Depressive and anxiety disorders are both associated with insomnia. Reference Geoffroy, Oquendo, Courtet, Blanco, Olfson and Peyre1 Studies indicate that over 70% of individuals with major depressive disorder and 50% of those with anxiety disorder experience insomnia. Reference Geoffroy, Hoertel, Etain, Bellivier, Delorme and Limosin2 Conversely, insufficient sleep can also precipitate or even exacerbate various mental disorders. Reference Chellappa and Aeschbach3 Individuals enduring persistent insomnia report a 65% recurrence rate of depression, compared with 13% for those without insomnia. Reference Dombrovski, Cyranowski, Mulsant, Houck, Buysse and Andreescu4 Despite these associations, concurrent management of insomnia alongside depression and anxiety is often overlooked in clinical practice. Reference Sweetman, Lack, Van Ryswyk, Vakulin, Reed and Battersby5,Reference Fang, Tu, Sheng and Shao6 Current expert consensus and clinical guidelines recommend a dual-focus approach when treating these comorbid conditions, and emphasise the importance of addressing both the mental disorders and insomnia, as their coexistence presents distinct clinical manifestations, treatment strategies and prognoses compared with insomnia alone. Reference Sweetman, Lack, Van Ryswyk, Vakulin, Reed and Battersby5,7
Guideline recommendations
Cognitive–behavioural therapy (CBT) is recognised as the first-line treatment for both insomnia and common mental disorders. For chronic insomnia, current guidance recommends CBT for insomnia as the first-line treatment and reserves pharmacologic agents, particularly non-benzodiazepine hypnotics and benzodiazepines, for short-term or refractory use. 8 For depressive disorder, stepped-care guidance recommends psychological therapies (e.g. CBT) as the first-line treatment for mild to moderate episodes, whereas moderate to severe episodes generally warrant antidepressant pharmacotherapy, with or without psychotherapy. Reference Qaseem, Owens, Etxeandia-Ikobaltzeta, Tufte, Cross and Wilt9 For anxiety disorders (e.g. generalised anxiety disorder), disorder-specific CBT is the first-line treatment. Reference Bandelow, Allgulander, Baldwin, da Conceição Costa, Denys and Dilbaz10 However, a lack of resources and trained professionals have resulted in limited availability of CBT, especially at primary healthcare facilities in China, Reference Kyle, Siriwardena, Espie, Yang, Petrou and Ogburn11,Reference Kendrick12 and so pharmacological interventions are commonly and often inappropriately used. Reference Kripke, Langer and Kline13,Reference Fu, Zhu, Gong, Li, Li and Shi14 Approximately 15% of adult out-patient visits at primary healthcare facilities involved a prescription for insomnia. Reference Fu, Zhu, Gong, Li, Li and Shi14 Chinese clinical guideline recommends selective serotonin reuptake inhibitors (SSRIs), selective norepinephrine reuptake inhibitors (SNRIs) and antidepressants with sedative effects (e.g. mirtazapine, trazodone) as the first-line pharmacological options for patients with insomnia comorbid with depressive or anxiety disorders, while reserving non-benzodiazepine hypnotics (also known as Z-drugs) as supplementary medications and benzodiazepines as a last resort. 7
Primary care evidence gap
Primary care is pivotal in the management of common mental disorders. Reference Manning and Jackson15,16 Although prescribing practices for psychotropic medications, such as benzodiazepines, non-benzodiazepine, anxiolytics and antidepressants, have been extensively studied in high-income countries, Reference Chin, Chan, Lam, Wong, Fong and Lo17–Reference Archer, MacNeill, Mars, Turner, Kessler and Wiles19 the appropriateness of their use among patients with insomnia comorbid with common mental disorders at primary healthcare facilities remains underexplored in China. Therefore, we designed this study to evaluate the prescribing rate and appropriateness of psychotropic medications at primary healthcare facilities for patients experiencing insomnia with comorbid depressive or anxiety disorders.
Method
Study design
We conducted a cross-sectional study at all 67 primary healthcare facilities in Dongcheng district, Beijing, China, in 2022. We also assessed the appropriateness of pharmacotherapy based on China’s guideline for the diagnosis and treatment of insomnia comorbid with depression or anxiety in adults. 7 Ethical approval for this study was obtained from the Peking University Institution Review Board (approval number IRB00001052-17016). A waiver of informed consent was granted because the data were deidentified. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for observational studies. Reference von Elm, Altman, Egger, Pocock, Gøtzsche and Vandenbroucke20
Sampling and data collection
Patients identified with insomnia (ICD-10-CM codes F51.0X and G47.0X), combined with depressive disorders (ICD-10-CM codes F32.X, F33.X, F34.1) or anxiety disorders (ICD-10-CM codes F41.X, F40) documented in their diagnoses in 2022 were eligible for inclusion in our study. 21 To improve diagnostic accuracy, we also cross-checked the corresponding Chinese text diagnoses recorded in the electronic health records, to confirm the coding and reduce potential misclassification. Given that primary clinicians may perceived insomnia as a secondary symptom of depressive and anxiety disorders, and the treatment duration for these mental disorders often extends over prolonged periods with common recurrences, Reference Nimmons, Bazo-Alvarez, Avgerinou, Hayes, Osborn and Cooper22,Reference Solomon, Keller, Leon, Mueller, Lavori and Shea23 patients diagnosed with these conditions in separate visits within the same year were also considered comorbid. We extracted data on out-patient visit dates, patient demographics, diagnoses and prescribed medications from the electronic health records. All data were digitally transferred and verified.
Definition
This study categorised anxiolytics, hypnotics and sedatives, antidepressants and antipsychotics as psychotropic medications, using the Anatomical Therapeutic Chemical classification (Supplementary Table 1 available at https://doi.org/10.1192/bjo.2025.10967). 24 We defined guideline-recommended pharmacotherapy based on Chinese guidelines. 7,8 A concise mapping of recommendations to medication classes appears in Supplementary Table 2. Specifically, SSRIs, SNRIs and antidepressants with sedative effects (i.e. mirtazapine, trazodone) are recommended as first-line pharmacotherapies for patients with insomnia comorbid with depressive or anxiety disorders. For patients with insomnia and depression, non-benzodiazepines, should be preferred over benzodiazepines for short-term use when necessary. For those with both insomnia and anxiety, benzodiazepines are recommended for short-term use when insomnia symptoms are more prominent. The fixed-dose combination of flupentixol and melitracen is also recommended by Chinese guidelines. 7 We focused on all visits that contained at least one psychotropic medication and categorised them into three groups based on guideline recommendations: recommended, conditional recommended, and not recommended or not mentioned.
Outcome measures
The primary outcome was the prescribing rate of appropriate psychotropic medications for treating insomnia combined with depressive or anxiety disorders across different age groups. This measure was calculated as the proportion of patient visits that were prescribed with guideline-recommended pharmacotherapy out of total patient visits that were prescribed with at least one psychotropic medication. The second outcome was the prescribing rate of psychotropic medications across different drug classes.
Statistical analysis
We used descriptive statistics to summarise patient characteristics and outcome measures. Continuous variables were reported with means and s.d., whereas categorical variables were expressed as counts and proportions, stratified by patient age group. Statistical analyses were performed with Stata BE (version 18.0 for Windows; StataCorp LLC, College Station, Texas, USA; https://www.stata.com).
Results
Study sample and characteristics
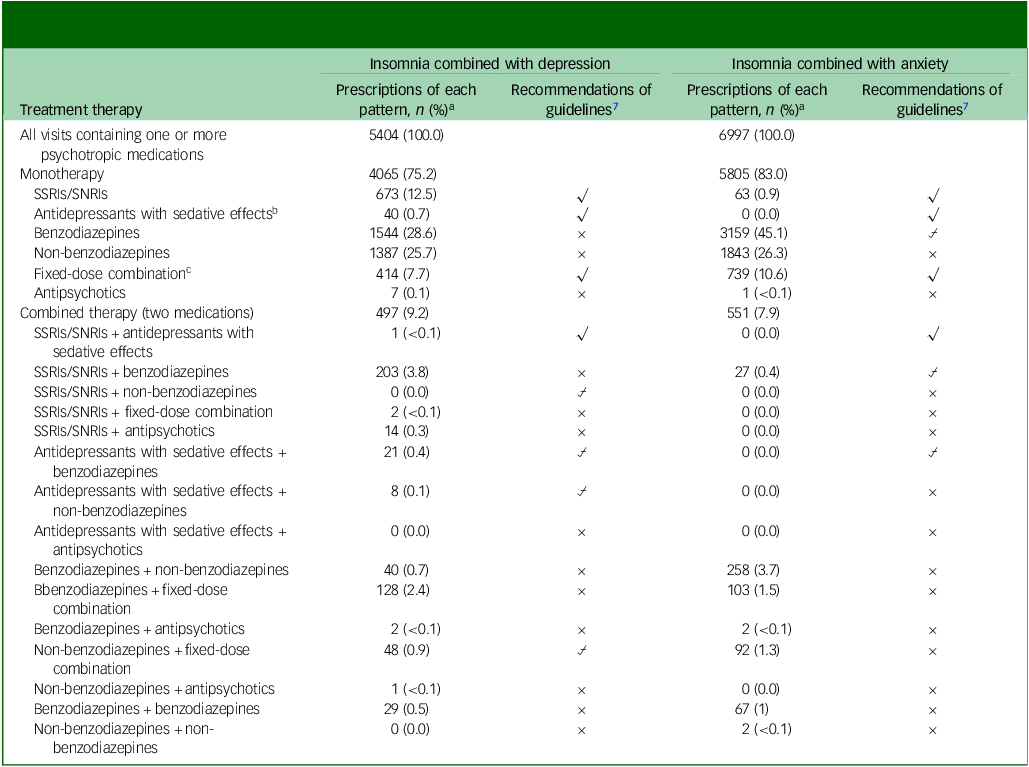
We identified 55 320 adult patients with a diagnosis of insomnia in primary healthcare facilities in Beijing in 2022. Of these, 842 (1.5%) patients had comorbid depressive disorders and 1014 (1.8%) had comorbid anxiety disorders (Supplementary Fig. 1). The mean ages of these two groups were 68.8 (s.d. 12.3) and 66.5 (s.d. 12.3), respectively. The study sample predominantly consisted of women (62.1% for insomnia comorbid depression and 63.2% for insomnia comorbid anxiety) and individuals covered by medical insurance (95.2% for insomnia comorbid depression and 95.3% for insomnia comorbid anxiety). The most common comorbidities were hypertension (66.6% for insomnia comorbid depression and 61.7% for insomnia comorbid anxiety) and diabetes (34.0% for insomnia comorbid depression and 32.1% for insomnia comorbid anxiety; see Table 1). The prevalence of patients with these conditions across different age groups is shown in Supplementary Fig. 2.
Table 1 Characteristics of patients with insomnia combined with depressive or anxiety disorders at primary care facilities, 2022
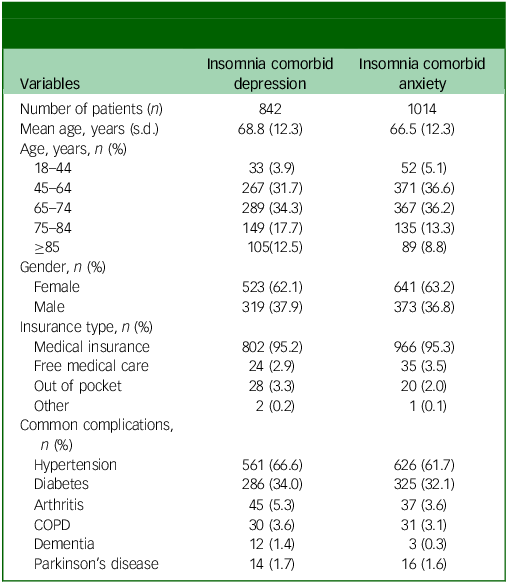
COPD, chronic obstructive pulmonary disease.
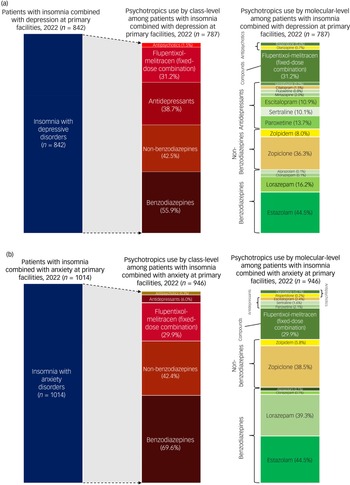
Distribution of prescribed psychotropic medications by drug classes
Across both comorbid groups, more than 90% of patient visits included at least one psychotropic medication, with minimal variation across age groups (Fig. 1). Benzodiazepines were the most frequently prescribed classes (55.9% for insomnia comorbid depression and 69.6% for insomnia comorbid anxiety), followed by non-benzodiazepines (42.5% for insomnia comorbid depression and 42.4% for insomnia comorbid anxiety). SSRIs and flupentixol-melitracen were also commonly used (SSRIs: 36.6% for insomnia comorbid depression and 6.0% for insomnia comorbid anxiety; flupentixol-melitracen: 31.2% for insomnia comorbid depression and 29.9% for insomnia comorbid anxiety). Antidepressants with sedative effects were prescribed infrequently (<5%) (Fig. 2(a) and (b)). The most commonly prescribed benzodiazepines were estazolam (44.5% for insomnia comorbid depression and 44.5% for insomnia comorbid anxiety) and lorazepam (16.2% for insomnia comorbid depression and 39.3% for insomnia comorbid anxiety), whereas zopiclone (36.3% for insomnia comorbid depression and 38.5% for insomnia comorbid anxiety) and zolpidem (8.0% for insomnia comorbid depression and 5.8% for insomnia comorbid anxiety) were most frequently used non-benzodiazepines. SSRIs such as paroxetine, sertraline and escitalopram were more often prescribed for insomnia patients with depression (paroxetine: 13.7%; sertraline: 10.1%; escitalopram: 10.9%) than for those with anxiety (paroxetine: 2.1%; sertraline: 1.6%; escitalopram: 2.4%).
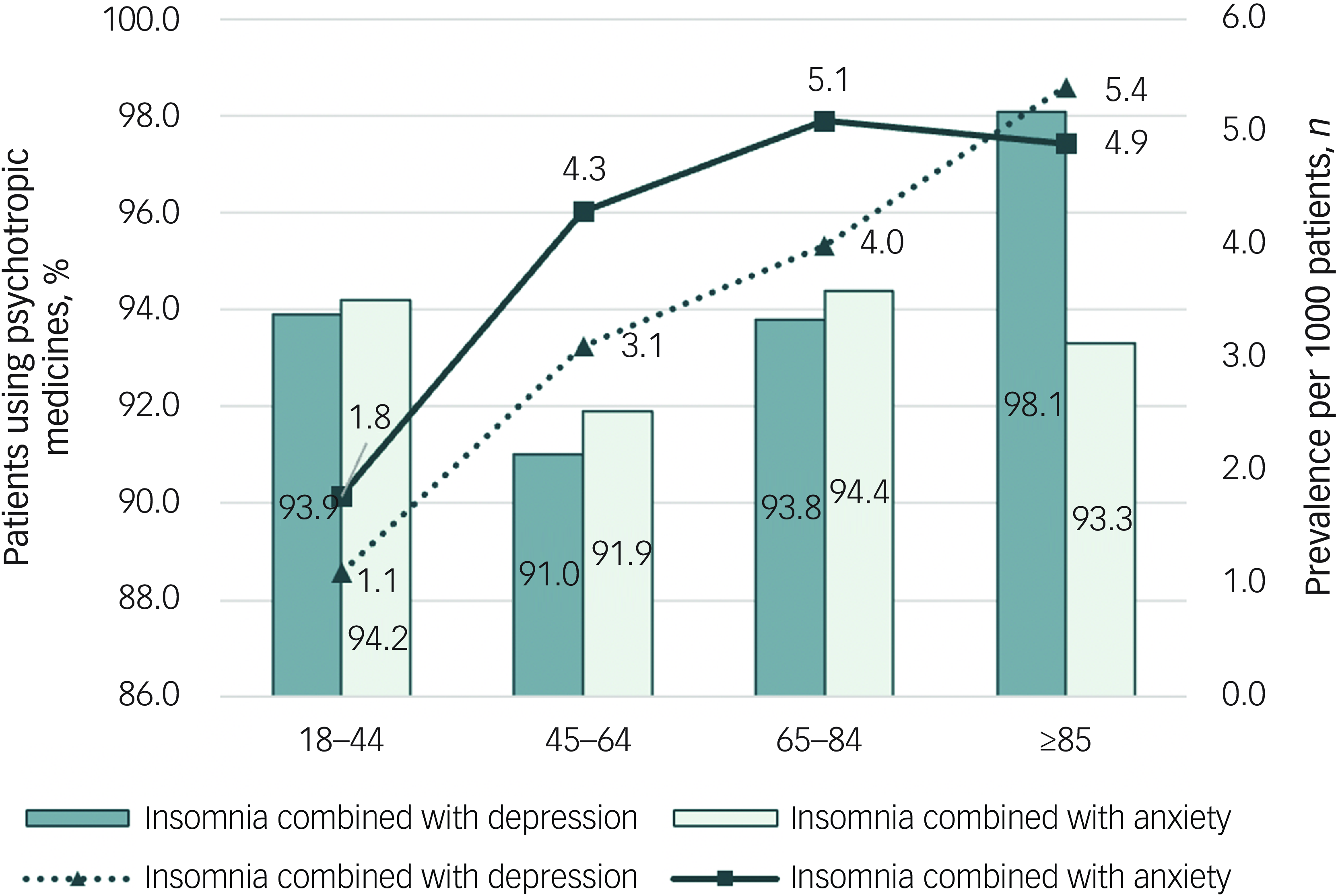
Fig. 1 Prevalence of insomnia comorbid with depressive or anxiety disorders and utilisation of psychotropic medications among patients in primary healthcare facilities in Beijing, 2022.
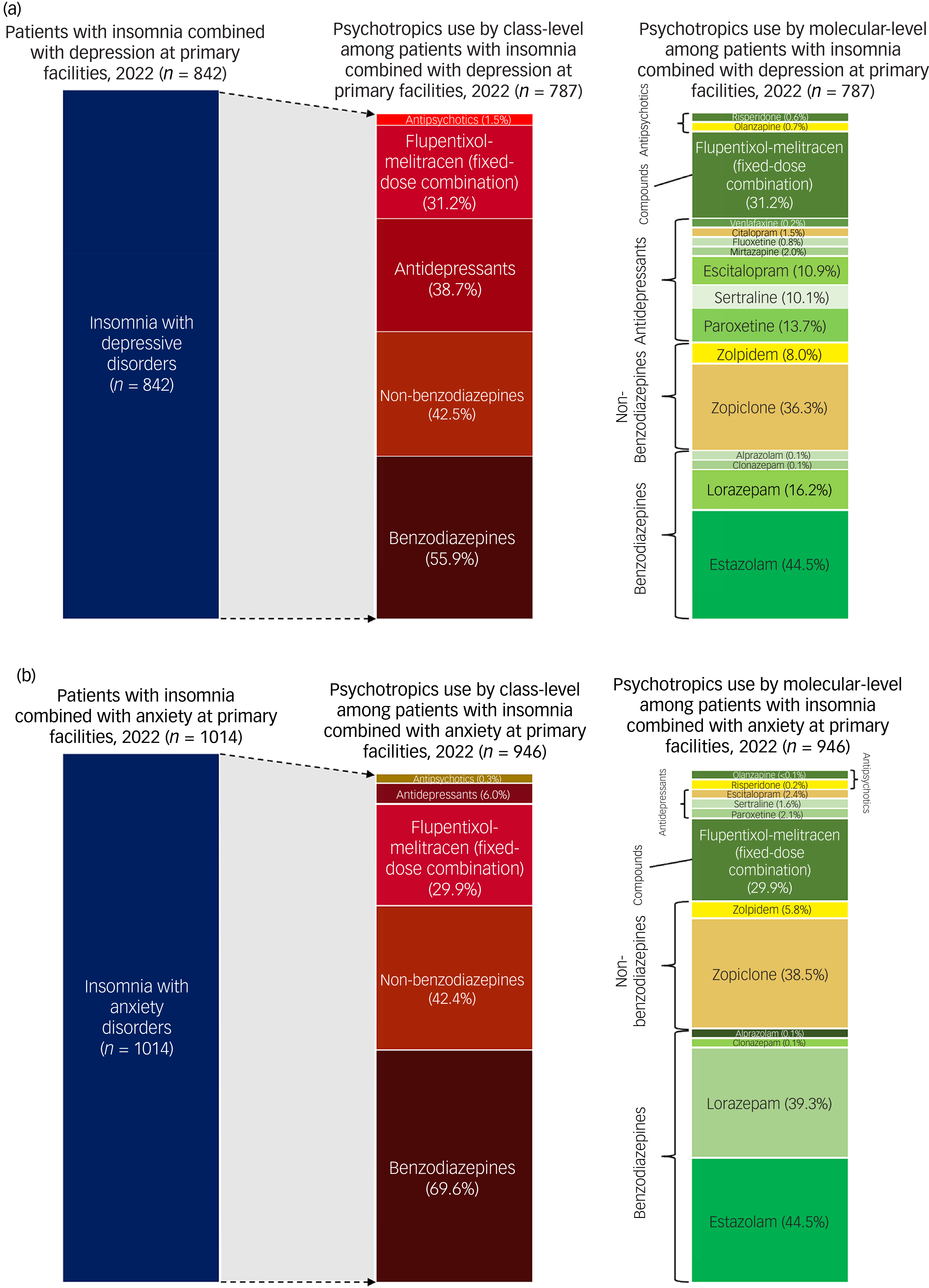
Fig. 2 Distribution of psychotropic medications among patients with (a) insomnia and depressive disorders or (b) insomnia and anxiety disorders, in primary healthcare facilities in Beijing, 2022.
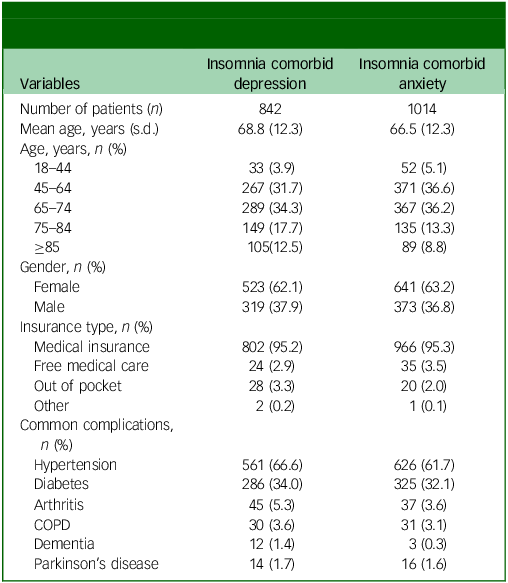
Guideline-recommended pharmacotherapy
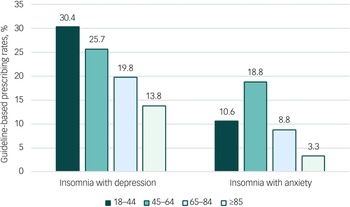
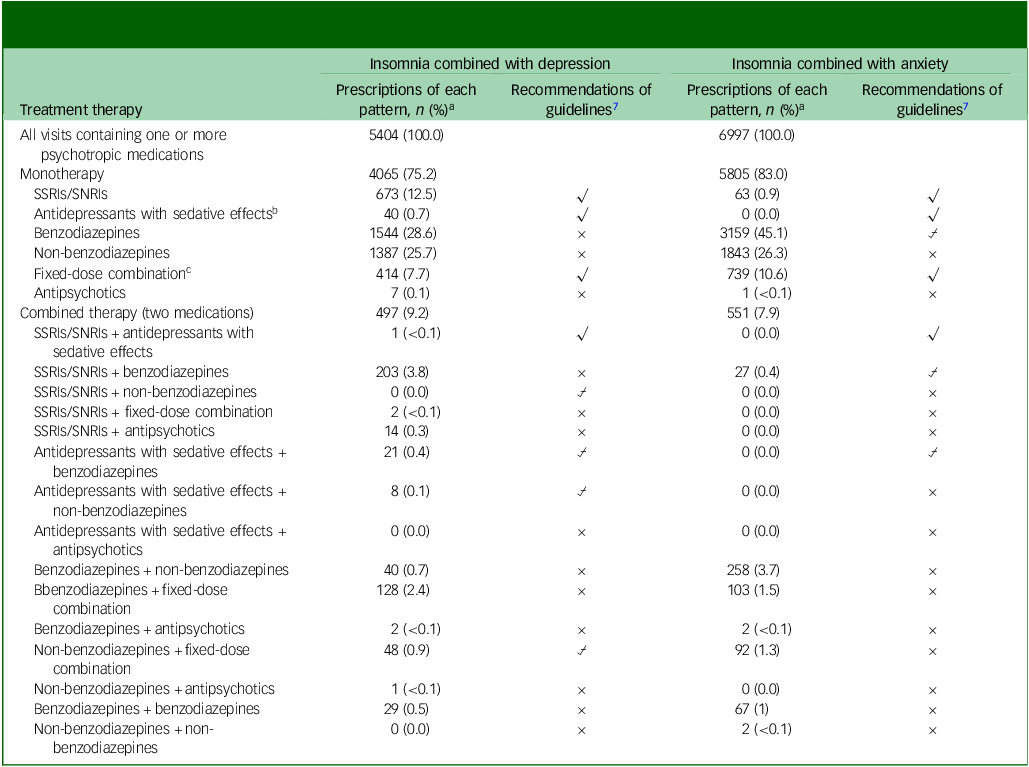
Approximately 24.8 and 17.0% of patients diagnosed with insomnia and either depressive or anxiety disorders received combined therapy, respectively. For patients with insomnia and depression, 29.9% received guideline-recommended pharmacotherapy, whereas this was only 11.5% for those with insomnia and anxiety (Table 2). We also observed a decreasing trend in the prescribing rate of guideline-recommended pharmacotherapy among older adults with insomnia comorbid depression (Fig. 3).
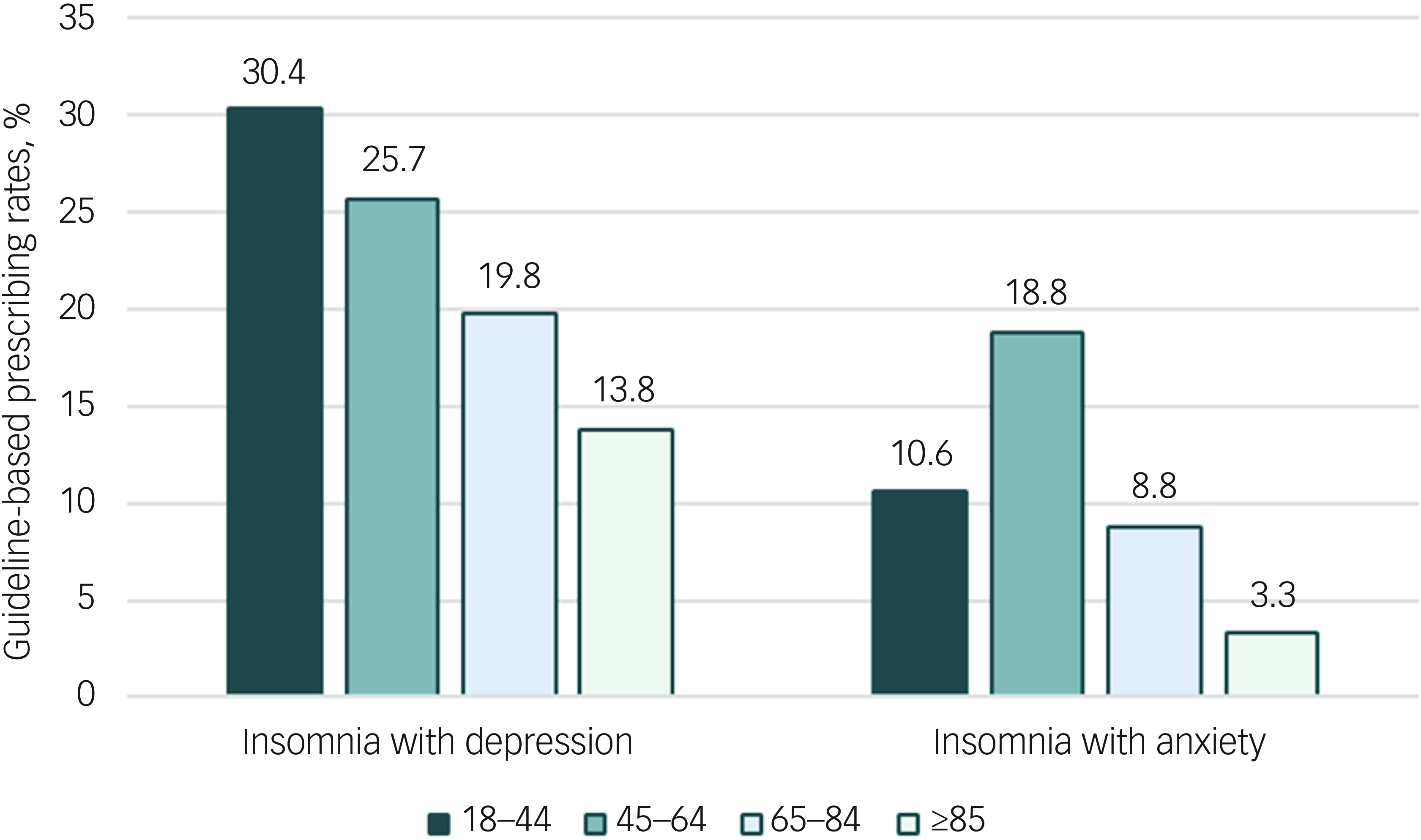
Fig. 3 Proportion of guideline-recommended prescribing for insomnia combined with depressive or anxiety disorders by patient age group in primary care facilities in Beijing, 2022.
Table 2 Guideline recommendations and prescribing patterns of the pharmacotherapy among patients with insomnia combined with depressive or anxiety disorders in primary care facilities in Beijing, 2022
SSRIs, selective serotonin reuptake inhibitors; SNRIs, selective norepinephrine reuptake inhibitors; √, recommended; ×, not recommended or not mentioned; ⍻, conditional recommended.
a. Denominator: the number of visits with at least one psychotropic medication of sample patients.
b. Mirtazapine, trazodone.
c. Flupentixol-melitracen.
Discussion
Our findings revealed that the prescribing rate of guideline-recommended pharmacotherapy was low for patients with insomnia comorbid depressive or anxiety disorders at primary healthcare facilities in China. Benzodiazepines and non-benzodiazepines were the most commonly prescribed medications, despite clinical guidelines prioritising antidepressants with sedative effects, SSRIs and SNRIs, which were less frequently used. 7
The prescribing rates of psychotropic medications for patients with insomnia comorbid with depression or anxiety exceeded 90% overall and across different age groups. Psychotherapy, such as CBT, has been demonstrated to be effective for common mental disorders (e.g. insomnia, depression, anxiety, solely or comorbid), and is recommended as first-line treatment in current clinical guidelines. Reference Qaseem, Owens, Etxeandia-Ikobaltzeta, Tufte, Cross and Wilt9,Reference Bandelow, Allgulander, Baldwin, da Conceição Costa, Denys and Dilbaz10,Reference Qaseem, Kansagara, Forciea, Cooke and Denberg25,Reference Riemann, Baglioni, Bassetti, Bjorvatn, Dolenc Groselj and Ellis26, However, access to psychotherapy remains extremely limited worldwide particularly in primary healthcare facilities, because of inadequate resources and a shortage of trained therapists. Reference Kyle, Siriwardena, Espie, Yang, Petrou and Ogburn11,Reference Kendrick12 Given these constraints, patients with mental disorders were frequently treated only pharmacologically. Reference Kendrick12,Reference Fu, Zhu, Gong, Li, Li and Shi14 Enhancing access to psychotherapy may help reduce unnecessary psychotropic medication use and mitigate associated adverse effects and drug-drug interactions, which is particularly pertinent to older persons. Reference Nimmons, Bazo-Alvarez, Avgerinou, Hayes, Osborn and Cooper22
Our findings highlighted that only 29.9% of patients with comorbid insomnia and depression and 11.5% of those with comorbid anxiety received treatments aligned with guideline recommendations. We observed high overall use of psychotropic medications across all age groups, but guideline-recommended prescribing rates were lower among adults aged ≥65 years, particularly among those with insomnia and depressive disorder. In older populations, sedative hypnotics should generally be avoided because they are associated with falls, delirium, cognitive impairment and dependence. 27 Given the high prevalence of multimorbidity and polypharmacy in older adults, primary care should routinely review medications and screen for cumulative sedative and anticholinergic burden. Expanding access to CBT for insomnia and, when syndromic depressive or anxiety disorders are present, considering antidepressants with sleep-promoting properties may reduce reliance on chronic hypnotics in this high-risk group.
Another major concern is the high prescribing rates of non-benzodiazepines and benzodiazepines, both of which should be used with caution according to the Chinese guideline. 7 However, our results showed that non-benzodiazepines were prescribed for 42.5% of patients with insomnia comorbid depression and 42.4% of those with comorbid anxiety, representing substantial inappropriate use. Moreover, although benzodiazepines were considered a last resort by guidelines because of their high risk of inducing cognitive dysfunction and falls, Reference Billioti de Gage, Moride, Ducruet, Kurth, Verdoux and Tournier28–Reference Maust, Lin, Goldstick, Haffajee, Brownlee and Bohnert30 they were prescribed at alarmingly high rates in both conditions (55.9 and 69.6%), far exceeding rates reported in the UK (14.5–27.1%). Reference Nimmons, Bazo-Alvarez, Avgerinou, Hayes, Osborn and Cooper22 This pattern of high non-benzodiazepine and benzodiazepine use, particularly noted in patients aged >85 years, has also been reported in our previous research focusing on insomnia treatment in primary care. Reference Fu, Zhu, Gong, Li, Li and Shi14 This pervasive issue may stem from clinicians’ limited knowledge of guideline recommendations in managing comorbid common mental disorders. Reference Fu, Zhu, Gong, Li, Li and Shi14 Tailored training programmes are therefore necessary to promote evidence-based treatment at primary healthcare facilities and reduce excessive use of benzodiazepines, especially among older adults.
The prevalent use of benzodiazepines or non-benzodiazepines as monotherapy in treating comorbid conditions suggests an oversight of depressive and anxiety symptoms by primary clinicians. This issue may primarily arise from primary care physicians’ unfamiliarity with the guidelines as discussed earlier, but it might also be influenced by patients’ expectations. Reference Sirdifield, Anthierens, Creupelandt, Chipchase, Christiaens and Siriwardena31 Some patients who initiated appropriate treatment at specialty hospitals or tertiary hospitals may seek stronger sedative hypnotics at primary care. This highlights the need for primary clinicians to be trained to meticulously review patients’ psychotropic medication use during consultations and make necessary medication reconciliation to ensure more appropriate prescribing and patient safety. Reference Almanasreh, Moles and Chen32 Establishing a shared network system among different healthcare levels to track diagnosis and treatment history could facilitate more comprehensive care. Reference Tian, Chen and Bai33 Future studies using regional databases that link different levels of healthcare institutions are need to better understand cross-setting differences in pharmacotherapy for insomnia comorbid with depression or anxiety.
Our research also showed prevalent use of flupentixol-melitracen in primary healthcare facilities in China, a pattern not observed in other countries. Reference Nimmons, Bazo-Alvarez, Avgerinou, Hayes, Osborn and Cooper22,Reference Tanana, Harrison, Nishtala and Chen34 Flupentixol-melitracen is a fixed-dose combination of a typical antipsychotic and melitracen, a tricyclic antidepressant. It has not been marketed in many high-income countries (e.g. USA, Canada, Japan, Denmark), and was banned by India’s health ministry in 2015 because of safety concerns regarding fixed-dose combinations of psychotropic agents. Reference Bhaumik35 Despite these international reservations, flupentixol-melitracen continues to be widely used in China, where it has been marketed since the late 1990s. Although Chinese guidelines recognise its efficacy for treating depression and anxiety, they offer limited guidance on its use in managing insomnia comorbid with depression or anxiety. The substantial use of this combination in the absence of definitive and conclusive evidence raises concerns about potential harms. Rigorous clinical research is urgently needed to establish clear evidence to inform and refine future treatment recommendations. Further, Chinese guidelines should provide more specific and concrete recommendations for flupentixol-melitracen to support safer clinical practice and improve patient outcomes.
Several limitations of this study should be noted. First, the data sources contained only primary healthcare facilities, whereas the treatment of depression and anxiety might predominantly occur in specialised or tertiary hospitals in China. This may explain the relatively small sample size of patients with insomnia comorbid depression or anxiety in our study, limiting its generalisability. Future region-wide, cross-setting linked studies are needed to assess duration and trajectories of care. Second, potential inaccuracy or inconsistency of diagnostic coding in the database may have affected case identification and inclusion. However, we also used the corresponding Chinese text diagnoses recorded in the electronic health records, which helped to partially mitigate this uncertainty in coding. Third, the study was conducted in Dongcheng, a district in central Beijing with higher economic status and superior medical resources. Consequently, the findings may not be fully representative of the broader population of patients in primary care across Beijing. Fourth, we restricted our study period to 2022 to maximise data completeness and coding stability. A single-year analysis limits assessment of trends such as seasonality or secular shifts.
In conclusion, the prescribing rate of guideline-recommended pharmacotherapy for patients with insomnia comorbid with depressive or anxiety disorders was considerably low in Chinese primary healthcare facilities, primarily because of the excessive use of benzodiazepines and non-benzodiazepines. These findings highlight the need to reduce the use of high-risk medications and to facilitate evidence-based treatment for complex mental health conditions at primary care, especially for older adults.
Supplementary material
The supplementary material is available online at https://doi.org/10.1192/bjo.2025.10967
Data availability
The data that support the findings of this study are available from the corresponding author, X.G., upon reasonable request.
Acknowledgement
We would like to thank the Dongcheng Health Service Management Center (DHSMC) for providing support for data collection of this study. The DHSMC was not compensated for this contribution.
Author contributions
M.F., C.L. and X.G. conceptualised the study and undertook the analyses. C.L. and X.Z. wrote the original draft of the manuscript. Z.G. and K.L. conducted a review of the models and analyses. Y.Z. did the work of data curation. M.F. critically revised the drafts for important intellectual contents. Y.D. polished the final draft of the manuscript. F.W. and L.S. supervised the project. All authors refined and approved the final version of manuscript. The corresponding author confirms that all listed authors meet authorship criteria and that no individuals meeting the criteria have been omitted.
Funding
This work was supported by National Natural Science Foundation of China (grant number 72304011 to M.F.).
Declaration of interest
None.




eLetters
No eLetters have been published for this article.