Highlights
-
Approximately 6.5% of patients within the Maritime Research Network for Family Practice database were diagnosed with migraine.
-
Pharmacological management of migraine in Nova Scotia aligns with best practice guidelines.
-
Not every patient who may have benefited from medications for treating migraine were prescribed such medications.
Introduction
Migraine is a common and debilitating neurological disorder, which is estimated to affect approximately 12% of the global population. Reference Burch, Buse and Lipton1 In 2019, migraine was ranked as a leading cause of disability in both sexes, and the primary cause of disability in women between the ages of 15–49. Reference Diseases and Injuries2 In Canada, approximately 8.3% of the population report living with migraine; however, this is likely an underestimate of the true prevalence since migraine is known to be under-diagnosed. Reference Cooke and Becker3,Reference Ramage-Morin and Gilmour4 The management of migraine is most commonly carried out by primary care providers, Reference Gibbs, Fleischer, Feldman, Sam and ODonovan5 with a smaller subset of patients treated by neurologists or other pain specialists. Studies have established that under-treatment of migraine is common Reference Diamond, Bigal, Silberstein, Loder, Reed and Lipton6,Reference Lipton, Bigal and Diamond7 and poor control of migraine is known to contribute to the worsening of symptoms and quality of life. Reference Buse, Pozo-Rosich and Dupont-Benjamin8 Thus, every effort should be made to ensure expert-recommended treatment plans are offered to Canadians living with migraine.
National and international guidelines have been established to describe optimal pharmacologic acute and preventative management of migraine. Reference Loder, Burch and Rizzoli9–Reference Worthington, Pringsheim and Gawel11 The Canadian Headache Society (CHS) has developed guidelines for the pharmacologic management of migraine, which include a 2013 guideline for acute management as well as 2012 and 2024 guidelines for the prevention of migraine. Reference Pringsheim, Davenport and Mackie10–Reference Medrea, Cooper and Langman12 For acute management of migraine attacks, the CHS guideline indicates that acetaminophen, acetylsalicylic acid, diclofenac, ibuprofen, naproxen sodium and triptans have the highest level of evidence for treatment of migraine attacks. This guideline also recommends against the use of opioid analgesics for routine management of migraine due to lack of evidence for superiority compared to other medications and risks associated with use. For pharmacologic prevention of migraine, the 2012 CHS guidelines recommend certain antidepressants, beta-blockers, calcium channel blockers and anti-seizure medications that have evidence for efficacy in reducing the frequency, severity, duration and disability of patients’ migraine attacks. The updated 2024 CHS guideline for migraine prevention added onabotulinumtoxinA and CGRP-targeting medications, which were approved and used for migraine prophylaxis even before the 2024 guideline update. Risk factors for ineffective migraine management include underdiagnosis, underprescribing of acute and preventative medications and non-compliance or discontinuation because of poor efficacy or side effects. Reference Rattanawong, Rapoport and Srikiatkhachorn13
There is currently limited data describing prescribing patterns among clinicians caring for patients with migraine in Canada. Reference Graves, Gerber and Berrigan14 It is therefore unknown whether current prescribing patterns reflect the recommendations made in headache management guidelines. Our aim for this exploratory study was to characterize the current pharmacological treatments prescribed for patients with migraine in Nova Scotia, Canada, seeking care through their primary care providers.
Methods
All research protocols received prior ethics board approval from Nova Scotia Health Authority (REB-1030253).
Retrospective cross-sectional analysis of migraine prescribing patterns
To characterize primary care prescribing patterns for migraine in Nova Scotia, we carried out a retrospective cross-sectional analysis of electronic medical record (EMR) data collected from January 2019 to December 2023 through the Maritime Research Network for Family Practice (MaRNet-FP), which manages a database of de-identified primary care EMR data from approximately 85,000 patients cared for by 67 primary care providers. Reference Birtwhistle, Keshavjee and Lambert-Lanning15,Reference Birtwhistle16 MaRNet-FP is part of a larger collection of national networks called the Canadian Primary Care Sentinel Surveillance Network (CPCSSN), which is composed of 14 regional networks contributing data centrally on ∼2 million patients across 1500 primary care providers in eight provinces and one territory. CPCSSN extracts, de-identifies and standardizes raw EMR data into functional data utilized for quality improvement, chronic disease surveillance and research. These data are stored at the Centre for Advanced Computing at Queen’s University and adhere to Personal Health Information Protection Act and ISO27002 privacy standards.
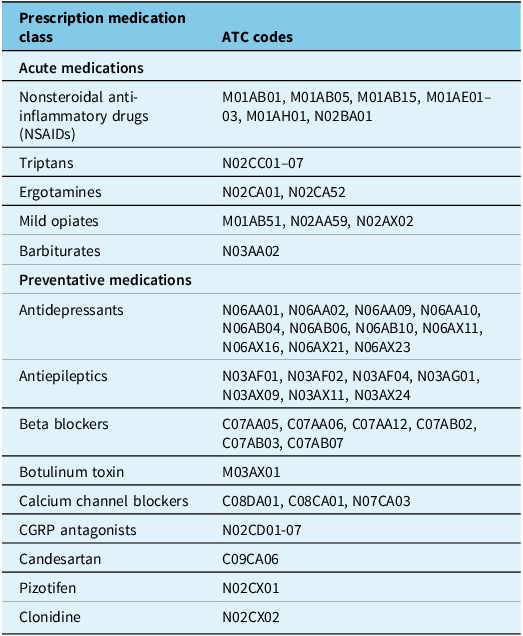
Study data were abstracted from all patients in the MaRNet-FP database who were 18 years or older at the index date and had ever been diagnosed with migraine as identified using ICD-9 codes (including all diagnoses with parent code 346). Patients under the age of 18 or patients who do not have a diagnosis of migraine were excluded from data abstraction. To better characterize the population of patients suffering from migraine in Nova Scotia, age, sex, geographical region and migraine diagnosis were collected. Medications which could be used for the acute and preventative management of migraine were abstracted for these patients using Anatomical Therapeutic Chemical codes (Table 1). These medications included those recommended by migraine prescribing guidelines as well as analgesic medications, which may be prescribed but have poor evidence for benefit in migraine. Using these data, the percentage of patients who were prescribed any type of acute or preventative migraine medications was calculated. The percentage of patients who were prescribed multiple medications that can be used in the acute or preventative treatment of migraine was also described. As this was an exploratory study, a priori hypotheses about prescribing patterns were not made and statistical analyses were not applied.
Table 1. Medications abstracted from MaRNet-FP EMR database

Note: Medications that could be used for the acute and preventive management of migraine were identified using their Anatomical Therapeutic Chemical (ATC) codes. Where possible, classes of medication were identified. Unique medications were also identified when a single medication is indicated for migraine rather than a class of drugs.
Results
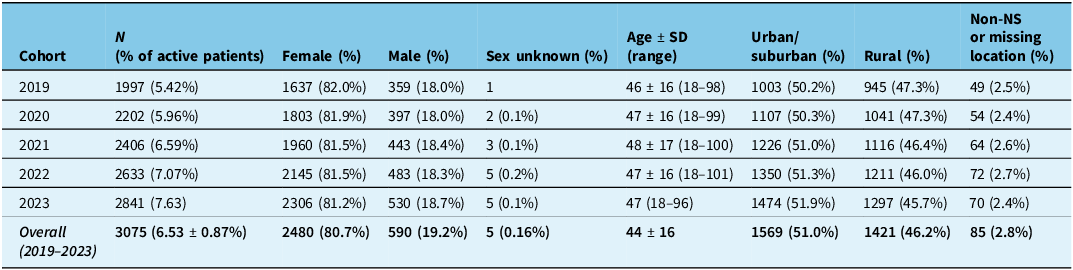
In total, 3075 active patients who have received a diagnosis of migraine were identified in the MaRNet-FP EMR database (6.53% of total patients). Diagnoses included migraine with and without aura, variants of migraine and unspecified migraine. Migraine patients were predominantly female (81%) with an average age of 44 ± 16 years. The geographic location of patients was divided similarly between urban/suburban (51.0%) and rural (46.2%) areas. In a small number of patients (2.8%) seen by MaRNet-FP providers, residential location was identified as out of province or could not be identified due to missing postal code data. Patient demographics across each year of abstracted data are summarized in Table 2.
Table 2. Demographic information of migraine patients in MaRNet-FP EMR

Note: Summary demographic data are presented for active MaRNet-FP patients with a diagnosis of migraine. Data are presented for each annual cohort and as an overall five-year summary. NS = Nova Scotia.
Acute management of migraine
Between 2019 and 2023, 50% of patients with a migraine diagnosis received a prescription for a medication that can be used for the acute management of migraine. Patients with migraine may be prescribed multiple classes of acute medication, so we examined how many distinct classes of drugs were prescribed to individual patients over the five-year period. Patients were most commonly prescribed only one drug class (38.9%), 10.8 % were prescribed two classes of medications, and less than one percent were prescribed three or more. When the classes of therapeutics were assessed, triptans and nonsteroidal anti-inflammatory drugs (NSAIDs) were identified as the most commonly prescribed classes of medications. In total, 33.9% of migraine patients were prescribed triptan medication, and 26.3% were prescribed NSAIDs. Opioids, ergotamines and barbiturates were seldom prescribed (percentage of patients: 1.0%, 0.13% and 0.03%, respectively). For patients who were prescribed a triptan, 40% received only one prescription over the five-year period.
To identify potential changes in the pharmacological management of migraine between 2019 and 2023, prescribing patterns were also examined for each individual year. Annually, the percentage of migraine patients prescribed any acute medication ranges from 21.6% to 30.7% (Figure 1A). Of those that received a prescription, most stayed within one class of drugs in any given year (18.8% to 26.7%). Prescriptions for two or three classes of acute migraine therapeutics were less common (2 classes: 2.7% to 3.9%, 3 classes: <1.0%), and no patients were prescribed four or more classes of acute medications. Triptans were consistently the most common prescription with 14.7% to 20.8% of patients receiving a prescription in any given year (Figure 1B). Nonsteroidal anti-inflammatory drugs (NSAIDs) were prescribed to 8.1% to 13.3% of patients annually, while prescriptions for opioids, ergotamines and barbiturates remained low throughout the five-year period (<1.0% of patients prescribed).

Figure 1. Summary of annual prescribing patterns for the acute management of migraine. The number of distinct classes of acute drugs prescribed to migraine patients in each year from 2019 to 2023 (A). The most commonly prescribed classes of drugs over the same cohort (B). Data are reported as percentages of migraine patients receiving prescriptions.
Preventative management of migraine
Between 2019 and 2023, 60.4% of patients were prescribed a medication that can be used for the prevention of migraine. Patients were often prescribed only one medication class over the five-year period (38.6%), while two and three-classes were prescribed less commonly (13.3% and 5.5%, respectively). A small percentage of patients were prescribed four or more classes of preventative medications (<2.0%). Antidepressant medications and beta-blockers were the most commonly prescribed classes of drugs with 51.6% and 14.0% of migraine patients receiving these prescriptions, respectively. Patients were also prescribed anti-epileptics (7.4%), calcium channel blockers (8.0%) and the angiotensin II receptor blocker, candesartan (4.3%). Fewer than one percent of migraine patients were prescribed CGRP-targeting drugs, Onabotulinum toxin, pizotifen or clonidine.
When annual prescribing patterns were examined, we determined that 41.2% to 45.8% of patients received prescriptions for medications that can be used for the prevention of migraine in any given year (Figure 2A). Migraine patients were most commonly prescribed one class of drugs annually (31.4% to 34.7%). Prescriptions for two classes of medications that could be used as preventative migraine therapeutics were also commonly observed (8.4% to 9.5%), while three and four classes were seldom prescribed (3 classes: 1.0% to 2.2%, 3 classes: <1.0%). No patients were prescribed five or more classes of acute medications in a given year. Annual prescriptions for antidepressants were identified for 33.4% to 37.6% of patients, while beta-blockers were prescribed for 7.5% to 9.3% of patients (Figure 2B). Approximately 5% of migraine patients were prescribed calcium-channel blockers annually (4.5% to 5.4%), with similar prescribing practices observed for antiepileptics (3.5% to 4.6%). Candesartan was prescribed for a minority of patients (1.9% to 3.7%), as were CGRP-targeting drugs, Onabotulinum toxin, pizotifen and clonidine (<1.0%).

Figure 2. Summary of annual prescribing patterns for the preventative management of migraine. The number of distinct classes of preventative drugs prescribed to migraine patients each year between 2019 and 2023 (A). The most commonly prescribed classes of preventative drugs over the same cohort (B). Data are reported as percentages of migraine patients receiving prescriptions.
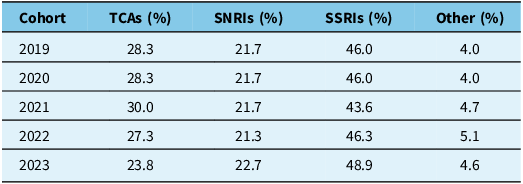
Given that antidepressant use between 2019 and 2023 may have been impacted by the global COVID-19 pandemic, we further analyzed antidepressant prescribing to report the classes of medications (Table 3). The most prescribed antidepressant medications were selective serotonin reuptake inhibitors (SSRIs; range: 43.6% to 48.9% of all antidepressant prescriptions between 2019 and 2023), followed by tricyclic antidepressants (TCAs; range: 23.8% to 30.0% between 2019 and 2023) and serotonin-norepinephrine reuptake inhibitors (SNRIs; range: 21.3% to 22.7% between 2019 and 2023). Approximately 5% of prescriptions were for mirtazapine, which did not fall under another category of antidepressant medications.
Table 3. Breakdown of antidepressant prescriptions based on classes of therapeutics between 2019 and 2023

Note: Proportion of antidepressant prescriptions based on class of therapeutics. TCA = tricyclic antidepressant; SNRI = serotonin-norepinephrine reuptake inhibitor; SSRI = selective serotonin reuptake inhibitor.
Discussion
In our sample of adult patients receiving care by MaRNet-FP primary care providers, annually, 6.53% ± 0.87% of patients were diagnosed with migraine compared to a national prevalence of 8.3%; a statistic which is thought to be an underestimation of migraine prevalence. Reference Ramage-Morin and Gilmour4 This is consistent with existing literature that suggests underdiagnosis of migraine is an ongoing medical issue. Reference Hazard, Munakata, Bigal, Rupnow and Lipton17 Lack of recognition of migraine may lead to undertreatment and unnecessary disability and suffering of patients.
While migraine prescribing practices are understudied in Canada, studies from other countries have reported disparate prescribing rates for acute and preventive medications, Reference Gendolla, Rauer, Kraemer, Schwerdtner and Straube18–Reference Takizawa, Kitano, Iijima, Togo and Yonemoto21 despite evidence that effective use of these therapeutics reduces the risk of disease progression. Reference Hutchinson, Lipton and Ailani22,Reference Lipton, Fanning, Serrano, Reed, Cady and Buse23 Utilizing claims databases, multiple retrospective studies have been carried out to investigate migraine prescribing on a national scale. Reference Gendolla, Rauer, Kraemer, Schwerdtner and Straube18,Reference Sumelahti, Mattila, Sillanmaki and Sumanen20 In Germany and Finland, approximately half of migraine patients receive prescriptions for acute treatments and a quarter receive preventative prescriptions. In Japan, in contrast, claims data suggest that most migraine patients (95.6%) are prescribed an acute migraine medication, while preventative prescriptions are filled by approximately 20% of patients. Reference Takizawa, Kitano, Iijima, Togo and Yonemoto21 Importantly, these studies collected prescribing data from any type of headache provider, including both family physicians and neurologists, who are known to exhibit different prescribing patterns. Reference Fitzek, Overeem and Ulrich24 In the present study, we focused on primary care prescribing and found that about 50% of migraine patients were prescribed an acute migraine medication over the five-year period and 60% received prescriptions for medications which could be used for prevention of migraine. Examining individual years, prescribing fell to 40% or less. While these prescribing rates are higher than those reported by others, it remains less than half. Interpreting EMR data is not without limitations; for example, since NSAIDs and many of the preventative medications examined in the present study are also used for the management of other chronic disorders, the prescribing rates reported herein may be an overestimation of migraine prescribing by primary care providers. Conversely, over-the-counter medications are poorly documented in EMRs, Reference Andrus and Anderson25 which could also contribute to under-reporting of migraine treatment.
The 2013 CHS guideline for the acute management of migraine strongly recommends the use of NSAIDs (naproxen, ibuprofen, acetylsalicylic acid and diclofenac), acetaminophen and triptans (almotriptan, eletriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan and zolmitriptan). Reference Becker and Worthington26 Our findings demonstrate that primary care prescribing patterns in Nova Scotia align with these recommendations where the most commonly prescribed acute therapies were triptans and NSAIDs. Approximately a third of migraine patients identified in the present study were prescribed triptan medication and a quarter were prescribed NSAIDs. We did find, however, that 40% of patients prescribed triptans were only offered one medication from this class. From the literature, we know that it is common to trial multiple types of triptan medications before finding an effective treatment and guidelines suggest trialing at least two medications before deeming the class of drugs failed. Reference American Headache27 Guidelines also support weak recommendations for dihydroergotamine, ergotamine or tramadol for use during severe attacks or when triptans are not available or effective. Prescriptions for these medications were seldom seen in the population examined (≤1.0%). We also evaluated whether barbiturates, which were previously commonly used and marketed for acute migraine treatment, were prescribed to migraine patients despite newer recommendations against their use. We identified very low prescribing rates (0.03%) between 2019 and 2023.
Canadian guidelines for the preventative management of migraine have been published; however, these recommendations have recently been significantly modified since the introduction of CGRP-targeting therapeutics in Canada. Reference Pringsheim, Davenport and Mackie10,Reference Medrea, Cooper and Langman12 Given that these medications are newly available and their entry to the Canadian market falls within our study time period, the prescribing data collected in the present study were primarily compared to the older 2012 CHS guidelines. Real-world prospective studies have demonstrated that CGRP-targeting therapeutics represent a safe, effective treatment option for migraine patients. Reference Caronna, Gallardo and Egeo28–Reference Iannone, Vaghi and Sebastianelli30 Since these new medications are considered first-line therapeutics, their introduction in the Canadian market will likely change future prescribing patterns.
There are several limitations to the current study. Due to the nature of the database used, we cannot know with certainty the indication for a specific medication. Most medications for migraine management have multiple indications (antihypertensives, antidepressants and anti-seizure medications), and patients with migraine may have medical comorbidities that lead to the prescription of these medications. We examined the use of antidepressants further, given potential changes in the use of these medications during the COVID-19 pandemic but identified stable prescribing across classes of antidepressant drugs. We are also unable to report on the use of nonprescription medications, including NSAIDs and supplements, or nonpharmacologic strategies for migraine management. The use of NSAIDs and acetaminophen by migraine patients in this population is likely higher than reported, given that the database does not include the use of analgesics available over the counter. The information available also does not provide data on medication compliance or discontinuation. Finally, we are unable to report if the patients were seen by additional providers beyond the primary care clinicians in the database as this information was not captured, and we cannot assess whether other external factors affected prescribing, such as the COVID-19 pandemic.
Conclusion
This study reports valuable information about the demographics and medication prescriptions for patients diagnosed with migraine in the province of Nova Scotia, Canada, over a five-year time period. Medication choices align with current guidelines; however, not every patient who may have benefited from medications for treating migraine was prescribed such medications. Given the significant disability associated with migraine, every effort should be made to optimize treatment plans, which include the consideration of evidence-based acute and preventative migraine treatment options.
Acknowledgements
Publication of this article was funded by the Department of Anesthesia, Pain Management, and Perioperative Medicine, Dalhousie University Anesthesia Research Fund.
Author contribution
Research project conception: MO, MG, JD, data collection: MO, MG, JD and manuscript writing and editing: MO, MG, JD.
Funding statement
JD has received funding from Abbvie for participation on an advisory board and providing a lecture.
Competing interests
MO has no competing interests to declare. MG has no competing interests to declare.




Target article
Pharmacological Management of Migraine by Primary Care Providers in Nova Scotia
Related commentaries (1)
Reviewer Comment on O’Brien et al. “Pharmacological Management of Migraine by Primary Care Providers in Nova Scotia”