastfeeding mothers
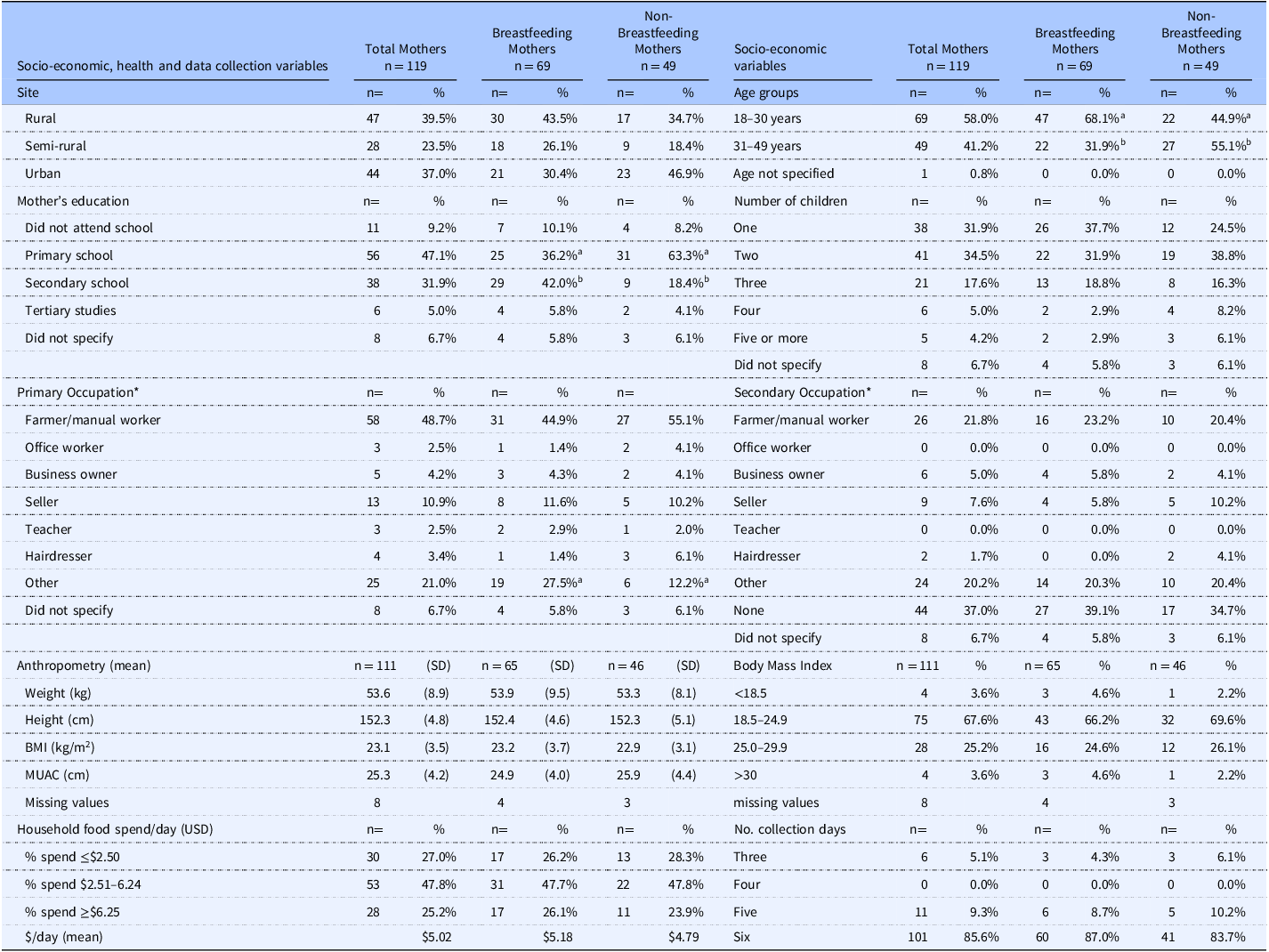
SD, standard deviation. 1Proportions % indicated per population group (column). Statistically significant differences between breastfeeding and non-breastfeeding mothers are indicated by superscripts (a,b) along rows. *Proportion z-score significance tests performed for occupation grouped non-farmer/manual worker (i.e. office, business owner, seller, teacher, hairdresser); P = 0.549 for primary occupation, and P = 0.303 for secondary occupation.
Fifty-eight percent of participants reported they were breastfeeding. Thirty-nine percent lived in a rural area, 37% in Siem Reap urban centre, with 24% from a semi-rural locality. Nearly two-thirds of rural women were breastfeeding (64% rural vs. 48% urban; P = 0.121).
Participants had a mean age of 28.8 (6.0) years, with BF women significantly younger than NBF women (27.4 vs. 30.8 years; P = 0.002). Two-thirds of women were in the healthy weight range (BMI 18.5 to 24.9 kg/m2) with no significant differences in weight, height, or middle-upper arm circumference between BF and NBF women.
Almost half (n = 58) the women were from a household whose primary occupation was reported as farming or manual labour, (64% rural vs. 27% urban, P = 0.001), and over one-third indicated having no secondary occupation. While most women had attended school, two-thirds (63%) of NBF women had attained primary school only, and a higher proportion (42% BF vs. 18% NBF, P = 0.007) of BF women attained some secondary education. Two-thirds of participants had families with up to two children.
Mean daily spending on food for the household was USD5.02, with urban households spending significantly more than rural households (USD6.41 vs. USD3.80, respectively, P = 0.001).
Ten participants reported taking supplements, four being iron, and six not reporting the specific type. Due to uncertainty of supplement types, doses and quantities, these supplement intakes have not been accounted for in nutrient intakes, thus dietary intake data reflects food and drink consumption only.
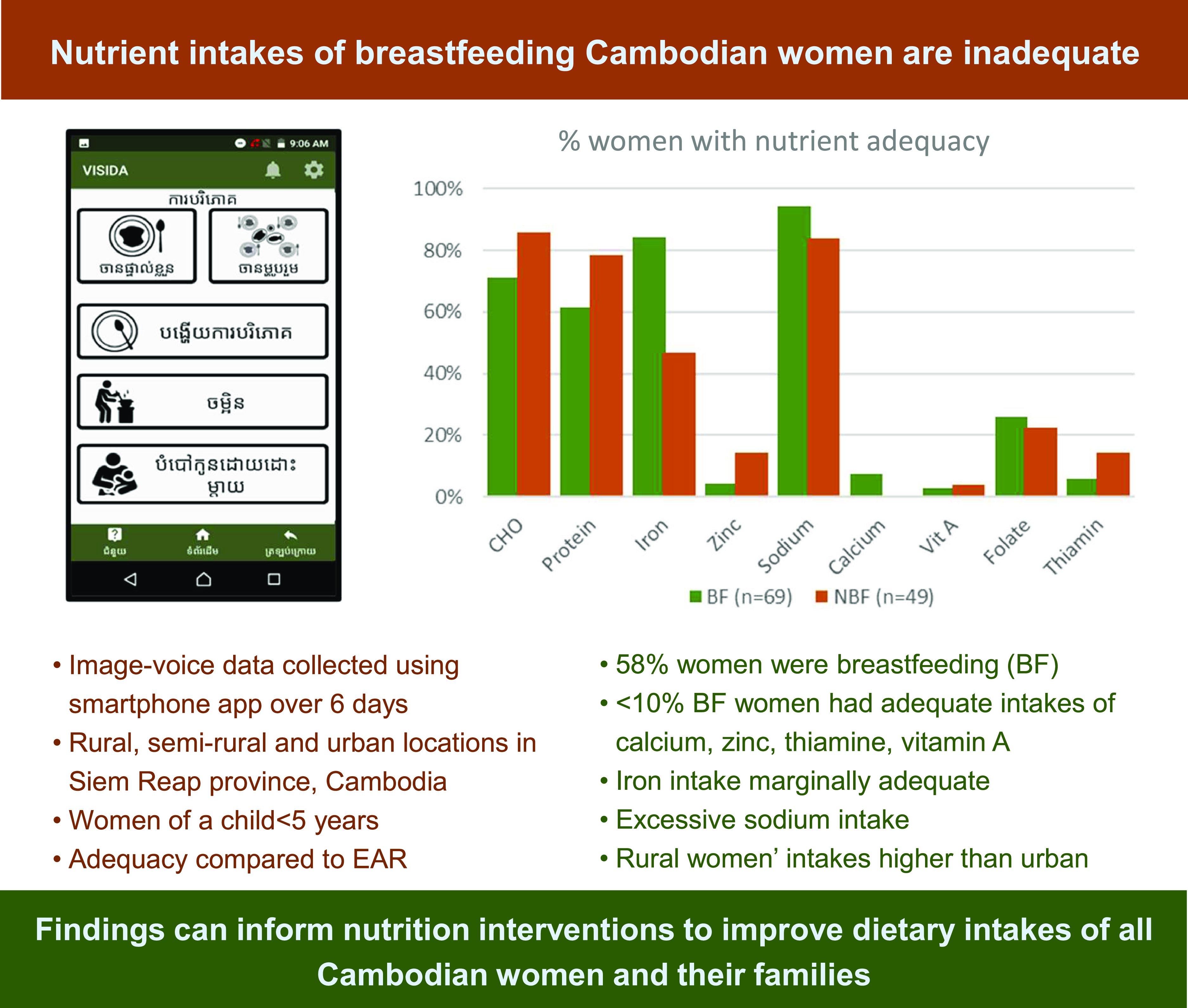
Nutrient intakes and adequacy for breastfeeding and non-breastfeeding women
Overall energy intakes were moderately low with less than 1% of all women with intakes above the estimated energy requirement.(32) Nutrients with the highest proportions of women with an estimated adequate intake were protein, carbohydrate, vitamin B12, iron and phosphorus. Less than 10% of participants were adequate in intakes of vitamin A, vitamin C, thiamine, calcium, zinc and potassium. Ninety per cent of all women consumed adequate sodium, with 64% of women exceeding the tolerable upper daily intake limit of 2300mg.(2) No other nutrient intakes exceeded recommended upper limits.(2)
Overall median daily nutrient intakes of BF women were significantly higher than those of NBF women for total energy and all nutrients except total fat and vitamin C (see Table 2). More BF women consumed adequate sodium than NBF (74% BF vs. 49% NBF, P = 0.006). A significantly higher proportion of BF women had adequate nutrient intakes compared to NBF women for iron (84% BF vs. 47% NBF, P = 0.001), vitamin B12 (84% BF vs. 67% NBF, P = 0.033), and with non-significant differences in proportions for calcium (7.2% BF vs. 0% NBF, P = 0.054) and folate (26% BF vs. 22% NBF, P = 0.651) (Supplementary Table 2 lists P-values comparisons by BF status).
Table 2. Median nutrient intake and proportion of adequate intake for total, breastfeeding, and non-breastfeeding mothers
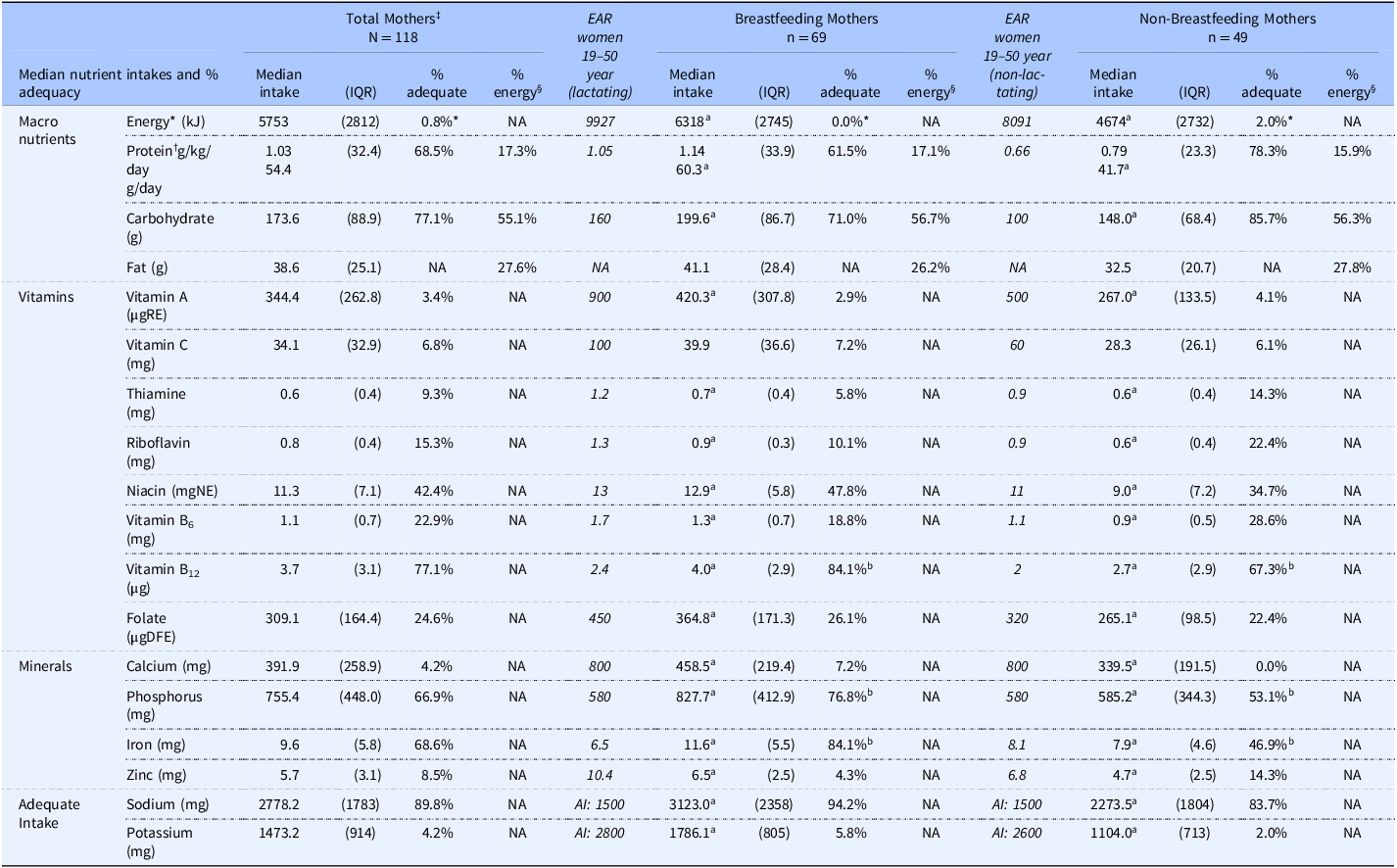
IQR, Inter-quartile range; NA, not applicable; RAE, retinol activity equivalent; NE, niacin equivalent; DFE, dietary folate equivalent; AI, Adequate Intake.
Statistically significant differences between groups are indicated by superscript (a,b) along rows. Pearson Chi-squared test used for adequacy proportions; P < 0.05. Non-parametric independent samples test of significance used for medians; *Proportion of participants with energy intakes lower than estimated energy requirement (EER), based on IOM equation(32): 354 – (6.91 × age [y]) + PA × ((9.36 × weight [kg]) + 726 × height [m])), where PA refers to physical activity level of which 1.12 of ‘low active’ level was applied, and mean age, weight and height for BF or NBF women respectively; and +400kcal applied to BF women’s EER. †Protein EAR calculated from body weight of each participant (n = 111), then identified as adequate or inadequate; (n = 8 missing body weight values). Protein grams per kilogram body weight were calculated from median body weights of each subsample: total mothers = 52.7 kg; BF = 52.7 kg; NBF = 52.6 kg. ‡One missing value of total mothers (did not indicate BF status). §Institute of Medicine (IOM) acceptable range of macronutrient energy contributions: protein 10–35%; carbohydrate 45–65%; fat 20–35%.
NB: For total mothers, significant differences between adequate and inadequate proportions were found for every nutrient except niacin, using Pearson Chi-squared test; P < 0.05.
There were clinically relevant but not statistically significant differences in the proportion of BF women with adequate nutrient intakes compared to NBF women reported for protein (62% BF vs. 78% NBF, P = 0.062), carbohydrate (71% BF vs. 86% NBF, P = 0.061), thiamine (5.8% BF vs. 14% NBF, P = 0.118), riboflavin (10% BF vs. 22% NBF, P = 0.067) and zinc (4.3% BF vs. 14% NBF, P = 0.056) (Table 2).
No significant differences in median intakes for any nutrient were found between younger (18–30 years) and older (31–49 years) women, although a trend towards higher intakes of macronutrients and folate was evident for younger women. A significantly greater proportion of younger women were breastfeeding (68% BF vs. 32% NBF of 18–30-year-olds; P = 0.001).
While total energy intakes significantly differed based on breastfeeding status (6318 kJ BF vs. 4674 kJ NBF, P = 0.001), proportions of macronutrient contributions to energy were similar, and within IOM’s acceptable ranges for protein, carbohydrate, and fat.(32)
Differences in nutritional intakes and adequacy by location
One hundred per cent nutrient adequacy was not achieved for any nutrient by any location group. Median energy and nutrient intakes were generally higher among rural compared to urban women, with significantly higher intakes reported for carbohydrate (198 g vs. 152 g, P = 0.010), dietary fibre (8.8 g vs. 6.5 g, P = 0.030) and calcium (468 mg vs. 362 mg, P = 0.044) (see Table 3). Significantly higher nutrient adequacy was evident for rural women in folate (28% rural vs. 44% semi-rural vs. 9.1% urban; P = 0.003) and vitamin A (8.5% rural vs. 0% for both semi-rural and urban; P = 0.044), and not significantly different for protein (73% rural vs. 56% semi-rural, P = 0.303), carbohydrate (83% rural vs. 73% urban; P = 0.464), iron (77% rural vs. 64% urban; P = 0.317) and calcium (8.5% rural vs. 0% semi-rural vs. 2.3% urban; P = 0.155) (Supplementary Table 3 shows location comparisons with P-values). Generally, intakes for semi-rural women were between rural and urban, although they had lowest intakes of protein (51 g), fat (32 g) and vitamin A (296 µgRE).
Table 3. Median nutrient intake and proportion of adequate intake for total mothers, and comparing locations
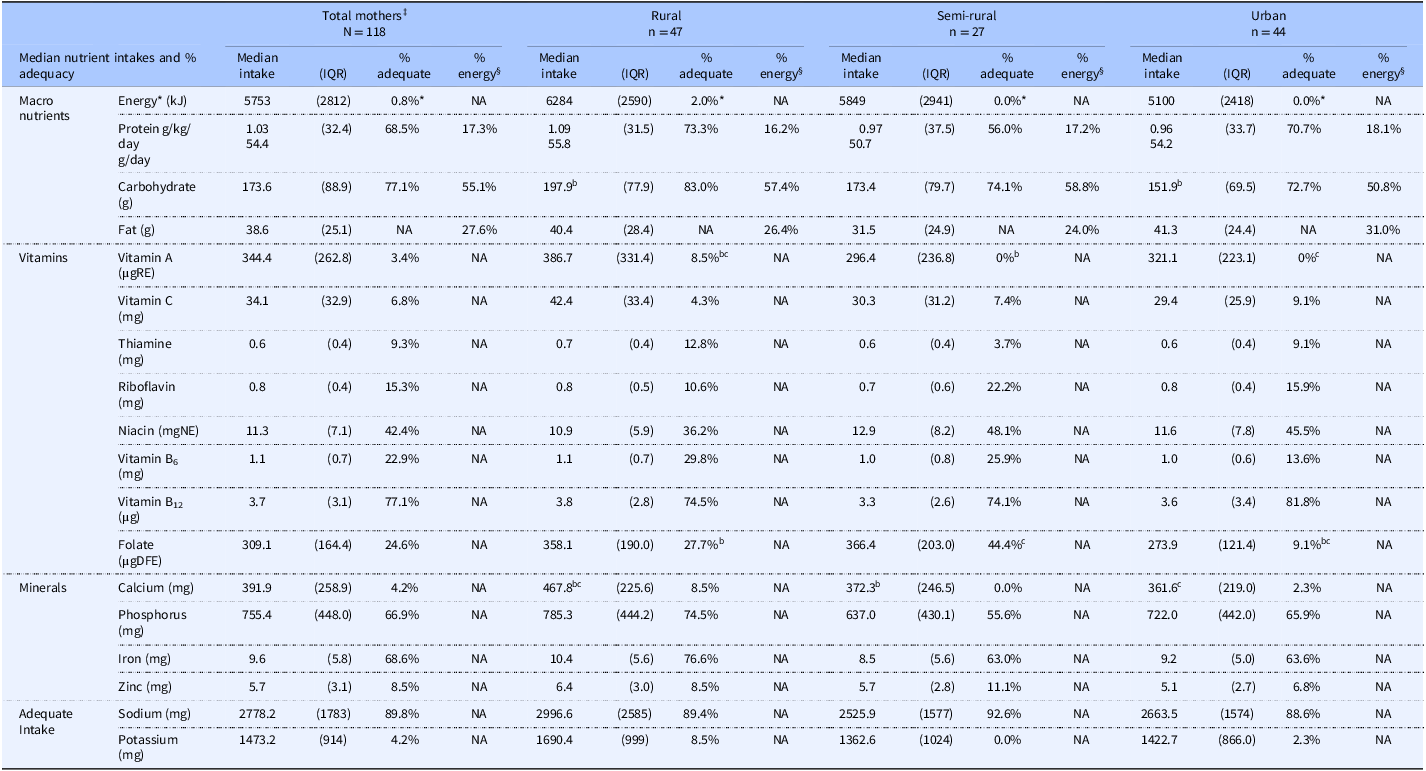
IQR, Inter-quartile range; NA, not applicable; RAE, retinol activity equivalent; NE, niacin equivalent; DFE, dietary folate equivalent.
Statistically significant differences between groups are indicated by superscripts (a,b,c) along rows. Pearson Chi-squared test used for adequacy proportions; P < 0.05. Non-parametric independent samples test of significance used for medians; *Proportion of participants with energy intakes lower than estimated energy requirement (EER), based on IOM equation(32): 354 – (6.91 × age [y]) + PA × ((9.36 × weight [kg]) + 726 × height [m])), where PA refers to physical activity level of which 1.12 of ‘low active’ level was applied, and mean age, weight and height for rural, semi-rural and urban women respectively. †Protein EAR calculated from body weight of each participant (n = 111), then identified as adequate or inadequate; (n = 8 missing body weight values). Protein grams per kilogram body weight were calculated from median body weights of each subsample: total mothers = 52.7 kg; rural = 51.3 kg; semi-rural = 52.4 kg; urban = 56.3 kg. ‡One missing value of total mothers (did not indicate BF status). §Institute of Medicine (IOM) acceptable range of macronutrient energy contributions: protein 10–35%; carbohydrate 45–65%; fat 20–35%.
Urban women reported the total lowest energy intakes (5100 kJ/d), and lowest folate (274 µgDFE), carbohydrate (152 g) and dietary fibre (6.5 g) intakes. A high rate of adequacy (90%) was reported for sodium, whereas potassium intakes were found to be very low, i.e. much lower that the AI across all locations (Table 3). Conversely, adequate intake of calcium, vitamin A and potassium was met by <3% of semi-rural and urban women.
Macronutrient contributions to energy differed across locations, with higher carbohydrate proportions for rural (57%) and semi-rural (59%) women compared to urban (51%), while protein (18%) and fat (31%) made higher contributions for urban women’s diets.
Discussion
This novel study using image-voice-based methods to collect dietary intakes from Cambodian women identified very low adequate nutrient intakes of BF women, placing them and their breastfed infants at nutritional risk. Results highlight that intakes of most nutrients by Cambodian women residing in Siem Reap province were inadequate, particularly for vitamin A, vitamin C, thiamine, calcium, zinc and folate, while sodium intakes were excessive. Although not significant, compared to NBF women proportionally fewer Cambodian BF women had adequate intakes of protein, carbohydrate, thiamine, riboflavin, vitamin B6 and zinc, while women from rural areas had higher energy intakes and more adequate nutrient intakes, particularly vitamin A, thiamine, calcium, iron and potassium compared to urban WRA whose folate intakes were highly inadequate. This provides evidence of the double burden of malnutrition in Cambodian WRA as low nutrient intakes contribute to micronutrient deficiencies, despite that rates of underweight are decreasing.(6) Intakes of these nutrients are similar to intakes reported from other southeast Asian LMICs.(Reference Roos, Ponce and Doak35–Reference Ferguson, Watson and Berger37)
Findings from the current study conflicted with other studies of dietary intake of Cambodian WRA. Whereas both Bunthang et al. (2014)(Reference Bunthang, Nam and Phen19) and Verbowski et al. (2018)(Reference Verbowski, Talukder and Hou18) reported intakes of protein, and most B-vitamins that were similar to the current study for rural women, they also reported considerably higher carbohydrate, vitamin A and vitamin B12 and higher calcium and zinc intakes. Differences could be attributed to alternative primary aims, data collection or analysis method, provincial region, or recent changes in the Cambodian diet resulting from economic growth between 2014 and 2019.(8) While the low energy intakes of this current study were consistent with these other studies, the relative validity study reported lower energy intakes for the image-voice method compared to 24-hour recall, which may indicate under-estimation.
Dietary adequacy differs by breastfeeding status
Nutritional adequacy of BF women’s dietary intakes is of paramount importance to prevent nutrient deficiencies. The finding that nearly 40% of BF women did not have adequate intakes of protein could suggest that breastmilk production or composition could be compromised(Reference Brown38) or increased risk of maternal skeletal muscle wasting.(Reference Dewey39) Similarly, poor maternal intakes of thiamine, riboflavin, vitamin B6, vitamin B12, vitamin A, vitamin C and iodine, could adversely impact nutrient concentrations in breastmilk(Reference Allen3,Reference Keikha, Shayan-Moghadam and Bahreynian40) and hence influence the nutritional status of breastfed infants.
Only 6% of BF and 14% of NBF women in the current study had adequate thiamine intakes. Positive impacts of thiamine supplementation or fortification have been demonstrated in three intervention studies with rural Cambodian BF women that reported thiamine supplements(Reference Coats, Frank and Reid41) or thiamine-fortified fish sauce(Reference Gallant, Chan and Green42,Reference Whitfield, Karakochuk and Kroeun43) rapidly restored serum thiamine and breastmilk thiamine concentrations, potentially reducing the risk of infantile beriberi.
Vitamin A intakes were highly inadequate for all women, consistent with reported intakes in other Asian countries.(Reference Passarelli, Free and Allen44) This contrasts with previous studies in Cambodian WRA that reported very low rates of vitamin A deficiency of either zero,(Reference Karakochuk, Whitfield and Barr45) less than 1%(Reference Wieringa, Sophonneary and Whitney46) or 3.2%.(8) These conflicting findings could reflect varying public health advice and vitamin A supplementation initiatives in Cambodia over time. In 2002, a government programme started distributing vitamin A capsules to postpartum women, but this ceased in 2010 upon WHO(47) advice strongly opposing vitamin A supplementation.(Reference McLean48)
Calcium intakes for all NBF women were inadequate and significantly lower than BF women. Cambodians regularly eat small, whole fish, including bones, which are a rich source of highly bioavailable calcium.(Reference Bunthang, Nam and Phen19) Food composition databases used for nutrient analyses in Cambodian studies do not specify whether small fish include bones, thus, it is possible that actual calcium intakes are higher than these studies indicate. Further research is needed to accurately assess dietary intake of calcium intake and the influence of calcium intake on bone mass and breast milk to better understand the full impact of low calcium intake for both mothers and their breastfed children.
The large difference in the proportion of women with adequate dietary iron intakes between BF (84%) and NBF women (47%) is attributed to both the significantly higher iron intakes of BF women and the higher EAR for NBF women. IOM calculates iron EAR by considering basal iron requirements, which are impacted by menstruation, oral contraception use, and iron secreted through breastmilk, so it is possible that the iron requirement of menstruating breastfeeding women may be underestimated.(33) Additionally, IOM also based the iron EAR on a high bioavailability of 18%,(33) however experts suggest 10% bioavailability should be applied to a less refined diet of fish/meat and rice, typical of Cambodian’s diet.(12,Reference Allen, Carriquiry and Murphy15) This suggests Cambodian women need to increase their consumption of iron-rich foods to account for a poorer iron bioavailability and obtain adequate iron intake.(Reference Allen, Carriquiry and Murphy15) This highlights the need for improved methods of estimating intake and bioavailability of dietary iron.(49)
Although high rates of anaemia are evident for Cambodian WRA, studies have reported low rates of iron deficiency in Cambodian WRA with anaemia.(Reference Wieringa, Dahl and Chamnan50) Low prevalence of iron deficiency in WRA of one rural province was reportedly related to high iron content of water.(Reference Karakochuk, Murphy and Whitfield51) Other contributing factors to Cambodia’s highly prevalent anaemia rates include zinc deficiency,(Reference Wieringa, Dahl and Chamnan50) infections,(Reference Thurnham and McCabe52) hookworm and parasites(Reference Wieringa, Dahl and Chamnan50) or genetic hemoglobinopathies such as thalassaemia.(Reference Karakochuk, Whitfield and Barr45) Nearly one in five Cambodian women experience intestinal infection, particularly hookworm,(8) which is likely to worsen zinc and iron deficiency.(Reference Wieringa, Dahl and Chamnan50) Half of Cambodian women postpartum receive iron supplements(8) which may interfere with zinc absorption.(Reference Gibson14) While studies show zinc concentrations in breastmilk are positively impacted by maternal zinc supplementation, the impact of higher dietary zinc intake alone is inconclusive.(Reference Keikha, Shayan-Moghadam and Bahreynian53,Reference Shaaban, El-Hodhod and Nassar54) What is clear, however, is the urgent need for Cambodian BF women to have greater access to foods rich in zinc to prevent deficiency, making this a priority for intervention.(Reference Wieringa, Dijkhuizen and Berger55) These factors highlight that anaemia is related to multiple causes other than iron deficiency, requiring further investigation.
While dietary folate intakes were significantly higher among BF women, adequate intakes were similar between BF and NBF women. No other study with Cambodian WRA has measured dietary folate intake, however, folate inadequacy is widespread among females in southeast Asia.(Reference Passarelli, Free and Allen44) With one in five (19.2%) Cambodian WRA deficient in folate (<10 nmol/l)(8) and its important role in reducing the risk of neural tube defects,(Reference De Benoist56) folate remains as a nutrient of concern for all WRA. Since 2007, a Cambodian national anaemia programme has distributed iron-folic acid supplements for pregnant and postpartum women, however, non-compliance was high, with only 49% of postpartum women taking supplements, mostly due to poor understanding of its continued benefit.(Reference McLean48) WHO recommends weekly iron (60 mg) and folic acid (2.8 mg) supplementation for WRA in countries with anaemia rates greater than 20% as a strategy to reduce anaemia and neural tube defects,(57) which Cambodia’s nutrition programme has been implementing for several years.(58)
Sodium is a nutrient of concern due to three-quarters of BF women consuming above the upper limit. The Cambodian diet includes many high-salt items, particularly fish pastes, soy sauce, fish sauce, pickled fruit and vegetables and salt-chilli dips, along with salt from chicken seasoning and monosodium glutamate used in marinades and mixed dishes (JW personal communication). WHO reports that a diet high in sodium intake >2000 mg/d coupled with low potassium intake contributes to increased risk of hypertension, heart disease and stroke.(59) With 35% of Cambodian women over forty years experiencing hypertension(Reference Chham, Buffel and Van Olmen60) and 86% of this cohort of BF women exceeding WHO’s recommendations, there is an urgent need for early intervention with WRA. Cambodian healthcare services provide hypertension management, however little is known of its effectiveness and whether it includes nutritional advice about reducing sodium intake.(Reference Chham, Buffel and Van Olmen60)
Location differences in dietary intakes
Despite rural populations having higher poverty rates, the current study suggests rural WRA diets may be more adequate than urban women who have greater food variety and higher income(61) with subsequent higher daily spending on food. Reasons for eating patterns reflecting intake differences include a greater reliance on rice in rural areas evidenced by higher carbohydrate intakes.(Reference Sar, Gilbert and Marks62) In et al. (2015)(Reference In, Lambre and Camel63) reports urban dwellers eat higher quantities of meat, fruit and vegetables than rural dwellers, however this is not reflected in higher iron, zinc or vitamin intakes in the current study. Rural WRA have greater opportunity for home food production by growing fruit and vegetables and raising livestock (chickens, ducks, pigs) or farming fish, which has been shown to increase intakes of energy, protein, vitamin A and some B-vitamins.(Reference Verbowski, Talukder and Hou18) Rural areas have closer access to land for foraging water plants, wild potatoes, frogs and crabs (JW personal communication), which may support dietary diversity and higher micronutrient intakes, however further research is required to substantiate this.
It was unexpected that intakes of many nutrients were lowest among semi-rural women, given that the site was close to the Tonle Sap Lake, known for its market gardens. Easy access to folate-rich green leafy vegetables may account for the higher adequate intakes of folate compared to rural and urban locations, however further research is needed to explore this.
Implications for future research
To date, government nutrition policies targeting nutritional deficiencies in Cambodian WRA have focused on iron, vitamin A, folic acid and iodine.(5,Reference Wieringa, Dijkhuizen and Berger55) However, the current study has highlighted other nutrients were highly inadequate among Cambodian WRA, particularly for calcium, zinc, thiamine and vitamin C and this requires further investigation. Data on nutrient deficiencies in Cambodia are limited or unavailable for most nutrients, indicating the need for a comprehensive national nutritional surveillance study, particularly for Cambodian WRA and other vulnerable population groups.
National Academies of Science, Engineering, and Medicine (NASEM, which has replaced IOM) recognises that applying EARs to LMICs requires specific considerations, including lower bioavailability for some nutrients, such as zinc, iron and folate and higher prevalence of infections exacerbating micronutrient deficiencies and chronic disease risk.(49) This highlights the need to establish country-specific NRVs for the Cambodian population.
Iron, calcium and folate have been reported as the most difficult nutrients to meet requirements using locally available foods alone in southeast Asia.(Reference Ferguson, Watson and Berger37) New strategies are needed to increase availability of nutritious foods across Cambodian provinces. The Cambodian government has recognised that food fortification is a feasible approach to address deficiencies,(5,Reference McLean48,Reference Theary, Panagides and Laillou64) with studies already trialling rice fortified with multiple micronutrients,(Reference Kuong, Tor and Perignon65) and fish sauce fortified with thiamine(Reference Whitfield, Karakochuk and Kroeun43) or iron,(Reference Longfils, Monchy and Weinheimer66) with promising results. Fish sauce, soy sauce and vegetable oils are readily available and commonly consumed, however only a small proportion are fortified, with very low use of fortified products evident.(Reference Theary, Panagides and Laillou64) Further fortification research accompanied by programs to raise awareness of their nutritional benefits are required.
While nutritional supplementation continues to address iron and folic acid deficiency,(Reference Roos, Ponce and Doak35,Reference McLean48) WHO recommends postpartum women receive adequate nutrient intakes through a healthy balanced diet.(47) This advice endorses educational and home-based food production programmes which promote rich food sources of key nutrients. With increasing rates of obesity(6) hypertension(Reference Jacobs, Men and Bigdeli67) and diabetes(68) targeted interventions such as peer educator programmes,(Reference van Olmen, Eggermont and van Pelt69) eHealth(Reference Steinman, van Pelt and Hen70) and healthy lifestyle initiatives should be considered(Reference Rawal, Tapp and Williams71), particularly focusing on reducing sodium intake to prevent hypertension and cardiovascular disease. Future nutritional interventions should engage with community members to tailor for Cambodia’s unique culture and beliefs, including an exploration into their common traditional mixed dishes.
Future dietary assessment with Cambodian and other LMIC populations should consider advantages of image-voice methods, such as collecting prospective ‘real-time’ data reducing participant burden and addressing dietary assessment challenges, i.e., memory recall,(72) estimating portions(Reference Burrows and Rollo73) and overcoming low literacy.(72,Reference Bell, Colaiezzi and Prata74) Increasing access to mobile phone cameras evident in LMICs enables broad use of image-based methods, which captures sufficient data to calculate macro- and micronutrient intakes of participants.(Reference Bell, Colaiezzi and Prata74) In the current study, the collection of additional voice records to images complements and aids in better data identification and quantification, reducing analyst burden for coding error. Consideration for image-voice based methods applied in this study includes using local analysts fluent in the same language as recorded data, conducting regular quality checks to obtain high-quality data, and use of reference objects such as fiducial markers to reduce coding error.(Reference Dalakleidi, Papadelli and Kapolos75) As technology improves, including natural language processing, the quality of image-voice-based methods is likely to further improve.(Reference Dodd, Adam and Windus76)
Strengths and limitations
This study was strengthened by the presence of Australian researcher (JW) living in Cambodia prior to and throughout the VISIDA project, which helped facilitate cultural understanding, collect resources, access Cambodian food and facilitate the contribution of local families during development. Another study strength was the complementary use of both image and voice data during data collection, creating a more robust dataset. An early cut-off of data collection due to the COVID-19 pandemic limited recruitment at the semi-rural site, resulting in its smaller sample size.
The EAR cut-point method of estimating the prevalence of inadequacy is based on populations from high-income countries. Due to the lack of NRVs specific to the Cambodian female population, the EAR cut-points from the Institute of Medicine have been pragmatically applied in this current study to allow comparison with literature internationally. Caution is suggested in using estimates of iron and calcium adequacy levels, as data may be underestimated, warranting further research.
This dietary intake assessment study was based on data from food and beverages only. While it is possible nutrient intakes for some women may have been higher, less than 10% of women reported consuming micronutrient supplements, of which the data lacked sufficient detail to quantify actual nutrient supplement content. Similarly, brands of product ingredients were not consistently identified in images or voice recordings, therefore, nutrient intake from supplements or fortified foods was not calculated and reported.
While the prospective approach of the image-voice based data collection method may be subject to participant reactivity, it reduced reliability on memory compared to other retrospective methods, such as 24-hour recall.
Conclusion
The current study indicated that Cambodian women from Siem Reap province had low energy intake, with low proportions having adequate intakes of several nutrients, excessive sodium intake and moderate iron intake. Findings indicate a need for a comprehensive nationwide nutritional surveillance and further research on thiamine, folate, calcium and zinc with BF women to identify impacts on nutrient intakes of their infants. Comprehensive, well-designed food and/or nutrient interventions are required, including education on dietary sources of priority nutrients, supplementation, and fortification programmes. These approaches need to be collaborative and informed by consultation with local Cambodian WRA to ensure cultural appropriateness.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/jns.2025.10011
Data availability statement
The data that support the findings of this study are available from the corresponding author, [JW], upon reasonable request. Also, for food intake and food composition data, please contact the corresponding author.
Acknowledgements
The authors thank ‘This Life (Cambodia)’ in coordinating the local fieldwork in Siem Reap province for the VISIDA study, particularly Mr Manith Chhoeng, Mr Billy Gorter, Mr Se Chhin and the Community Research and Consultancy team of research assistants (https://thislife.ngo/about). Thanks go to members of the VISIDA project team, especially Samantha Stewart for data management, coding and cleaning, Janelle Skinner for her role in developing the Cambodia-specific food composition database, and Connor Dodd for his expertise in developing the VISIDA app and CMS. We acknowledge our gratitude to the Cambodian mothers and their children who participated in the VISIDA study.
Authorship
All authors have read and agreed to the published version of the manuscript. JW contributed to conceptualisation, methodology, formal analysis; investigation; data curation; writing original draft preparation and editing and visualisation. KD contributed to conceptualisation, software development, supervision, data analysis and interpretation, and manuscript review and editing. TB contributed to conceptualisation, software development, supervision, data analysis and interpretation, and manuscript review and editing. CC contributed to conceptualisation, software development, supervision, data analysis and interpretation, and manuscript review and editing. MR contributed to conceptualisation, software development, project administration, funding acquisition, supervision, data analysis and interpretation, and manuscript review and editing.
Financial support
VISIDA project was undertaken by University of Newcastle and funded by the Bill and Melinda Gates Foundation (Grant OPP1171389). CC is supported by an NMHRC Research Leadership Fellowship (Level 3, 2009340 App); TB is supported by an NHMRC Investigator Grant (App1801414). Bill and Melinda Gates Foundation or NMHRC had no role in the design, analysis or writing of this article.
Competing interests
The authors declare none.
Ethical standards disclosure
The VISIDA study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the National Ethics Committee for Health Research in Cambodia (Ref No. 151 NECHR), University of Newcastle (Ref H-2018-0515) and Curtin University (HRE2022-0366) Human Research Ethics Committees in Australia. Verbal informed consent was obtained from all participants to participate in the study and use their data for publication, which was witnessed and formally recorded. No individual details, images or videos relating to an individual person are included in this manuscript.