Statement of Research Significance
Research Question(s) or Topic(s): We explored how aspects of neuropsychological functioning relate to suicidal thoughts in people with moderate–severe traumatic brain injury. Main Findings: Participants with suicidal thoughts after moderate–severe traumatic brain injury often reported difficulties in managing their emotions, using unhealthy coping strategies, such as avoiding problems or self-blame, and experiencing cognitive difficulties. Lower resilience – or a reduced ability to “thrive in the face of adversity” – was also associated with greater suicidal thoughts. These factors appeared to be linked to suicidal thoughts primarily through their associations with symptoms of depression and anxiety. However, participants who used healthy coping strategies, like problem-solving, or who performed well on cognitive tests did not necessarily experience fewer suicidal thoughts. Study Contributions: Our study offers insights into factors that may contribute to suicidal thoughts in people with moderate–severe traumatic brain injury, highlighting considerations for suicide risk assessment and potential targets for future intervention efforts.
Introduction
Suicidal ideation (SI) and suicide attempts are significantly more common in individuals with traumatic brain injury (TBI) than in the general population (Chen et al., Reference Chen, Chi, Niu, Gao, Mei, Zhao, Hu, Zhao and Ma2022; Ineson et al., Reference Ineson, Erlangsen, Nordentoft, Benros and Madsen2023; Lu et al., Reference Lu, Wu, Zhang, Zhang, Lu and Wu2020). Among individuals with predominately moderate–severe TBI, SI has been reported to increase the risk of a future suicide attempt approximately fivefold compared to those without ideation (Simpson & Tate, Reference Simpson and Tate2002). Psychiatric disorders are strong predictors of suicidality after TBI (Izzy et al., Reference Izzy, Chen, Tahir, Grashow, Radmanesh, Cote, Yahya, Dhand, Taylor, Shih, Albastaki, Rovito, Snider, Whalen, Nathan, Miller, Speizer, Baggish, Weisskopf and Zafonte2022; McIntire et al., Reference McIntire, Crawford, Perrin, Sestak, Aman, Walter, Page, Wen, Randolph, Brunner, Novack and Niemeier2021), but they are estimated to account for only about 30% of the increased risk (Miller et al., Reference Miller, Zhou, Peterson, Swedo, Holland and Kresnow2023). This suggests that other psychological and cognitive factors may contribute to suicide risk after TBI and warrant investigation.
Emotional lability and detachment
Emotion-processing difficulties, such as emotional lability (intense and rapid shifts in emotions) and emotional detachment (being emotionally distant and reserved; Simms et al., Reference Simms, Goldberg, Roberts, Watson, Welte and Rotterman2011), have been linked to suicidality in the general population (Hemming et al., Reference Hemming, Taylor, Haddock, Shaw and Pratt2019; Turton et al., Reference Turton, Berry, Danquah and Pratt2021). Emotional lability, for example, may heighten vulnerability to suicidality by amplifying the intensity and volatility of negative affective states, potentially increasing impulsive or reactive suicidal thoughts in moments of distress (Links et al., Reference Links, Boggild and Sarin2000). Furthermore, emotional detachment and related experiences are thought to disrupt emotional regulation by reducing flexibility in emotional responses and diminishing awareness of internal states, leading to increased psychological distress (Brett et al., Reference Brett, Zarei, Preece and Becerra2025; Carpenter & Trull, Reference Carpenter and Trull2013; Preece et al., Reference Preece, Becerra, Allan, Robinson and Dandy2017). Difficulties processing emotions are especially common after moderate–severe TBI (Arciniegas & Wortzel, Reference Arciniegas, Wortzel, Silver, McAllister and Arciniegas2018; Carmichael et al., Reference Carmichael, Ponsford, Gould, Tiego, Forbes, Kotov, Fornito and Spitz2025a; Fynn et al., Reference Fynn, Gignac, Becerra, Pestell and Weinborn2021), being typically attributed to damage in frontal and limbic brain regions critical for emotion regulation and inhibitory control (Becerra et al., Reference Becerra, Amos and Jongenelis2002; McAllister, Reference McAllister2011; Hogeveen et al., Reference Hogeveen, Bird, Chau, Krueger and Grafman2016). Given the established link between emotional dysregulation and suicidality in the general population, these changes post-TBI may contribute to elevated suicide risk in this group.
Although no studies have specifically examined the associations of emotional lability or detachment with suicidality following TBI, a related construct – alexithymia, or a difficulty identifying and describing one’s emotions (Preece et al., Reference Preece, Becerra, Allan, Robinson and Dandy2017) – has been investigated. While alexithymia and emotional detachment both involve altered emotion processing, alexithymia reflects a fundamental difficulty in recognizing emotions, whereas emotional detachment may involve intact emotion recognition but a tendency to nevertheless suppress or disengage from emotional experiences. Among individuals with TBI, alexithymia has been linked to greater psychopathology and SI (Neumann et al., Reference Neumann, Hammond, Sander, Bogner, Bushnik, Finn, Chung, Klyce, Sevigny and Ketchum2025; Henry et al., Reference Henry, Phillips, Crawford, Theodorou and Summers2006; Wood & Williams, Reference Wood and Williams2007; Wood et al., Reference Wood, Williams and Lewis2010). Moreover, a longitudinal study found that alexithymia one year post-injury predicted poorer emotional outcomes and greater SI at two years (Neumann et al., Reference Neumann, Hammond, Sander, Bogner, Bushnik, Finn, Chung, Klyce, Sevigny and Ketchum2024a). These findings support the broader relevance of altered emotion processing in post-TBI suicidality and highlight the need to examine how emotional lability and emotional detachment, as distinct from alexithymia, may also be associated with SI in this population.
Coping and resilience
Coping and resilience are additional psychological factors that may be associated with suicidality in individuals with TBI. Coping can be broadly categorized as more healthy/adaptive (e.g., self-soothing, seeking social support) or unhealthy/non-productive (e.g., self-blame, substance use) depending on their potential for long-term adverse consequences (Stallman, Reference Stallman2020). Resilience, in contrast, reflects a broader capacity for psychological adaptation, encompassing not only the use of adaptive coping strategies but also factors such as optimism, self-efficacy, and external resources (e.g., social support, financial stability) that facilitate recovery from adversity (Connor & Davidson, Reference Connor and Davidson2003). As moderate–severe TBI often results in profound life changes, both coping and resilience are likely to play a crucial role in psychological adjustment and recovery (Rabinowitz & Arnett, Reference Rabinowitz and Arnett2018).
There is some evidence from individuals with TBI (Wolters Gregório et al., Reference Wolters Gregório, Gould, Spitz, Van Heugten and Ponsford2014) and informants (Dawson et al., Reference Dawson, Catanzaro, Firestone, Schwartz and Stuss2006) that coping styles may change toward increased maladaptive coping following TBI. For example, Wolters Gregório and colleagues (Reference Wolters Gregório, Gould, Spitz, Van Heugten and Ponsford2014) assessed self-reported coping at multiple timepoints following moderate–severe TBI, including an initial assessment during inpatient admission in which patients retrospectively reported on their pre-injury coping styles. Across follow-up assessments up to three years post-injury, participants reported increased reliance on non-productive coping strategies, such as self-blame and wishful thinking – patterns which are associated with increased psychopathology (Anson & Ponsford, Reference Anson and Ponsford2006a; Bryant et al., Reference Bryant, Marosszeky, Crooks, Baguley and Gurka2000; Curran et al., Reference Curran, Ponsford and Crowe2000; Gould et al., Reference Gould, Ponsford, Johnston and Schönberger2011a; Hoofien et al., Reference Hoofien, Gilboa, Vakil and Donovick2001; Spitz et al., Reference Spitz, Schönberger and Ponsford2013; Tomberg et al., Reference Tomberg, Toomela, Ennok and Tikk2007; Wolters et al., Reference Wolters, Stapert, Brands and Van Heugten2010; Wolters Gregório et al., Reference Wolters Gregório, Gould, Spitz, Van Heugten and Ponsford2014). Similar to coping, lower psychological resilience after TBI has been linked to higher psychopathology, lower life satisfaction, and greater functional disability (Hanks et al., Reference Hanks, Rapport, Waldron Perrine and Millis2016; Paasila et al., Reference Paasila, Smith, Daher and Simpson2022; Rapport et al., Reference Rapport, Wong and Hanks2020; Sima et al., Reference Sima, Yu, Marwitz, Kolakowsky-Hayner, Felix, Bergquist, Whiteneck, Kreutzer and Johnson-Greene2019; Wardlaw et al., Reference Wardlaw, Hicks, Sherer and Ponsford2018).
While no study has directly examined coping strategies in relation to suicidality after TBI, preliminary evidence suggests resilience may be protective. Paasila and colleagues (Reference Paasila, Smith, Daher and Simpson2022) found that higher resilience was associated with lower SI post-TBI. However, although the study included a measure of depression, it did not assess whether the relationship between resilience and SI persisted after accounting for depression. This leaves open the possibility that this relationship operates indirectly through emotional distress, such as symptoms of depression and anxiety. Given evidence of the protective roles of adaptive, problem-focused coping and resilience against suicidality in other populations (Darvishi et al., Reference Darvishi, Farhadi, Azmi-Naei and Poorolajal2023; Sher, Reference Sher2019), further research is needed to clarify their contributions to suicide risk following TBI.
Cognitive functioning
Lastly, cognitive impairments across multiple domains – particularly working memory, executive functioning, and reward-based learning – have been linked to suicidality in psychiatric populations (Le et al., Reference Le, Wong, Haikazian, Johnson, Badulescu, Kwan, Gill, Di Vincenzo, Rosenblat, Mansur, Teopiz, Rhee, Ho, Liao, Cao, Schweinfurth-Keck, Vinberg, Grande, Phan and McIntyre2024). Following a moderate–severe TBI, individuals commonly report numerous subjective or perceived cognitive difficulties in daily life (Borgen et al., Reference Borgen, Kleffelgård, Hauger, Forslund, Søberg, Andelic, Sveen, Winter, Løvstad and Røe2022; Jourdan et al., Reference Jourdan, Bayen, Pradat-Diehl, Ghout, Darnoux, Azerad, Vallat-Azouvi, Charanton, Aegerter, Ruet and Azouvi2016; Ponsford et al., Reference Ponsford, Downing, Olver, Ponsford, Acher, Carty and Spitz2014) and also demonstrate objective or performance-based deficits on numerous neuropsychological tests (Cristofori & Levin, Reference Cristofori and Levin2015). Speculatively, such impairments may be associated with suicidality after TBI by reducing problem-solving ability (Barnes et al., Reference Barnes, Monteith, Gerard, Hoffberg, Homaifar and Brenner2017), contributing to functional disability (Perrin et al., Reference Perrin, Klyce, Fisher, Juengst, Hammond, Gary, Niemeier, Bergquist, Bombardier, Rabinowitz, Zafonte and Wagner2022), or through shared neurobiological mechanisms involving overlapping differences in the brain. For example, Yurgelun-Todd and colleagues (Reference Yurgelun-Todd, Bueler, McGlade, Churchwell, Brenner and Lopez-Larson2011) found that SI and perceived cognitive impairments related to impulsivity were intercorrelated in individuals with TBI, with both linked to poorer white matter integrity in frontal regions – structural abnormalities that were more pronounced in the TBI group than in controls.
Although subjective cognitive concerns are more consistently and strongly associated with post-TBI psychopathology than objectively measured impairments (Byrne et al., Reference Byrne, Coetzer and Addy2017; Draper & Ponsford, Reference Draper and Ponsford2009; Fann et al., Reference Fann, Katon, Uomoto and Esselman1995; Grauwmeijer et al., Reference Grauwmeijer, Heijenbrok-Kal, Peppel, Hartjes, Haitsma, De Koning and Ribbers2018; Satz et al., Reference Satz, Forney, Zaucha, Asarnow, Light, McCleary, Levin, Kelly, Bergsneider, Hovda, Martin, Namerow and Becker1998; Vos et al., Reference Vos, Williams, Poritz, Ngan, Leon-Novelo and Sherer2020), individuals with TBI who have psychiatric symptoms also tend to perform worse on neuropsychological testing (Gould et al., Reference Gould, Ponsford and Spitz2014; Keatley et al., Reference Keatley, Bombardier, Watson, Kumar, Novack, Monden and Dams-O’Connor2023; see review by Uiterwijk et al., Reference Uiterwijk, Stargatt, Humphrey and Crowe2022). This suggests that both perceived and objectively measured impairments in cognitive functioning may be relevant to post-injury mental health. While research directly linking cognitive impairment to suicidality after TBI is limited, emerging evidence points to a potential association. Veterans with TBI and a history of suicide attempts have shown objectively poorer decision-making and more perseverative errors on the Iowa Gambling Task – indicative of executive dysfunction, particularly in cognitive flexibility and feedback-based learning (Brenner et al., Reference Brenner, Bahraini, Homaifar, Monteith, Nagamoto, Dorsey-Holliman and Forster2015; Homaifar et al., Reference Homaifar, Brenner, Forster and Nagamoto2012). However, no study has yet examined the relationship between suicidality and both subjective and objective cognitive impairments across multiple cognitive domains in individuals with TBI, highlighting a gap in the literature.
Current study
Building on previous research, this study aimed to investigate psychological and cognitive correlates of SI in individuals with moderate–severe TBI. It was hypothesized that SI would be positively associated with emotional lability, emotional detachment, non-productive coping, and both subjective and objective cognitive difficulties. Conversely, SI was expected to show negative associations with adaptive coping and psychological resilience. In recognition that psychiatric disorders are among the strongest risk factors for suicidality, as an exploratory analysis, this study also considered whether the associations between these psychological and cognitive factors and SI could be accounted for by symptoms of depression and anxiety.
Method
The data were obtained in compliance with the Monash University Human Research Ethics Committee (#27729) and Helsinki Declaration.
Study design and participants
Data were collected as part of a follow-up to a larger project at the Monash-Epworth Rehabilitation Research Centre (MERRC) on psychopathology after TBI (Carmichael et al., Reference Carmichael, Ponsford, Gould, Tiego, Forbes, Kotov, Fornito and Spitz2025a). Participants were recruited via email or phone call from a longitudinal database of patients admitted to Epworth HealthCare (Ponsford et al., Reference Ponsford, Downing, Olver, Ponsford, Acher, Carty and Spitz2014), a rehabilitation hospital in Melbourne, Australia. Eligibility criteria for the larger baseline study included age 18–80 and having a moderate–severe TBI (but no other neurological conditions) as defined by the Mayo Classification System (Malec et al., Reference Malec, Brown, Leibson, Flaada, Mandrekar, Diehl and Perkins2007). Participants were classified as having a moderate–severe TBI, and therefore eligible for the study, if they met at least one of three Mayo criteria: a worst score of ≤ 12 on the Glasgow Coma Scale (GCS) within the first 24 hours after injury, ≥ 1 day of post-traumatic amnesia (PTA), and intracranial abnormality detected on computed tomography (CT) scan. For example, participants with a GCS of 13–15 could still meet eligibility if they had another qualifying indicator for moderate–severe TBI, such as PTA ≥ 1 day.
In the baseline study, participants completed a range of questionnaires about their psychiatric functioning. To answer additional research questions on the relationship between psychiatric and cognitive functioning after TBI, we conducted a follow-up assessment with a subset of the original participants, using the same psychiatric questionnaires and adding new measures of coping, resilience, and cognitive functioning. This paper presents a secondary analysis of those follow-up data, focused specifically on SI and its psychological and cognitive correlates.
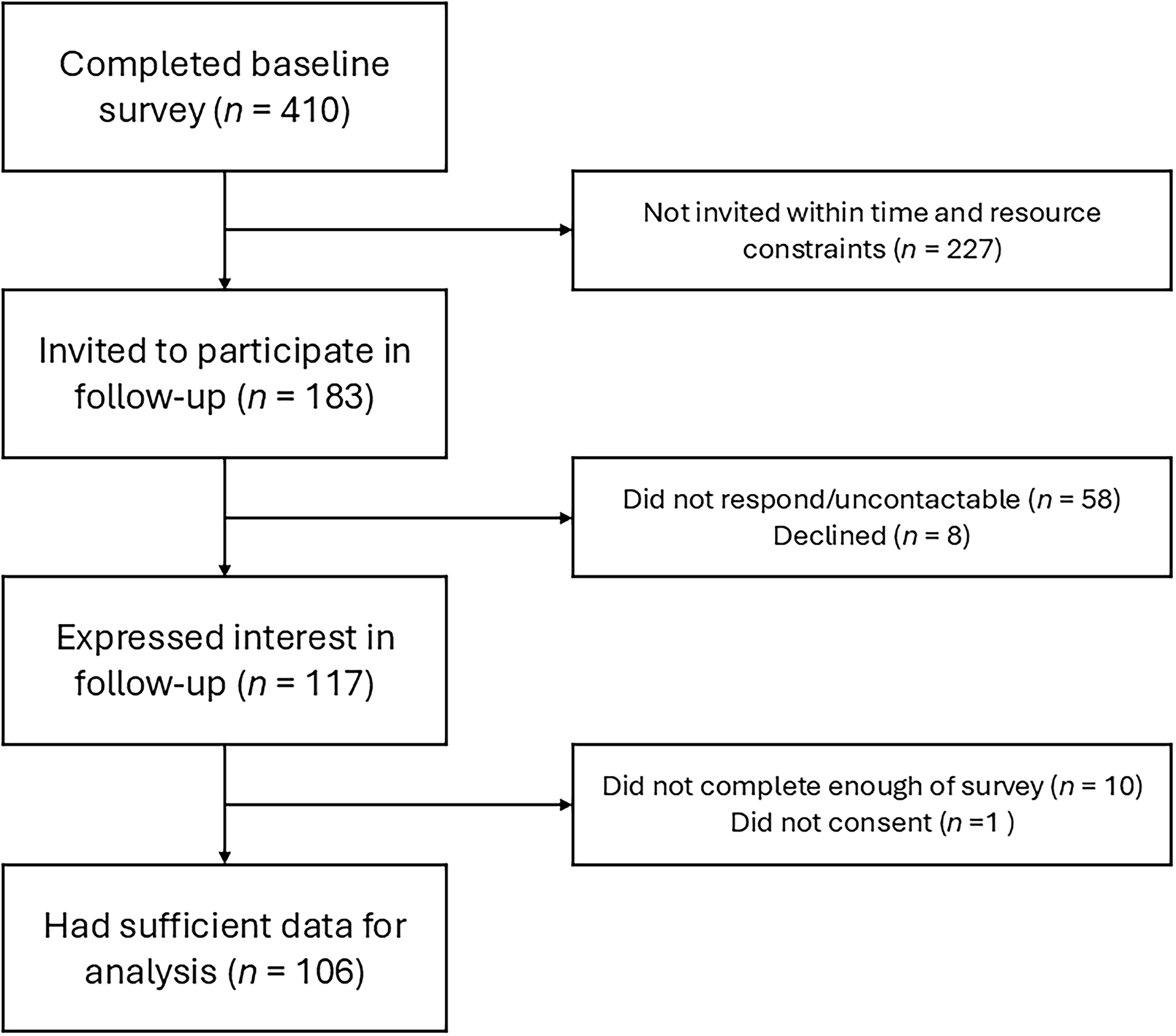
The participant recruitment flowchart is presented in Figure 1. Of the 410 participants who completed the baseline psychiatric assessment between March 2021 and August 2022 (Carmichael et al., Reference Carmichael, Ponsford, Gould, Tiego, Forbes, Kotov, Fornito and Spitz2025a), 183 were invited in chronological order, starting with those who completed the baseline survey earliest, to participate in the follow-up study from January 2024 to October 2024. Recruitment was informed by an a priori goal of obtaining a sample size of 100 for the primary aims of the broader follow-up study, which focused on examining pairwise associations between psychopathology and cognitive functioning following TBI (Samiotis et al., in preparation), not SI specifically. The primary analyses were planned as part of a PhD project with a fixed timeline and supported by a time-limited research grant. As such, the sample size was pragmatically constrained by available time and funding (Lakens, Reference Lakens2022), and it was not feasible to reassess the full baseline cohort.

Figure 1. Participant recruitment flowchart. Note: “Not invited within time and resource constraints” refers to baseline participants who had not yet reached the top of the chronological list at the time of completing this study’s analyses.
Of those invited, 117 expressed interest, and 106 participants provided complete data on SI, emotional distress, and at least one other psychological or cognitive variable of interest (n = 86–104 for other variables). These 106 participants comprised the sample for this report, and importantly, they did not significantly differ on any sociodemographic or injury variables from the 304 other baseline participants (see Supplementary Table S1). We also compared the current study sample to the broader MERRC cohort of individuals aged 18 years and over who were recruited from inpatient rehabilitation following a TBI (n = 4,502). Several statistically significant differences were observed, with small-to-medium effect sizes. Compared to the broader MERRC cohort, the current participants (n = 106) had more years of education at the time of injury (M difference = 1.40 years of education, p < .001, d = 0.54), were more likely to be employed or studying at the time of injury (91% vs. 70%, p < .001, h = 0.53), had a shorter duration of PTA (M difference = 5.06 days, p = .013, d = 0.15), and were fewer years post-injury (M difference = 4.88 years, p < .001, d = 0.45). No significant differences were observed in age at injury, sex, pre-injury relationship status, pre-injury mental health treatment, acute CT brain findings, or worst 24-hour GCS score (p-values > .05).
Procedure and measures
All 106 participants completed the psychological questionnaires (1.5–2 hours), and a subset of 92 completed a brief cognitive assessment (15–30 minutes). The majority completed the survey independently online (n = 104; 98.11%), while one individual completed it via teleconference and another in-person with a researcher. All cognitive assessments were conducted over the phone by one of two clinical neuropsychology PhD trainees (A.S. and J.-Y.C.).
A detailed summary of all measures and evidence of their validity is provided in Supplementary Appendix S1. SI experienced in the previous two weeks was measured using the Inventory of Depression and Anxiety Symptoms – Expanded Version (IDAS-II; Watson et al., Reference Watson, O’Hara, Naragon-Gainey, Koffel, Chmielewski, Kotov, Stasik and Ruggero2012). The IDAS-II includes a six-item Suicidality scale. Factor analysis conducted on the baseline sample of individuals with moderate–severe TBI revealed that this scale is not unidimensional but instead measures two distinct factors: one measuring SI and another measuring self-harm (Carmichael et al., Reference Carmichael, Ponsford, Gould, Tiego, Forbes, Kotov, Fornito and Spitz2025a). The self-harm factor does not explicitly reference death or suicide and therefore also encompasses non-suicidal self-injury. Consequently, in this study, SI was measured using a subset of three items from the IDAS-II Suicidality scale: Item 13 (“I had thoughts of suicide”), Item 33 (“I thought that the world better off without me”), and Item 46 (“I thought about my own death”). This three-item index of SI showed good internal consistency within the current sample (ω = .84).
Briefly, regarding the other questionnaire data, emotional distress, encompassing both symptoms of anxiety and depression, was measured using the total score of the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, Reference Zigmond and Snaith1983). Emotional lability and detachment were assessed using the corresponding scales from the Comprehensive Assessment of Traits Relevant to Personality Disorders – Static Form (CAT-PD-SF; Simms et al., Reference Simms, Goldberg, Roberts, Watson, Welte and Rotterman2011). Coping was evaluated with the Adaptive Coping and Non-Productive Coping subscales of the original short-form Coping Scale for Adults (Fredenberg & Lewis, Reference Fredenberg and Lewis1997), and psychological resilience was measured using the 10-item Connor–Davidson Resilience Scale (CD-RISC 10; Campbell-Sills & Stein, Reference Campbell-Sills and Stein2007). Subjective cognitive functioning was assessed using the Cognitive Problems scale from the CAT-PD-SF and the Behavioral Regulation Index (BRI) and Metacognition Index (MI) from the self-report Behavior Rating Inventory of Executive Function – Adult (BRIEF-A; Roth et al., Reference Roth, Isquith and Gioia2005).
Finally, most participants also underwent an objective screen of cognitive functioning using Form A of the Brief Test of Adult Cognition by Telephone (BTACT; Tun & Lachman, Reference Tun and Lachman2006). The BTACT has been validated for use with individuals with moderate–severe TBI (Nelson et al., Reference Nelson, Barber, Temkin, Dams-O’Connor, Dikmen, Giacino, Kramer, Levin, McCrea, Whyte, Bodien, Yue and Manley2021) and includes seven phone-administered subtests adapted from established neuropsychological tests, measuring verbal encoding (Word List Immediate Recall), verbal episodic memory (Word List Delayed Recall), verbal working memory (Digits Backward), verbal idea generation (Category Fluency), inductive reasoning (Number Series), and verbal processing speed (Backward Counting). The seventh subtest, Stop and Go Switch, was excluded from analysis due to a ceiling effect (i.e., it was too easy for participants: Z skew = –5.62 and –6.81 for the reverse and switching conditions, respectively); this is consistent with prior TBI research that also excluded this task (Dams-O’Connor et al., Reference Dams-O’Connor, Sy, Landau, Bodien, Dikmen, Felix, Giacino, Gibbons, Hammond, Hart, Johnson-Greene, Lengenfelder, Lequerica, Newman, Novack, O’Neil-Pirozzi and Whiteneck2018; Hicks et al., Reference Hicks, Sander, McKenzie, Carrier, Fraser, Hall, Pappadis, Ponsford and Fleming2024; Nelson et al., Reference Nelson, Barber, Temkin, Dams-O’Connor, Dikmen, Giacino, Kramer, Levin, McCrea, Whyte, Bodien, Yue and Manley2021). We analyzed performance on each of the six subtests, as well as previously factor-analytically derived composite scores of Episodic Memory (average of Word List Immediate Recall and Delayed Recall), Executive Function (average of Digits Backward, Category Fluency, Number Series, Backward Counting), and Overall Cognition (average of all six subtests; Nelson et al., Reference Nelson, Barber, Temkin, Dams-O’Connor, Dikmen, Giacino, Kramer, Levin, McCrea, Whyte, Bodien, Yue and Manley2021).
Data analysis
Data were analyzed using “R,” version 4.3.2 (R Core Team, 2023), using the packages psych (Revelle, Reference Revelle2025), PASWR2 (Arnholt, Reference Arnholt2021), stats (R Core Team, 2023), Hmisc (Harrell & Dupont, Reference Harrell and Dupont2025), lavaan (Rosseel, Reference Rosseel2012), semhelpinghands (Cheung, Reference Cheung2024), and semTools (Jorgensen et al., Reference Jorgensen, Pornprasertmanit, Schoemann and Rosseel2025). All statistical tests were two-sided, with alpha set at .05.
Responses on the HADS and CD-RISC 10 were described in relation to general community normative data from Crawford et al. (Reference Crawford, Garthwaite, Lawrie, Henry, MacDonald, Sutherland and Sinha2009) and Campbell-Sills et al. (Reference Campbell-Sills, Forde and Stein2009), respectively. Normative data for the CAT-PD-SF were obtained from the authors of the “HiTOP Digital Assessment Tracker” (Jonas et al., Reference Jonas, Stanton, Simms, Mullins-Sweatt, Gillett, Dainer, Nelson, Cohn, Guillot, Kotov, Cicero and Ruggero2021). Age-corrected T-scores for the BRIEF-A indices were calculated using the professional manual (Roth et al., Reference Roth, Isquith and Gioia2005) and then converted to Z-scores. Age-, sex-, and education-adjusted Z-scores for the BTACT were derived from the Midlife in the United States epidemiological (MIDUS 2) study normative data (DiBlasio et al., Reference DiBlasio, Sima, Kumar, Kennedy, Retnam, Lachman, Novack and Dams-O’Connor2021), as no Australian normative data were available. We conducted t-tests to compare scores in our TBI sample with the available normative samples.
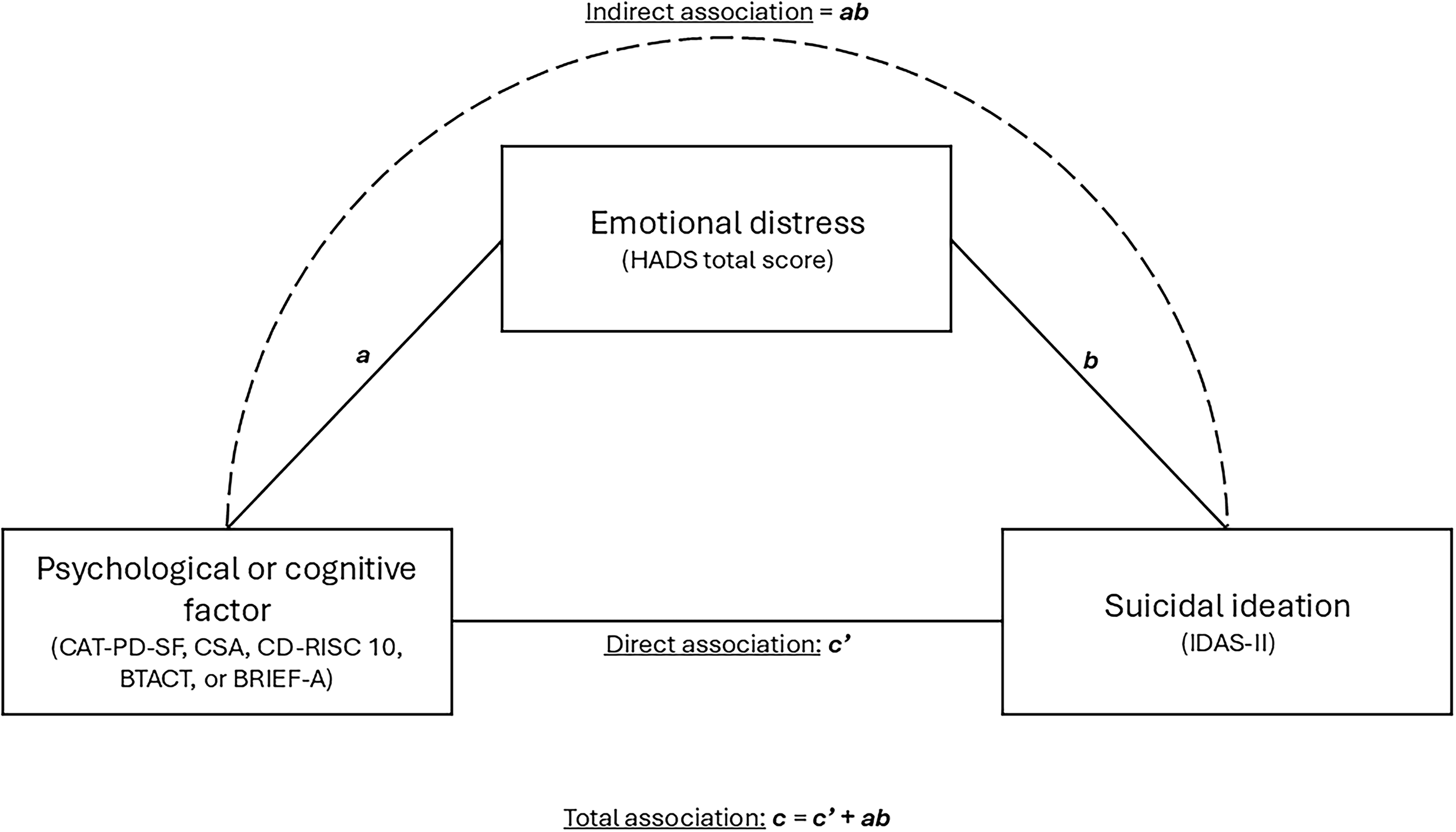
To address the study aims, zero-order, pairwise correlations among all variables were calculated. Spearman’s coefficients were used for correlations involving SI, given its positive skew (Z skew = +2.32), while Pearson’s correlations were applied for all other pairwise associations (Z skew for other variables between + 1 and –1). For each psychological or cognitive factor significantly associated with SI, we next conducted exploratory analyses considering the extent to which these associations occurred independently versus indirectly through emotional distress (measured by the HADS total score). To do this, we conducted path analyses, represented by the conceptual model shown in Figure 2. These analyses estimated the total association between each psychological or cognitive factor and SI, the indirect association (i.e., occurring indirectly through emotional distress), and the direct association (i.e., independent of emotional distress). Although such analyses are sometimes referred to as “cross-sectional mediation,” we avoid this terminology, as it implies a causal framework that cannot be determined with cross-sectional data. Instead, we use more neutral language, referring to direct and indirect associations.

Figure 2. Conceptual model for estimated path models. Note: The direct association (c’) reflects the relationship between a psychological or cognitive factor and suicidal ideation that is independent of emotional distress. The indirect association (ab) – representing the relationship between the psychological or cognitive factor and suicidal ideation occurring indirectly through emotional distress – was calculated by multiplying the estimates for the association between the psychological/cognitive factor and emotional distress (a) and the association between emotional distress and suicidal ideation (b). The total association (c) between the psychological or cognitive factor and suicidal ideation is equal to the sum of the estimates for the direct (c’) and indirect associations (ab). The percentage of the total association explained by emotional distress can therefore be calculated using the following formula: (ab / c’ + ab) × 100. CAT-PD-SF = Comprehensive Assessment of Traits Relevant to Personality Disorders – Static Form; CSA = Coping Scale for Adults; CD-RISC 10 = 10-item Connor–Davidson Resilience Scale, BTACT = Brief Test of Adult Cognition by Telephone; BRIEF-A = self-report Behavior Rating Inventory of Executive Function – Adult; HADS = Hospital Anxiety and Depression Scale; IDAS-II = Inventory of Depression and Anxiety Symptoms – Expanded Version.
In these path analyses, SI was treated as a continuous variable; due to its positive skew, models were estimated using maximum likelihood estimation with 10,000 bootstraps, providing a robust, nonparametric approach for non-normally distributed data. Before estimating each path model, we also first ensured that emotional distress and the other psychological or cognitive variables were not significantly multicollinear in their prediction of SI (all variance inflation factors were ≤ 2.24).
Addressing Type I and Type II errors
Supplementary Appendix S2 provides a detailed account of efforts to address Type I and Type II errors. In brief, to address the potential for Type I errors (i.e., false positives), we applied false discovery rate (FDR) correction to several families of p-values using the Benjamini–Hochberg procedure (Benjamini & Hochberg, Reference Benjamini and Hochberg1995). Where FDR correction was applied, all associations that were statistically significant prior to correction remained significant after correction, suggesting that our findings demonstrated robustness to Type I errors.
Regarding Type II errors (i.e., false negatives), an a priori power analysis was not conducted as this was a secondary analysis of existing data. Instead, we conducted sensitivity and simulation-based power analyses (Lakens, Reference Lakens2022). These analyses indicated that the current study had sufficient power (80%) to detect pairwise correlations in the small-to-medium range (r = .27–.32) and sufficient power (80%) to detect direct associations of medium size in the path analyses (β = .29–.31). The study also had fair power (68–73%) to detect medium-sized indirect associations of approximately β = .13, reflecting the product of a small-to-moderate association and a strong association, based on theoretically and empirically plausible input values (see Supplementary Appendix S2).
Results
Sample characteristics
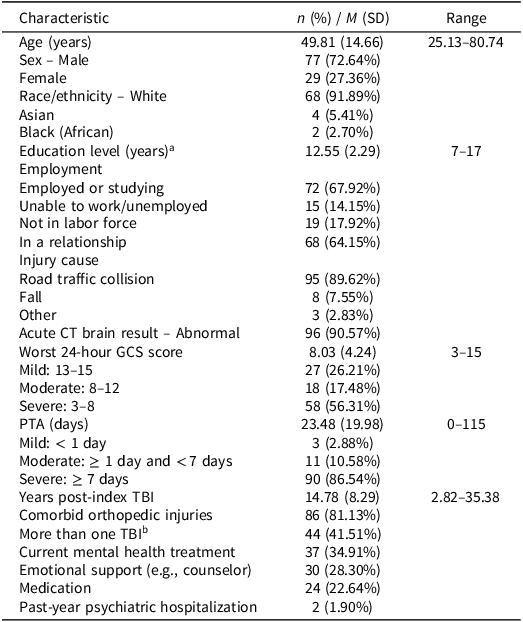
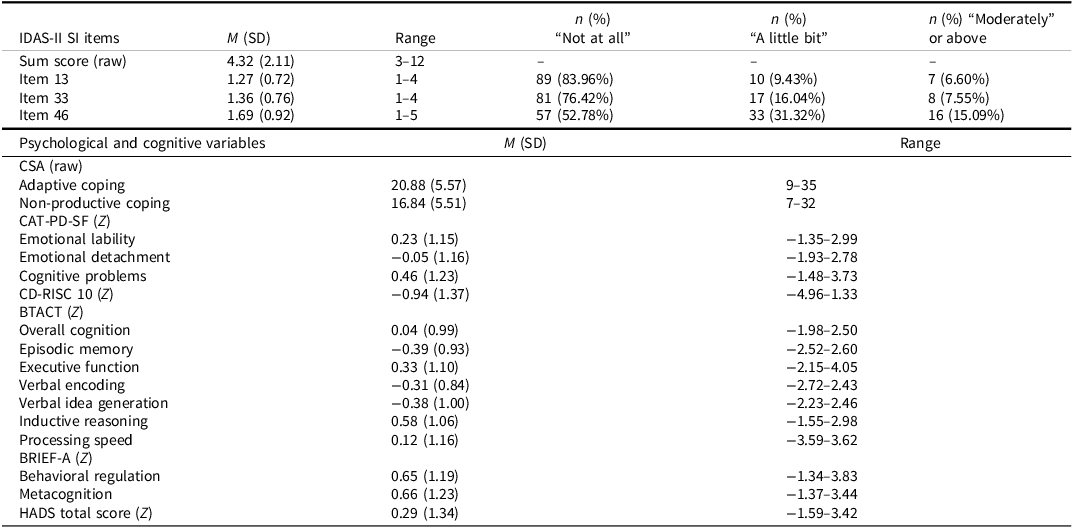
Table 1 details the sociodemographic and injury characteristics of the sample, while Table 2 provides descriptive and frequency statistics for the psychological and cognitive factors. Regarding SI on the IDAS-II, half of the sample did not endorse experiencing any SI-related items in the previous two weeks. In contrast, over the same timeframe, approximately 16, 25, and 46% reported thoughts of suicide, feeling the world would be better off without them, and thoughts about their death, respectively, at least “a little bit” (see Table 2).
Table 1. Sample characteristics (n = 106)

Note: CT = computed tomography; GCS = Glasgow Coma Scale; PTA = post-traumatic amnesia; TBI = traumatic brain injury.
Complete data were available for the following variables: age, sex, employment, in a relationship, injury cause, acute CT brain result, years post-index TBI, comorbid orthopedic injuries, more than one TBI, emotional support, and medication. Data were available for 74/106 (race/ethnicity), 101/106 (education level), 103/106 (GCS), 104/106 (PTA), and 105/106 (past-year psychiatric hospitalization). Unfortunately, race/ethnicity was not routinely recorded in the medical record, resulting in missing data for n = 38. However, for approximately 70% of participants, this information was obtained from other studies.
a Recorded at the time of injury.
b Participants were asked if they had experienced additional head injuries, including concussions, besides their index TBI. However, these additional head injuries were neither medically confirmed nor characterized in terms of severity.
Table 2. Descriptive and frequency statistics for psychological variables (n = 86–106)
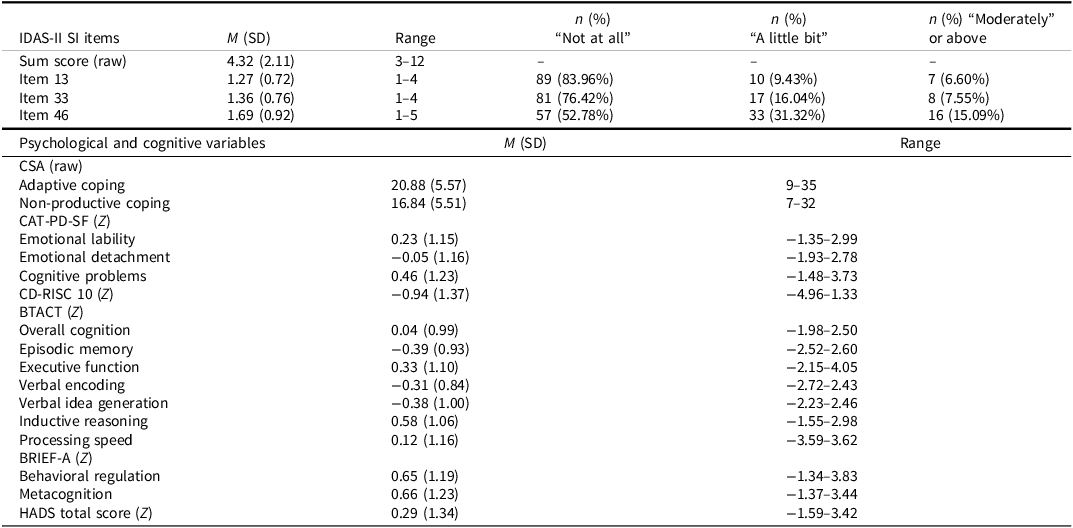
Note: IDAS-II = Inventory of Depression and Anxiety Symptoms – Expanded Version; SI = suicidal ideation; CSA = Coping Scale for Adults; CAT-PD-SF = Comprehensive Assessment of Traits Relevant to Personality Disorders – Static Form; CD-RISC 10 = 10-item Connor–Davidson Resilience Scale, BTACT = Brief Test of Adult Cognition by Telephone; BRIEF-A = self-report Behavior Rating Inventory of Executive Function – Adult; HADS = Hospital Anxiety and Depression Scale.
Data were available for 106/106 (SI), 100/106 (adaptive coping), 99/106 (non-productive coping), 103/106 (emotional lability), 104/106 (emotional detachment), 102/106 (cognitive problems), 96/106 (resilience), 86/106 (BTACT), 93/106 (behavioral regulation), 92/106 (metacognition), and 106/106 (HADS). The IDAS-II SI sum score was formed from three items: Item 13 (“I had thoughts of suicide”), Item 33 (“I thought that the world better off without me”), and Item 46 (“I thought about my own death”). While 92 individuals in the follow-up study completed the BTACT, we only used data from 86 participants who also had complete data for SI, the HADS, and education (required to norm the BTACT). Descriptive statistics were standardized against normative data using Z-transformation (Mnormative = 1, SDnormative = 0), except for the IDAS-II and CSA. The possible raw score range for the IDAS-II SI sum score is 3–15, with individual item responses being able to range between 1 and 5. For the CSA subscales, raw scores can range from 7 to 35.
Compared to normative data, participants with TBI reported significantly higher anxiety and depression symptoms over the previous week (HADS total score: p = .029, d = 0.29), lower psychological resilience (CD-RISC 10: p < .001, d = 0.90), more self-reported executive functioning and self-regulation difficulties over the previous month (BRIEF-A BRI: p < .001, d = 0.65; BRIEF-A MI: p < .001, d = 0.66), and more perceived cognitive problems in general (CAT-PD-SF Cognitive Problems: p = .001, d = 0.44). However, they did not differ significantly on measures of emotional lability (CAT-PD-SF Affective Lability: p = .068, d = 0.22) or detachment (CAT-PD-SF Emotional Detachment: p = .691, d = 0.05).
On the BTACT, the TBI sample performed significantly worse based on normative data from MIDUS 2 on the Episodic Memory composite (Episodic Memory composite: p < .001, d = 0.39; Word List Immediate Recall: p < .001, d = 0.31; Word List Delayed Recall: p < .001, d = 0.38), showed no difference in verbal working memory (Digits Backward: p = .595, d = 0.06), verbal idea generation (Category Fluency: p = .058, d = 0.17), or processing speed (Backward Counting: p = .345, d = 0.12), but performed significantly better on inductive reasoning (Number Series: p < .001, d = 0.58) and the Executive Function composite (p = .006, d = 0.33) after adjusting for age, sex, and education level. There was no significant difference between the TBI and normative samples on the Overall Cognition composite (p = .734, d = 0.04).
Psychological and cognitive correlates of SI in individuals with TBI
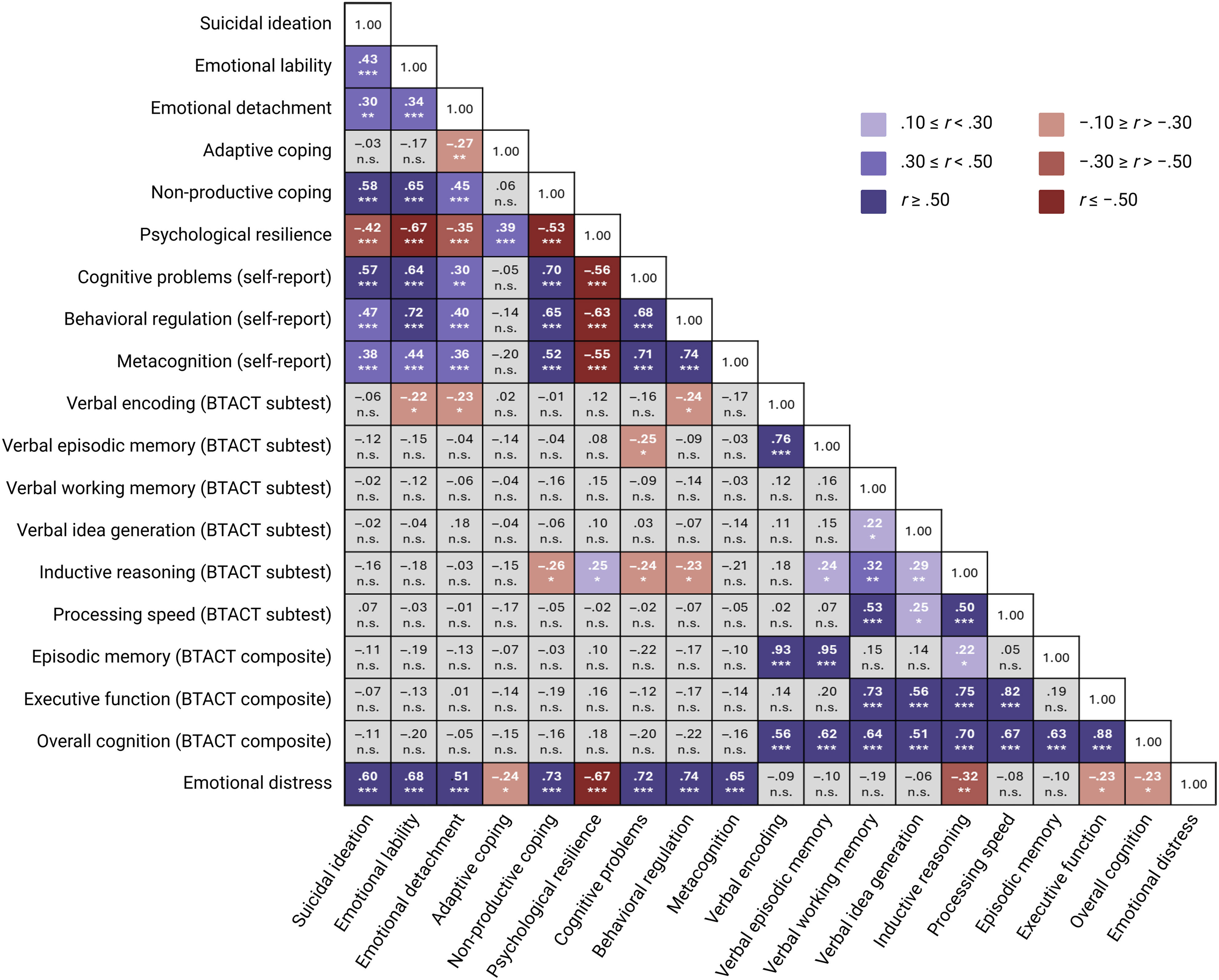
Figure 3 illustrates the pairwise associations between the psychological and cognitive factors, with detailed statistics provided in Supplemental Appendix S3. SI was significantly positively associated with emotional lability (ρ = .43, corrected p < .001), emotional detachment (ρ = .30, corrected p = .004), non-productive coping (ρ = .58, corrected p < .001), perceived cognitive and executive functioning problems (CAT-PD-SF Cognitive Problems: ρ = .57, corrected p < .001; BRIEF-A BRI: ρ = .47, corrected p < .001; BRIEF-A MI: ρ = .38, corrected p < .001), and emotional distress symptoms (HADS total score: ρ = .60, corrected p < .001). SI was also negatively associated with psychological resilience (ρ = –.42, corrected p < .001) but showed no significant associations with adaptive coping (ρ = –.03, corrected p = .840) or objective cognitive performance across the BTACT (see Figure 3; ρ values between –.16 and .07, corrected p = .291–.840).

Figure 3. Pairwise associations between variables of interest (n = 73–106). Note: The numbers presented are correlation coefficients, either Spearman’s (for pairwise associations involving suicidal ideation, due to its positive skew) or Pearson’s (for all other associations). Correlations were calculated using pairwise complete data, ranging from 73 (between self-reported executive functioning difficulties and objective cognitive performance) to 106 participants (between suicidal ideation and emotional distress). ***p < .001, **p < .010, *p < .050, n.s. = non-significant (i.e., p ≥ .050). BTACT = Brief Test of Adult Cognition by Telephone.
Direct and indirect associations between SI and psychological and cognitive factors
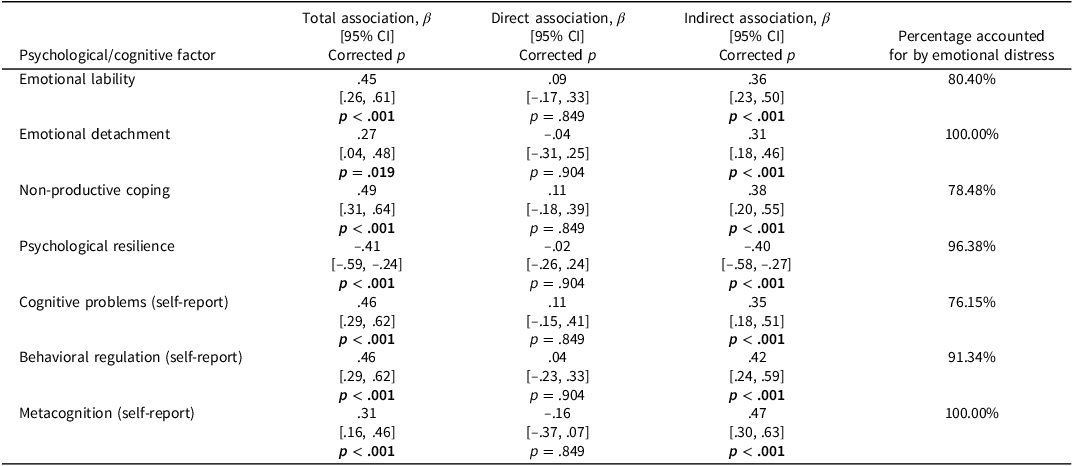
In summary of the above, pairwise correlational analyses showed that SI was positively associated with emotional lability, detachment, self-reported cognitive and executive functioning problems, and non-productive coping, and negatively associated with resilience. To examine the extent to which these associations occurred independently versus indirectly through emotional distress (measured with the HADS), we conducted exploratory path analyses. Table 3 presents the path analysis results, indicating that none of the psychological and cognitive factors were significantly associated with SI independently of emotional distress, either before or after FDR correction. Instead, approximately 76% of the association between SI and self-reported cognitive problems, up to 100% for emotional detachment and self-reported metacognition, were estimated to occur indirectly through emotional distress – associations that remained significant following correction. Put differently, the pairwise correlations reported in the previous section did not account for indirect associations occurring through emotional distress. When emotional distress was included as a third variable in path analysis, the relatively small proportion of variance in SI (i.e., 0–24%) uniquely attributable to the other psychological and cognitive variables was no longer significant, before or after correction.
Table 3. Results of path models (n = 92–104)

Note: The models were estimated using pairwise complete data from 103 (emotional lability), 104 (emotional detachment), 99 (non-productive coping), 96 (psychological resilience), 102 (cognitive problems), 93 (behavioral regulation), and 92 participants (metacognition). 95% confidence intervals were derived from 10,000 bootstraps. Estimates (β) and their bootstrapped confidence intervals are fully standardized. The direct association reflects the relationship between a psychological or cognitive factor and suicidal ideation that is independent of emotional distress. The indirect association represents the relationship between the psychological/cognitive factor and suicidal ideation occurring indirectly through emotional distress. The total association equals the sum of the estimates for the direct and indirect associations – but may differ slightly in the table due to rounding. The percentages were calculated using unrounded estimates. In the case of emotional detachment and metacognition, where the direct associations had an opposite sign (negative) to the total associations (positive), we indicated that the percentage of the total associations accounted for by emotional distress was 100%. The p-values have been corrected for false discovery rate using the Benjamini–Hochberg procedure.
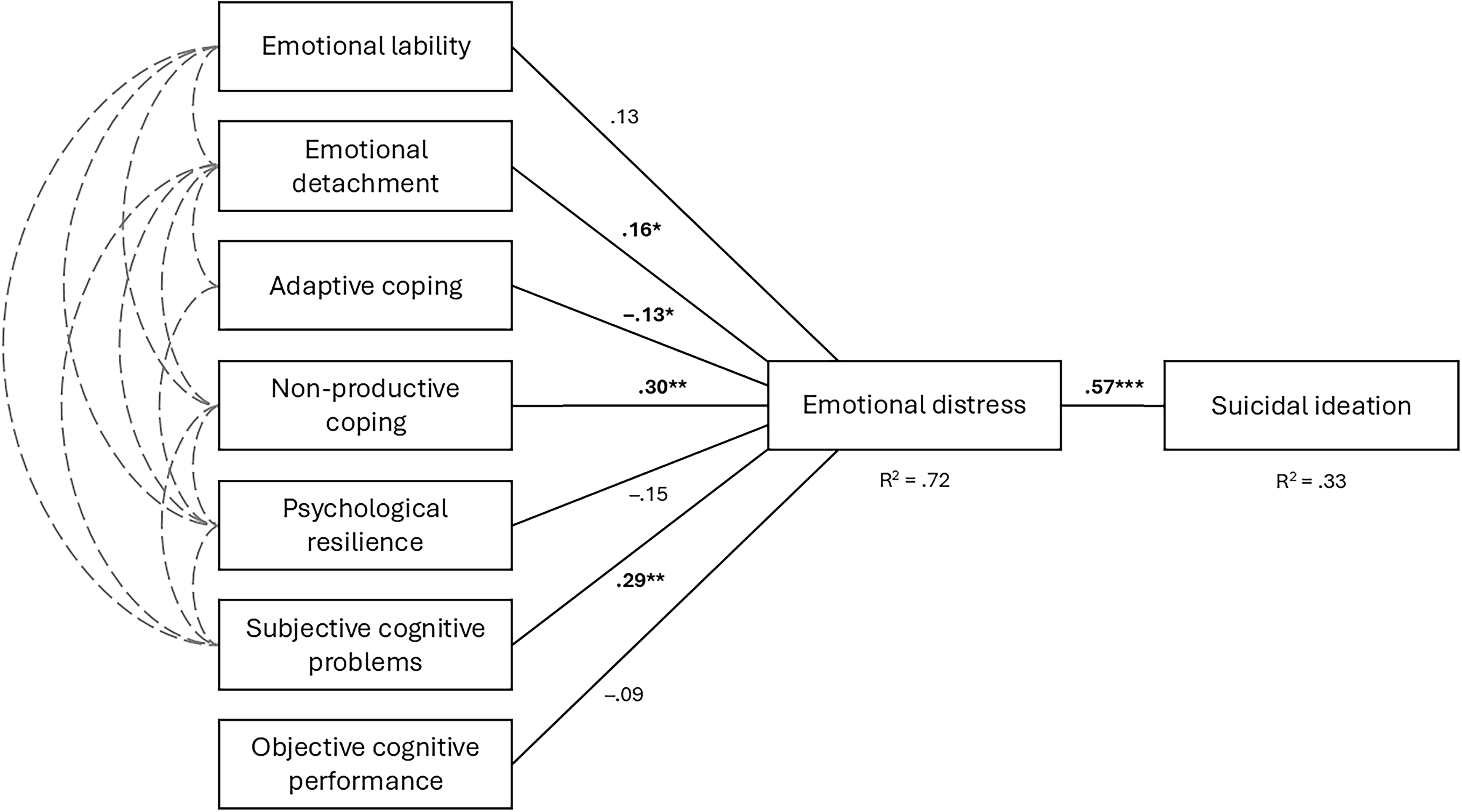
As an additional exploratory analysis informed by the preceding results, we constructed a final path model, presented in Figure 4. This model simultaneously estimated the indirect associations between seven psychological or cognitive variables and SI occurring through emotional distress. The model demonstrated a good fit (root mean square error of approximation = .06, comparative fix index = .99, Tucker–Lewis index = .97, standardized root mean squared residual = .07), with the included psychological and cognitive factors collectively accounting for 72% of the variance in emotional distress. Emotional detachment, adaptive coping, non-productive coping, and self-reported cognitive problems each accounted for unique portions of this variance. Emotional distress, in turn, accounted for 33% of the variance in SI. Further details on the model are provided in the figure note, and the full statistical output is available in Supplemental Table S2.

Figure 4. Final path model (n = 106). Note: This path model was estimated using data from all 106 participants with 10,000 bootstraps, utilizing full information maximum likelihood estimation to model relationships based on pairwise complete data. The model fit the data well, including a non-significant chi-square test (desirable): χ 2(36) = 20.96, p = .180, robust root mean square error of approximation = .06, robust comparative fix index = .99, robust Tucker–Lewis index = .97, standardized root mean squared residual = .07. To reduce model complexity, we used only the CAT-PD-SF Cognitive Problems scale as a measure of subjective cognitive problems and the BTACT Overall Cognition composite as a measure of objective cognitive performance, both of which were significantly associated with emotional distress in the pairwise correlational analyses (Figure 3). Based on the results of the initial path models (Table 3), the seven psychological or cognitive factors, shown on the left side of the figure, were specified as having no direct relationship with suicidal ideation, only indirect relationships through emotional distress. The path coefficients in the figure are fully standardized, with significant relationships highlighted in bold. Those coefficients representing the direct relationships between the psychological and cognitive factors and emotional distress are partial regression coefficients: emotional detachment, adaptive coping, non-productive coping, and self-reported cognitive problems showed unique associations with emotional distress, while emotional lability, psychological resilience, and objective cognitive performance accounted for variance in emotional distress shared with other factors. Covariances/correlations between psychological and cognitive factors are depicted as dashed gray lines and were specified based on the previously identified pairwise correlations (Figure 3). All covariances were statistically significant (see Supplemental Table S2 for full statistical output). ***p < .001, **p < .010, *p < .050.
Discussion
This study examined psychological and cognitive correlates of SI in 106 individuals with moderate–severe TBI. As hypothesized, SI was positively associated with emotion-processing difficulties (emotional lability and detachment), non-productive coping strategies, and self-reported cognitive and executive functioning problems, while being negatively associated with psychological resilience. However, contrary to expectations, pairwise correlations showed no significant association between SI and either adaptive coping or objective cognitive performance. Both these variables, however, were inversely associated with emotional distress, which itself was strongly correlated with SI. Further exploratory analyses indicated that emotional distress, encompassing symptoms of depression and anxiety, accounted for 76–100% of the associations between the other psychological and cognitive factors and SI, rather than these factors being independent correlates. A final path model demonstrated that a set of seven psychological and cognitive factors collectively accounted for 72% of the variance in emotional distress, which, in turn, accounted for 33% of the variance in SI.
Our study examined associations between coping strategies and suicidality after TBI. Pairwise correlations revealed that non-productive coping, but not adaptive coping, was associated with SI. Consistent with previous research (Bombardier et al., Reference Bombardier, D’Amico and Jordan1990; Curran et al., Reference Curran, Ponsford and Crowe2000; Gould et al., Reference Gould, Ponsford, Johnston and Schönberger2011a; Spitz et al., Reference Spitz, Schönberger and Ponsford2013), non-productive coping also showed a stronger correlation with emotional distress than adaptive coping, and the two coping styles were not significantly associated with one another (see Figure 3). These findings align with the Health Theory of Coping (Stallman, Reference Stallman2020), which conceptualizes suicidality itself as an unhealthy coping strategy used when healthy coping strategies fail to sufficiently alleviate distress. Supporting this theory, research indicates that unhealthy coping strategies, including suicidality, are often used during periods of high distress, even when healthy strategies are also being utilized (Stallman et al., Reference Stallman, Beaudequin, Hermens and Eisenberg2021). Alternatively, non-productive coping strategies may simply be more frequently used or dominant in response to distress among individuals with TBI, outweighing healthier, problem-focused approaches (Spitz et al., Reference Spitz, Schönberger and Ponsford2013).
The observed discrepancy between subjective and objective cognitive measures also warrants discussion, as only subjective cognitive problems were significantly associated with SI in pairwise correlations. Subjective cognitive concerns also showed a stronger correlation with emotional distress than objective cognitive performance (see Figure 3), underscoring the role of self-perceived impairments in psychological well-being after TBI. These findings replicate previous research in TBI and other neuropsychological populations, suggesting that subjective and objective cognitive measures may reflect distinct constructs (Byrne et al., Reference Byrne, Coetzer and Addy2017; Finley et al., Reference Finley, Cladek, Gonzalez and Brook2024; Draper & Ponsford, Reference Draper and Ponsford2009; Fann et al., Reference Fann, Katon, Uomoto and Esselman1995; Grauwmeijer et al., Reference Grauwmeijer, Heijenbrok-Kal, Peppel, Hartjes, Haitsma, De Koning and Ribbers2018; Løvstad et al., Reference Løvstad, Sigurdardottir, Andersson, Grane, Moberget, Stubberud and Solbakk2016; Satz et al., Reference Satz, Forney, Zaucha, Asarnow, Light, McCleary, Levin, Kelly, Bergsneider, Hovda, Martin, Namerow and Becker1998; Vos et al., Reference Vos, Williams, Poritz, Ngan, Leon-Novelo and Sherer2020).
Several mechanisms may explain this discrepancy. First, the subjective measures of cognitive functioning used in this study assess lapses in everyday cognition (e.g., “I easily lose my train of thought”), which are not necessarily captured by performance measures administered in controlled testing environments. Furthermore, emotional distress may contribute to more negative self-evaluations, leading individuals to perceive relatively minor cognitive lapses as more severe or pathological (Finley et al., Reference Finley, Cladek, Gonzalez and Brook2024; Vos et al., Reference Vos, Williams, Poritz, Ngan, Leon-Novelo and Sherer2020). Conversely, anosognosia or reduced insight may lead individuals with TBI to overestimate their cognitive abilities and thereby buffer against emotional distress. Additionally, recall bias – particularly “good old days” bias – may cause individuals to overestimate their pre-injury cognitive functioning, creating further misalignment between subjective and objective assessments of cognition (Schlehofer & Suhr, Reference Schlehofer and Suhr2024).
Nevertheless, although subjective cognitive measures showed stronger associations with SI, several measures of objective cognitive functioning were inversely associated with emotional distress (see Figure 3). Given that emotional distress itself was strongly associated with SI, these findings suggest that objective cognitive impairment may still play at least an indirect role in suicide risk after TBI. Previous studies have also reported inverse associations between objective cognitive functioning and emotional distress after TBI (Keatley et al., Reference Keatley, Bombardier, Watson, Kumar, Novack, Monden and Dams-O’Connor2023; Uiterwijk et al., Reference Uiterwijk, Stargatt, Humphrey and Crowe2022), as well as SI (Brenner et al., Reference Brenner, Bahraini, Homaifar, Monteith, Nagamoto, Dorsey-Holliman and Forster2015; Homaifar et al., Reference Homaifar, Brenner, Forster and Nagamoto2012). Furthermore, we know that cognitive impairment is a major cause of disability after TBI, such as inability to return to work and social challenges, which can drive emotional distress (Carmichael et al., Reference Carmichael, Hicks, Gould, Spitz and Ponsford2023b; Gould et al., Reference Gould, Ponsford, Johnston and Schönberger2011b; Schönberger et al., Reference Schönberger, Ponsford, Gould and Johnston2011) and, in turn, suicidality (Awan et al., Reference Awan, DiSanto, Juengst, Kumar, Bertisch, Niemeier, Fann, Kesinger, Sperry and Wagner2021; Perrin et al., Reference Perrin, Klyce, Fisher, Juengst, Hammond, Gary, Niemeier, Bergquist, Bombardier, Rabinowitz, Zafonte and Wagner2022). Thus, it would be premature to dismiss the potential relevance of cognitive impairment in future research.
Importantly, the absence of evidence for a relationship does not equate to evidence of absence (Feres & Feres, Reference Feres and Feres2023), especially given certain methodological limitations. The small sample size and the high-functioning nature of our TBI sample – who were, on average, long post-injury and highly educated – may have reduced the likelihood of detecting significant correlations between objective cognition and SI. Cognitive impairments are typically more pronounced during the earlier stages of recovery and may partially resolve over time (Ponsford, Reference Ponsford, Ponsford, Sloan and Snow2012); thus, associations between cognitive impairment and SI may be more detectable earlier post-injury, when cognitive difficulties are more prevalent at the group level. While our participants with TBI performed worse on memory testing, they scored similarly to, or in the case of the Number Series subtest, significantly better than the MIDUS 2 normative sample on the rest of the BTACT. The BTACT, as a telephone cognitive screening measure, may lack the sensitivity and ecological validity needed to detect cognitive impairment, particularly executive dysfunction, as it manifests in more complex, real-world situations. Additionally, the use of US norms may have further limited the BTACT’s ability to detect meaningful differences in our Australian sample (Kamieniecki & Lynd-Stevenson, Reference Kamieniecki and Lynd-Stevenson2002; Ryan et al., Reference Ryan, Woods, Britt, Murray, Shah, Reid, Wolfe, Nelson, Orchard, Lockery, Trevaks and Storey2020).
Implications
These findings increase our understanding of psychological and cognitive factors associated with SI after moderate–severe TBI, while underscoring the central role of depression and anxiety symptoms. Importantly, the absence of independent associations between these broader factors and SI does not mean they are irrelevant for clinical risk assessment, formulation, or treatment. Some factors may not have shown unique associations because they overlap conceptually with emotional distress (e.g., perceived cognitive difficulties may index distress rather than being a distinct risk factor). Others, however, may function as distinct constructs that contribute to SI indirectly by increasing emotional distress, suggesting a mediating relationship. For example, emotion-processing difficulties, poor coping, and low resilience may contribute to the development, maintenance, or exacerbation of emotional distress, which in turn serves as a more immediate risk factor for suicidality. Addressing these contributory factors in treatment may therefore help alleviate emotional distress and reduce SI, but longitudinal research is needed to confirm these potential mediation effects.
Clinicians assessing suicide risk in individuals with TBI should consider not only the level of depression and anxiety, but also difficulties in emotion regulation, which may manifest as emotional lability, emotional detachment/avoidance, poor emotional awareness, difficulty accepting emotions, and impaired impulse control when experiencing distress (Gratz & Roemer, Reference Gratz and Roemer2004) – issues which are common after brain injury (Salas et al., Reference Salas, Gross and Turnbull2019). Given emerging evidence linking emotional dysregulation to SI, assessing these difficulties may refine risk stratification and inform targeted interventions. The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, Reference Gratz and Roemer2004), though originally developed for neurotypical populations, has been used in studies on emotional problems after brain injury (Cooper et al., Reference Cooper, Phillips, Johnston, Whyte and MacLeod2015; Neumann et al., Reference Neumann, Malec and Hammond2017; Shields et al., Reference Shields, Ownsworth, O’Donovan and Fleming2016). The DERS is a broad measure that captures elements overlapping in content with the measures used in our study, such as poor impulse control when distressed (emotional lability) and poor emotional awareness (emotional detachment), along with other emotion regulation difficulties. However, further work validating measures targeting specific emotion-processing constructs in individuals with moderate–severe TBI could also be beneficial.
The findings suggest that reducing maladaptive coping strategies, such as self-blame, wishful thinking, social withdrawal, and substance use, may be an important clinical consideration in addressing suicidality following TBI. It is also important to recognize that individuals with TBI who report having adaptive coping strategies may still be at risk for suicidality. Intervention may consequently need to focus on not only strengthening coping strategies but also ensuring their effective application during times of high distress, building distress tolerance skills, and developing personalized, “in-the-moment” psychological tools such as coping and safety plans (Stallman, Reference Stallman2018; Rainbow et al., Reference Rainbow, Tatnell, Blashki and Melvin2024). Our findings also replicate the association between resilience and SI after TBI (Paasila et al., Reference Paasila, Smith, Daher and Simpson2022), highlighting the value of a strengths-based approach rather than a solely risk-focused framework. Finally, on the basis of the available evidence, we recommend that clinicians consider their clients’ injury-related cognitive impairments and supplement self-report of cognitive functioning with performance-based measures or informant reports, using their skills in clinical formulation to develop hypotheses about the functional interplay between cognitive difficulties, emotional distress, and suicidality on a case-by-case basis.
Regarding specific intervention programs, research on suicide prevention for individuals with TBI remains limited, with only small-scale pilot trials targeting hopelessness (Brenner et al., Reference Brenner, Forster, Hoffberg, Matarazzo, Hostetter, Signoracci and Simpson2018; Simpson et al., Reference Simpson, Tate, Whiting and Cotter2011) and problem-solving (Barnes et al., Reference Barnes, Monteith, Gerard, Hoffberg, Homaifar and Brenner2017). More broadly, however, evidence supports the use of adapted cognitive behavioral therapy for treating depression and anxiety in individuals with TBI (Barua et al., Reference Barua, Ahrens, Shao, MacKenzie, Wolfe, Sequeira, Teasell, Loh and Mehta2024; Ponsford et al., Reference Ponsford, Lee, Wong, McKay, Haines, Alway, Downing, Furtado and O’Donnell2016), while other psychological interventions incorporating psychoeducation, emotional support, and skill-building have also demonstrated promise in improving emotional regulation, coping, and resilience (Anson & Ponsford, Reference Anson and Ponsford2006b; Kreutzer et al., Reference Kreutzer, Marwitz, Sima, Mills, Hsu and Lukow2018; Kuppelin et al., Reference Kuppelin, Goetsch, Choisel, Isner-Horobeti, Goetsch and Krasny-Pacini2024; Mueller et al., Reference Mueller, Wesenberg, Nestmann, Stubbs, Bebbington and Raymont2018; Neumann et al., Reference Neumann, Parrott and Hammond2024b; Tsaousides et al., Reference Tsaousides, Spielman, Kajankova, Guetta, Gordon and Dams-O’Connor2017). Pharmacological interventions may help manage emotional dysregulation (e.g., lability) among individuals with TBI, but evidence remains mixed and limited (Arciniegas & Wortzel, Reference Arciniegas and Wortzel2014; Hicks et al., Reference Hicks, Clay, Hopwood, James, Jayaram, Perry and Ponsford2019, Reference Hicks, Clay, Ponsford, Perry, Jayaram, Batty and Hopwood2020; Wortzel et al., Reference Wortzel, Brenner, Silver, Arciniegas, Yudofsky and Hales2018). Notably, despite their potential utility, none of these broader interventions have been directly assessed for their impact on suicidality after TBI. Future research evaluating these interventions needs to incorporate measures of suicidality to establish their utility. Focusing on our specific findings, the results suggest that emotional lability, emotional detachment, coping style, and psychological resilience may be important not only for identifying suicide risk but also as potential targets for clinical intervention following moderate–severe TBI, potentially paving the way for new interventions. More work is needed to understand the role of cognitive profiles in relation to suicidality in this population.
Limitations
These findings should be interpreted in light of the study’s limitations. First, while general population rates of key factors were provided, the absence of a control group limits the ability to draw injury-specific conclusions regarding the mechanisms underlying SI in individuals with moderate–severe TBI. Potentially, similar patterns of SI may also be observed in non-TBI populations. Nevertheless, this study focused on studying correlates of SI in individuals with TBI, given the clinical significance of understanding typical profiles in this cohort. Second, while previous studies have examined alexithymia in relation to suicidality after TBI (Neumann et al., Reference Neumann, Hammond, Sander, Bogner, Bushnik, Finn, Chung, Klyce, Sevigny and Ketchum2024a, Reference Neumann, Hammond, Sander, Bogner, Bushnik, Finn, Chung, Klyce, Sevigny and Ketchum2025; Henry et al., Reference Henry, Phillips, Crawford, Theodorou and Summers2006; Wood & Williams, Reference Wood and Williams2007; Wood et al., Reference Wood, Williams and Lewis2010), our dataset included a measure of emotional detachment – a construct which we have argued conceptually overlaps with, but may differ from, alexithymia. This, however, raises the possibility of a jangle fallacy, where we may be inclined to believe two constructs differ because they are labeled differently. Given that emotional processing and regulation encompass multiple facets, a comprehensive and contemporaneous investigation of these dimensions in the context of TBI would be valuable for advancing both theoretical understanding and clinical application (Salas et al., Reference Salas, Gross and Turnbull2019).
Third, our objective assessment of cognitive functioning relied on the BTACT, a brief screening measure with limited coverage of executive functioning domains (e.g., inhibitory control, set-shifting), which may not have been sensitive enough to detect executive dysfunction or other cognitive impairments. A more comprehensive neuropsychological battery is needed to clarify the relationship between objective cognition and SI after TBI. All BTACT scores were adjusted for age, sex, and education, but scores on the self-report questionnaires (e.g., measuring SI, emotional lability) were not adjusted. Fourth, we did not establish the validity of the obtained self-report and cognitive test data (using symptom and performance validity tests), and a few participants completed the psychiatric questionnaires with a researcher, rather than independently online. It is possible that these participants may have responded in a more socially desirable manner.
Fifth, the sample was relatively small and skewed toward relatively high-functioning individuals who were many years post-injury, limiting generalizability. Here, it is important to reiterate that, compared to the broader MERRC cohort of adults recruited from inpatient rehabilitation following TBI, our sample was more educated, had higher rates of pre-injury employment, and had sustained less severe brain injuries based on PTA duration. Furthermore, at the time of survey completion, around 68% of our participants reported being engaged in work or study – higher than the 40–50% previously reported within the first decade following moderate–severe TBI (Corrigan et al., Reference Corrigan, Cuthbert, Harrison-Felix, Whiteneck, Bell, Miller, Coronado and Pretz2014; Cuthbert et al., Reference Cuthbert, Harrison-Felix, Corrigan, Bell, Haarbauer-Krupa and Miller2015; Jourdan et al., Reference Jourdan, Bayen, Pradat-Diehl, Ghout, Darnoux, Azerad, Vallat-Azouvi, Charanton, Aegerter, Ruet and Azouvi2016; Ponsford et al., Reference Ponsford, Downing, Olver, Ponsford, Acher, Carty and Spitz2014). This elevated participation rate may partly reflect our Australian cohort’s access to comprehensive, multidisciplinary rehabilitation through a no-fault accident compensation system (Ponsford et al., Reference Ponsford, Downing, Olver, Ponsford, Acher, Carty and Spitz2014). Indeed, the MERRC cohort has previously demonstrated fewer ongoing impairments than a comparably injured US cohort (Ponsford et al., Reference Ponsford, Harrison-Felix, Ketchum, Spitz, Miller and Corrigan2021). Therefore, the current sample may be biased both in comparison to the broader MERRC cohort and to individuals from other settings with more limited or less consistent access to TBI rehabilitation. Larger studies with a greater representation of individuals with more severe cognitive impairments and post-injury suicidality are needed. Sample size is a relevant limitation, as our sensitivity and simulation-based power analyses indicated the study was underpowered (<80% power) to detect small associations that may still be meaningful. The sample also demonstrated variability across injury-related variables (e.g., time post-injury, PTA). These factors were not included as covariates in the current analyses in order to minimize statistical complexity given the relatively small sample size. However, a separate publication investigating associations with injury-related factors in an overlapping sample has just been published (Carmichael et al., Reference Carmichael, Fernando, Ponsford, Spitz, Hicks, Johnston and Gould2025b).
Sixth, longitudinal research is needed to more clearly identify factors driving post-TBI suicidality over different timescales. While our cross-sectional analysis of direct and indirect associations is hypothesis-generating and highlights the relevance of emotional distress to the observed relationships between broader psychological and cognitive factors and SI, it cannot explain the underlying mechanisms of these relationships (e.g., mediation). Seventh, the study focused only on SI, excluding other dimensions of suicidality. The self-report items used to assess SI are open to varied interpretations, such as the IDAS-II item on thoughts of death being related to the injury itself rather than SI. Future research should examine psychological and cognitive factors in relation to suicidal behaviors after TBI, which were not assessed here. Non-suicidal self-injury also warrants dedicated investigation in this population (Carmichael et al., Reference Carmichael, Fernando, Ponsford, Spitz, Hicks, Johnston and Gould2025b). Additionally, we acknowledge that the IDAS is not a widely used measure of SI in the TBI population, limiting comparability with other studies. Finally, by focusing on individual characteristics, this study does not address broader contextual, social, and systemic factors that likely also contribute to suicide risk in the TBI population.
Conclusions
Limitations notwithstanding, our study suggests that SI in individuals with moderate–severe TBI is positively associated with emotion-processing difficulties, non-productive coping, and perceived cognitive and executive functioning problems, and negatively associated with psychological resilience – primarily through shared associations with emotional distress. In contrast, SI was not significantly associated with adaptive coping or objective cognitive performance, although both were inversely related to emotional distress. These findings offer insights into factors that may contribute to SI in the moderate–severe TBI population, highlighting important considerations for suicide risk assessment and potential intervention targets.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S1355617725101471.
Funding statement
This work was supported by a grant funded by the Transport Accident Commission, through the Institute for Safety, Compensation and Recovery Research (awarded to the MERRC), and by Australian Government Research Training Program Scholarships (A.S. and J.-Y.C.).
Competing interests
None.