Exclusive breast-feeding is recommended during the first months of life to secure adequate nutrition for infants. Breast milk provides all nutrients required for the infant, except vitamin D( Reference Butte, Lopez-Alarcon and Garza 1 ). Breast milk also contains hormones and enzymes that affect physiological maturing( Reference Bernt and Walker 2 ), and protects infants against respiratory infection and diarrhoea( 3 ). Long-term benefits from breast-feeding include reduced risk of obesity and type 2 diabetes in later life, and higher odds of increased intelligence( 4 ). For the mother, exclusive breast-feeding may help her to regain original weight( Reference Silva, Assis and Pinheiro 5 ) and reduce the risk for ovarian and breast cancer( Reference Feng, Chen and Shen 6 , Reference Pechlivani and Vivilaki 7 ). For society, breast-feeding is one of the most cost-effective investments a nation can make( 8 ). Still, according to WHO, there is no country in world that fully adheres to the given breast-feeding recommendations.
Norwegian health authorities recommend that infants should be exclusively breast-fed for the first 4 to 6 months of life depending on the mother’s and infant’s needs, followed by a gradual introduction of foods in parallel with continued breast-feeding( 9 ). Before 2016, Norwegian mothers were recommended to breast-feed exclusively for the first 6 months of life( 10 ). These recommendations were adjusted in 2016, however, after the subjects had participated in the current study. Breast-feeding initiation rates are high (99 %) in Norway compared with other nations( Reference Drago, Hayes and Yi 11 ). Despite long paid maternity leave for 46 or 56 weeks, depending on 100 or 80 % degree of wage coverage respectively( 12 ), exclusive breast-feeding rates at 6 months are low in Norway. The latest national cross-sectional study on infant nutrition from 2013 showed that 17 % were exclusively breast-fed at 5·5 months( Reference Lande and Helleve 13 ). For Norwegian immigrants these numbers were even lower. Only 7 % of Norwegian-Somali and 10 % of Norwegian-Iraqi infants were exclusively breast-fed at 4 months of age( Reference Grewal, Andersen and Sellen 14 ).
Socio-economic factors such as maternal education and lifestyle variables like maternal smoking are associated with duration of breast-feeding and exclusive breast-feeding( Reference Kristiansen, Lande and Overby 15 ). Norwegian public health policy aims to reduce the social gap in health( 16 ). A long maternity leave is established inter alia to enable breast-feeding for all infants regardless of their mother’s socio-economic status. Previous studies have shown that people with higher socio-economic status breast-feed longer than people with lower socio-economic status( Reference Flacking, Nyqvist and Ewals 17 ). This contributes to maintaining the social gradient in health, based on the documented health benefits of breast-feeding.
The Norwegian health authorities have recently launched a specific goal to increase the exclusive breast-feeding rate at 4 months to 60 %( 18 ). A national study on breast-feeding with data from 2013 shows that there has been no improvement in breast-feeding duration from early 2000( Reference Grewal, Andersen and Sellen 14 ). To reach such high breast-feeding rate one needs to explore predictors of breast-feeding. Newer data are needed to explore whether there is a social gap in duration of exclusive breast-feeding and any breast-feeding, respectively, of Norwegian infants in 2016. Further, the socio-economic variables that have been investigated have mostly been limited to education and smoking.
There is a general lack of acknowledgment of obesity issues related to breast-feeding and breast-feeding duration( 18 ). Worldwide, 40 % of women aged 18 years or older are overweight and 15 % are obese( 19 ). In Norway, 24 % of woman aged 25–44 years are overweight and 10 % are obese( 20 ). Both the WHO and Norwegian public health policy have addressed overweight as one of the main risk factors of premature death( 16 , 21 ). Overweight and obesity have health consequences across the life cycle, with an increased risk of non-communicable diseases( 19 ). One of the health implications related to maternal overweight and obesity is the seemingly lower ability to initiate and sustain breast-feeding( Reference Winkvist, Brantsæter and Brandhagen 22 ). Due to the growing epidemic of overweight, we wanted to include maternal BMI in the analyses to explore whether this association is present in a recent Norwegian population( Reference Winkvist, Brantsæter and Brandhagen 22 , Reference Krause, Lovelady and Østbye 23 ).
The baseline data from the randomized controlled trial Early Food for Future Health was used to explore associations between socio-economic factors and maternal BMI, respectively, and duration of any breast-feeding/exclusive breast-feeding during the infants’ first 5 months of life.
Methods
Subjects and design
In 2016, Norwegian parents were invited to participate in the Early Food for Future Health study. Parents were eligible to participate if they had a 3–5-month-old infant, were literate in Norwegian and were responsible for providing food to their infant. Parents with infants aged 3–5 months were recruited through posting an information site and video on social media. All Norwegian health centres were informed about the study, including public health nurses who could inform mothers about the study. Parents consented to participate on an information site, and were subsequently sent an email with a link to a questionnaire when the infant had reached 5 months of age. Questionnaire data were collected between March 2016 and October 2016.
Among the 1048 participating parents, there were 960 unique infants (some had registered their infant several times). Of these, 718 parents completed the questionnaire (74·8 %). Baseline data from both the intervention and the control group were used in the current analyses. A sample of 718 Norwegian infants aged 5–6 months was established. After the duplicates were removed there were only three fathers left. These were excluded from the present study, leaving the total number of participants at 715 mother/infant dyads.
The Norwegian Centre for Research Data evaluated the study and informed consent was obtained from mothers/parents.
FFQ
An FFQ was developed for the Early Food for Future Health study to assess daily food consumption, breast-feeding duration and age at introduction of solid foods. Parents were asked to complete the questionnaires when their infant was between 5 and 6 months old.
Questions about breast milk and other liquids were asked as follows: ‘What kind of food and drinks has the infant received the first 6 months of life? Tick the box for each month (0, 1, 2, 3, 4, 5, 6) the infant has received the listed foods and drinks’ (breast milk, formula, water, juice, baby porridge, dinner, fruits/berries). Month 0 represents the time before the age of 1 month whereas month 1 represents 1 month of age and so forth.
Parents responded to questions concerning time of introduction of complementary foods as ‘How old was your infant when he/she first was introduced for these foods?’ (porridge, industrial and homemade; mashed vegetables, industrial and homemade; mashed fruits, industrial and homemade; meals with red/white meat or fish, industrial and homemade; and bread). Response alternatives were given in months.
All presented variables above were included when calculating exclusive breast-feeding duration.
Socio-economic status
Socio-economic status was measured with six different questions. (i) Education level, categorized as less than lower secondary school, upper secondary school, college/university up to 4 years, and college/university more than 4 years. This variable was subsequently recoded into high or low education level (college/university education or not). (ii) Main activity/main activity before maternity leave had ten different categories (working full-time; working part-time; student; unemployed; homemaker; sick leave; disability benefits; leave; rehabilitation; other). These were recoded into working full-time, part-time, student and not working. (iii) Size at nearest urban area was reported in four categories: ≤4999, 5000–14 999, 15 000–49 999, ≥50 000 people. (iv) Geographic region was reported as nineteen different regions which were recoded into capital, East, South, West, Middle and North regions. (v) Ability to pay an unforeseen expense of 3000 NOK was categorized as ‘yes’, ‘no’ and ‘maybe’. These were recoded into ‘yes’ and ‘no/maybe’. (vi) The last question asked if participants had experienced difficulties paying their rent, food or transportation costs during the last 6 months. Possible responses were ‘sometimes’, ‘often’ or ‘never’, subsequently recoded into ‘difficulties’ and ‘no difficulties’. In addition, we included one question regarding parental mother tongue, as an indicator of being native or not: ‘Do you or the other parent have another mother tongue than Norwegian?’ Responses were ‘yes’ or ‘no’.
Maternal BMI
BMI is calculated as a person’s weight in kilograms divided by the square of his/her height in metres (kg/m2). Underweight is defined as BMI less than 18·5 kg/m2, and normal BMI is defined as BMI between 18·5 and 25 kg/m2. Overweight is defined as BMI equal to or greater than 25 kg/m2 and obesity is defined as BMI equal to or greater than 30 kg/m2 ( 24 ). Maternal BMI was coded according to these cut-offs into four categories: normal, underweight, overweight and obese.
Covariates
The questionnaire also included sociodemographic variables such as parental age (reported as a continuous variable), gestational age (after age 38 weeks) and parity. A woman’s parity is defined as the number births( 25 ). In the present paper, parity was categorized as 1, 2 or ≥3 births.
We included smoking as a lifestyle variable in our study. The response categories for parents’ smoking status were ‘no, never’, ‘no, but quitted’, ‘yes, but not daily’ and ‘yes, daily’. These response categories were recoded into ‘no’ and ‘yes’. We also included physical activity, which was assessed with the following question: ‘How many times a week are you physically active to the extent of being out of breath or sweating?’ Response alternatives were ‘never’, ‘less than once a week’, ‘twice a week’, ‘3–4 times per week’ and ‘5 times or more per week’. This variable was subsequently dichotomized into ≤2 times/week and ≥3 times/week.
Definition of breast-feeding
Being exclusively breast-fed at a given age is defined as receiving only breast milk and not being introduced to any other liquids or foods. Vitamin supplements, supplements and cod-liver oil do not affect exclusive breast-feeding status( 26 ). Being breast-fed at a given age is defined as receiving breast milk, either given exclusively or with supplementary foods and/or drinks. Breast-feeding was categorized into exclusive breast-feeding and any breast-feeding in the present paper. The variable ‘exclusively breast-fed’ was constructed in SPSS. Duration of exclusive breast-feeding was calculated as the consecutive months the infant had received breast milk, without being introduced to any other liquids or foods. For example, an infant would be exclusively breast-fed at 5 months of age if having received breast milk at 5 months of age, without any other foods or liquids at any age point up to 5 months of age.
Data analysis
Associations between socio-economic factors and maternal BMI, respectively, and duration of exclusive breast-feeding and any breast-feeding were assessed at 4 and 5 months of age.
Predictor variables were selected based on earlier studies, and socio-economic variables that were thought to affect breast-feeding and exclusive breast-feeding were included. Univariate tests where the P value was less than 0·1 were considered candidates for the adjusted model. The following variables were included: maternal age, maternal education, marital status, parity, maternal BMI, degree of urbanization, geographic region, ability to pay an unforeseen expense of 3000 NOK, difficulties with running expenses, smoking status, whether mother/father had mother tongue other than Norwegian and physical activity. There were different variables included in the different models, as only the variables from the univariate model with P value of less than 0·1 were selected for each model. Maternal education and maternal age are two well-known predictors of breast-feeding and exclusive breast-feeding( Reference Kristiansen, Lande and Overby 15 , Reference Thulier and Mercer 27 , Reference Scott and Binns 28 ), and were therefore included in all analyses regardless of their statistical significance level in the univariate tests. Potential violations of multicollinearity assumptions were tested by treating the categorical values as continuous in a linear regression and collinearity diagnostics were performed. Since we were not able to evaluate under-reporting or over-reporting of infant diet, the participants’ responses regarding infant diet were kept as originally reported in the analysis.
The outcome variables (exclusive breast-feeding and any breast-feeding) are categorical. The predictor variables are dichotomous and categorical. Binary logistic regression analyses were used to examine factors that contribute to breast-feeding and exclusive breast-feeding. A two-tailed 5 % level of significance was used. Results were presented as OR with 95 % CI.
All statistical analyses were conducted using the statistical software package IBM SPSS Statistics version 24.
Results
Table 1 presents selected characteristics of the infants and their mothers. The gender distribution among the infants was almost 50 %. About 80 % of mothers had college/university education and 36·5 % were physically active three times or more weekly. Almost 13 % of the parents had a mother tongue other than Norwegian. Only 3·8 % of the mothers smoked. The proportion of exclusively breast-fed infants the first month of life (age=0 months) was 73·6 %, at 4 months it decreased to 52·7 %, and at 5 months it dropped to 16·4 % (Fig. 1). The proportion of infants who were breast-fed but not necessarily exclusively started at 94·8 % the first month of life and decreased slowly to 81·0 % at 5 months of age (Fig. 1).
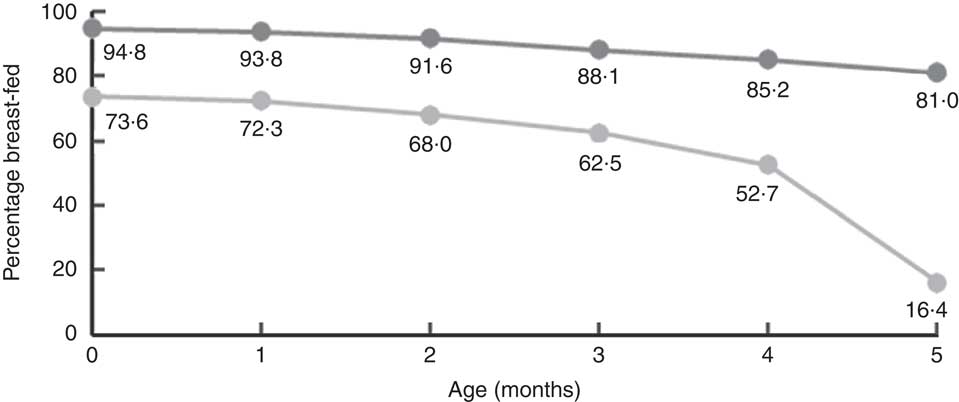
Fig. 1 Any breast-feeding (![]() ) and exclusive breast-feeding (
) and exclusive breast-feeding (![]() ) during the first 5 months of life among Norwegian infants (n 715), Early Food for Future Health study, March–October 2016
) during the first 5 months of life among Norwegian infants (n 715), Early Food for Future Health study, March–October 2016
Table 1 Characteristics of infants and their mothers (n 715), Early Food for Future Health study, March–October 2016

† Data are presented as percentages for categorical variables, or as means and sd for continuous variables.
‡ Physically active to the extent of being out of breath and sweating.
Factors associated with breast-feeding
Factors associated with any breast-feeding at age 4 and 5 months are presented in Tables 2 and 3. At the age of 4 months, infants of mothers living in a rural area of 5000–14 999 people had lower odds of being breast-fed compared with infants of mothers living in bigger cities (≥50 000 inhabitants). Further, infants of mothers with overweight/obesity had lower odds of being breast-fed at 4 months of age compared with infants whose mothers had normal BMI (Table 2).
Table 2 Adjusted OR and 95 % CI of exclusive breast-feeding (n 600) and breast-feeding (n 700) at 4 months of ageFootnote † among Norwegian infants, Early Food for Future Health study, March–October 2016
Ref., referent category.
* P<0·05, **P<0·01.
† Two models are presented with different covariates included; this explains the open spaces in the table.
‡ Adjusted for maternal education, maternal age, marital status, number of children, maternal BMI, smoking status, ability to pay an unforeseen expense of 3000 NOK and degree of urbanization.
§ Adjusted for maternal education, maternal age, marital status, maternal BMI, smoking status, ability to pay an unforeseen expense of 3000 NOK, problems with running expenses and degree of urbanization.
║ Maternal age in years.
Table 3 Adjusted OR and 95 % CI of exclusive breast-feeding (n 703) and breast-feeding (n 700) at 5 months of ageFootnote † among Norwegian infants, Early Food for Future Health study, March–October 2016

Ref., referent category.
*P<0·05, **P<0·01.
† Two models are presented with different covariates included; this explains the open spaces in the table.
‡ Adjusted for maternal education, maternal age, marital status, number of children, geographic region and degree of urbanization.
§ Adjusted for maternal education, maternal age, marital status, maternal BMI, smoking status, ability to pay an unforeseen expense of 3000 NOK, problems with running expenses and degree of urbanization.
║ Maternal age in years.
At 5 months, infants with highly educated mothers had higher odds of being breast-fed compared with infants of mothers with less education, as did infants with a married mother compared with other civil status (Table 3).
Factors associated with exclusive breast-feeding
BMI was associated with exclusive breast-feeding at 4 months of age (Table 2). Infants having mothers who were overweight or obese had lower odds of being exclusively breast-fed compared with infants of normal-weight mothers. Higher maternal age was negatively associated with exclusive breast-feeding at 4 months of age. Maternal civil status and degree of urbanization of home place were associated with exclusive breast-feeding at age 4 months.
Parity was significantly associated with exclusive breast-feeding at both 4 months (Table 2) and 5 months (Table 3). Higher parity yielded higher odds of the infant being exclusively breast-fed compared with infants of mothers with only one child. Infants of mothers living in the western part of Norway had higher odds of being exclusively breast-fed at 5 months of age compared with infants in the capital region.
Discussion
The aim of the current study was to investigate the association between socio-economic factors and maternal BMI, respectively, and exclusive breast-feeding/any breast-feeding among Norwegian infants at 4 and 5 months of age. High maternal education was positively associated with breast-feeding at age 5 months of life. However, there was no significant association between high maternal education and exclusive breast-feeding. Our results show that there are associations between socio-economic factors such as maternal education related to breast-feeding, but there are also strong associations between maternal BMI and both breast-feeding and exclusive breast-feeding.
The total number of ever breast-fed infants in the present study was high, which is similar to previous studies in Norway( Reference Lande, Andersen and Bærug 29 ). However, the percentage of exclusively breast-fed infants was 16·4 % at 5 months, which is 10 percentage points lower than what has been reported in earlier studies carried out in Norway( Reference Kristiansen, Lande and Overby 15 ). This could indicate a real change over time or it could reflect selection bias. The current study recruited participants from all over Norway, but the sample is skewed towards a more well-educated population and could be different from the national study.
Maternal education
Several studies have found a significant association between maternal education and the duration of exclusive breast-feeding or any breast-feeding( Reference Kristiansen, Lande and Overby 15 , Reference Bærug, Laake and Løland 30 ). In the present study, we found no significant association between maternal education and exclusive breast-feeding. Similar results were also found in an Icelandic study( Reference Thorisdottir, Gunnarsdottir and Thorsdottir 31 ). However, the odds of being breast-fed at 5 months was significantly higher for infants of mothers with high education.
Maternal education is often used to describe socio-economic status because it reflects both knowledge and economy( Reference Solar and Irwin 32 ). Cognitive function could be affected by the knowledge and skills achieved through education and may therefore make people with higher education more receptive to health education messages( Reference Solar and Irwin 32 ). Health promotion interventions such as breast-feeding promotion may therefore be more efficient in groups with higher education.
Degree of urbanization
The current study found that infants of mothers living in smaller communities (5000–14 999 inhabitants), compared with infants living in bigger cities (≥50 000 inhabitants), had lower odds of being both breast-fed and exclusively breast-fed at 4 months. The same association was found by Lande et al., who showed that an increased number of inhabitants yielded higher odds of being exclusively breast-fed at 4 and 6 months of age( Reference Lande, Andersen and Bærug 29 ). Allen et al. found that hospitals in less urbanized counties scored lower on breast-feeding assistance, staff training, and structural and organizational aspects of care. They suggested that the differences in breast-feeding rates could be affected by the differences in maternity care practices supportive of breast-feeding( Reference Allen, Perrine and Scanlon 33 ). In the current study, infants of mothers living in the smallest communities had higher odds of being exclusively breast-fed at 4 and 5 months of age, compared with infants of mothers living in bigger cities (≥50 000 inhabitants). However, there were few participants in these groups and the association could therefore be affected by the small selection in this group.
Maternal BMI
Maternal overweight and obesity has been reported to be negatively associated with breast-feeding duration and initiation( Reference Winkvist, Brantsæter and Brandhagen 22 , Reference Baker, Michaelsen and Sørensen 34 ). Our study supports these findings, as infants of overweight or obese mothers had lower odds of being both breast-fed and exclusively breast-fed at several of the studied ages, compared with infants of mothers with normal BMI. Maternal overweight can be a barrier to successful breast-feeding due to physical problems from their large size and possibly a decrease in their first phase of milk production( Reference Catalano and Shankar 35 ). Overweight and obesity also increases the risk of caesarean delivery( Reference Catalano and Shankar 35 ) which previous studies have found to be associated with early cessation of full breast-feeding (full breast-feeding: infants could have received water, water-based drinks and fruit juice additional to breast milk)( Reference Häggkvist, Brantsæter and Grjibovski 36 ). A study on predictors of breast-feeding in overweight and obese mothers pointed out that overweight and obese mothers might need additional encouragement to initiate and continue breast-feeding( Reference Krause, Lovelady and Østbye 23 ). This might contribute to reduce the inequities in breast-feeding.
Maternal age
Maternal age has been observed as being significantly associated with duration of both exclusive breast-feeding and any breast-feeding in earlier studies( Reference Kristiansen, Lande and Overby 15 , Reference Biro, Yelland and Brown 37 ). Our results do not support these findings from previous studies in Norway or other industrialized countries. We found that infants of mothers with higher age had lower odds of being exclusively breast-fed at 4 months of age; however, this was not found at 5 months, and for any breast-feeding we found no associations with maternal age. One could speculate whether the older mothers are more aware of the recent discussions regarding potential benefits of introducing food at this age.
Parity
Previously there has been inconsistent results regarding the association between parity and breast-feeding( Reference Thulier and Mercer 27 ). In our study, infants of mothers with previous children had higher odds of being exclusively breast-fed. However, we found no significant association between parity and being breast-fed. Hass et al. found that prior breast-feeding experience was a predictor of continued breast-feeding at 6 weeks postpartum( Reference Hass, Howard and Christopher 38 ).
Maternal smoking
Our study does not support previous results from Norway concerning an association between smoking and breast-feeding( Reference Kristiansen, Lande and Overby 15 ), as we did not find a significant association between smoking and breast-feeding or exclusive breast-feeding. The number of smoking mothers participating in the current study was low and might have affected our results.
Strengths and limitations
Recruitment of the participants was made via social media and through health-care clinics; thus the participants were not selected, but were voluntarily recruited. This led to an uncertainty over who we were able to recruit from those who were potentially eligible and how many who were actually invited. The study sample was dominated by highly educated mothers. The difference in participation between highly and lower educated mothers may have resulted in an underestimation of socio-economic differences in breast-feeding. This leads to a selection bias that weakens the current research’s generalizability to a greater population. The data were self-reported, which reduces the reliability, especially for questions about BMI and breast-feeding. The questionnaires were filled in retrospectively at infant age 6 months, thus asking the parents about their infant’s nutrition in the last 6 months could lead to a recall bias. Further, for the data in Tables 2 and 3 presenting findings for the association between BMI category and breast-feeding, one should acknowledge that there were few underweight participants, so these estimates should be read with caution. Also, we included all participants in the analysis regardless of gestational age. Children born preterm may have difficulties being breast-fed, so one could argue that they should have been excluded from the analysis. We therefore ran a sensitivity test by excluding those born before week 38 and the results did not change (data not shown), so we decided to have them included. A strength to our study is the inclusion of a comparatively large number of participants and the broad use of variables for socio-economic status. The FFQ was developed for Early Food for Future Health and was based on questionnaires used in national surveys in Norway( Reference Øverby, Kristiansen and Frost Andersen 39 ). We acknowledge that other factors can affect breast-feeding such as time of initiating breast-feeding( 40 ), breast-feeding difficulties( Reference Bærug, Laake and Løland 30 ) and postpartum depression( Reference Dias and Figueiredo 41 ); however, we did not have specific information about these conditions in our study except from data on depression symptoms, which could be explored further.
Conclusion
Despite the Norwegian long-term public health policy to reduce social differences in health, factors like maternal education are still associated with inequality in breast-feeding duration. Our results also show a lower rate of exclusively breast-fed infants after 4 months of age compared with previous studies, with only 16·4 % of infants exclusively breast-feeding at 5 months of age. Infants of mothers with overweight/obesity had lower odds of being exclusively breast-fed at 4 months compared with infants of normal-weight mothers in our study. Infants of highly educated mothers had higher odds of being breast-fed compared with infants of lower educated mothers. Breast-feeding promotion should still focus on lower educated mothers to reduce the social gap in diet and health, but should also target overweight and obese mothers to increase the rates of exclusively breast-fed infants in Norway.
Acknowledgements
Financial support: This work was supported by the University of Agder and the Eckbo-foundation. The funders had no role in the design, analysis or writing of this article. Conflict of interest: No conflicts of interest were reported. Authorship: N.C.Ø. and E.R.H. conceived the study. C.H., E.R.H. and N.C.Ø. developed the study. C.H. managed the data collection. V.K.B. analysed the data and drafted the paper. N.C.Ø. contributed with counselling and revision of the paper. All authors commented critically on the paper and helped with interpreting the data. Each author has seen and approved the contents of the submitted manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by The Norwegian Social Science Data Services. Written informed consent was obtained from all subjects.






