The world population is rapidly ageing as life expectancy increases( Reference Boffetta, Bobak and Borsch-Supan 1 ) and it is common for the elderly to not be able to meet their nutritional needs with diet alone( Reference Hickson 2 , Reference Relph 3 ). Insufficient intake of vitamins and minerals or even borderline deficiency has been linked to numerous conditions among the elderly such as functional decline, frailty and problems with living alone( Reference ter Borg, Verlaan and Hemsworth 4 , Reference Ward 5 ). Although it is difficult to demonstrate a clear cause–effect relationship between chronic disease and nutrition, results from prospective cohorts shows that a poor nutritional status is associated with the development of chronic disease( Reference Heaney 6 – 8 ).
The use of dietary supplements has increased widely in recent years, with the most commonly used supplements being multivitamins, and their use is often recommended if their concentration in the diet is inadequate( Reference Rautiainen, Lee and Rist 9 , 10 ). The risk for exceeding upper recommended intake levels for vitamins and minerals from diet alone is generally low. However, the risk for exceeding recommended intake levels from supplement use is far greater as high amounts of vitamins and minerals can easily be consumed, and the consumption is added to what is obtained from diet( Reference Mulholland and Benford 11 – Reference Renwick 13 ). The upper intake level of micronutrients is the maximum total level of daily long-term intake that is unlikely to cause harm in humans( 10 ).
A number of observational studies have examined the potential benefits of multivitamin supplementation as prevention against chronic diseases and total mortality( Reference Messerer, Hakansson and Wolk 14 – Reference Park, Murphy and Wilkens 19 ). A few cohort studies have not observed an association between the use of multivitamins and lower risk for chronic diseases or mortality( Reference Messerer, Hakansson and Wolk 14 – Reference Park, Murphy and Wilkens 19 ). However, one relatively large prospective study of middle-aged subjects (mean age 62 years at baseline) with a mean follow-up period of 19 years observed an increased risk for total mortality among users of multivitamins compared with non-users( Reference Mursu, Robien and Harnack 20 ). This finding raised concerns regarding the safety of long-term use of multivitamins( Reference Mursu, Robien and Harnack 20 ). Since then, a systematic review has examined the pros and cons of vitamin- and mineral-supplement use from controlled trials and observational studies and found the evidence to be inconclusive( Reference Fortmann, Burda and Senger 21 ).
The aims of this study were to describe supplement use among 5764 elderly Icelanders, examine whether there is a risk for exceeding the tolerable upper level of recommended intake and to investigate whether there was an association between supplement use and total mortality or CVD-related mortality.
Methods
Study population
The data on supplement use in this study were obtained from the Age/gene Environment Susceptibility (AGES)-Reykjavik study, which was conducted by the Icelandic Heart Association. The AGES-Reykjavik cohort was initiated in 2002 and is based on an older cohort, the Reykjavik Study. The Reykjavik study, established to examine risk factors for CVD, was a cohort of 19 381 men and women born between 1907 and 1935 and living in Reykjavik at baseline recruitment in 1967–1991. In 2002, participants of the original Reykjavik study were invited to join the AGES-Reykjavik study. The AGES-Reykjavik study ended in 2006 with 5764 participants recruited( Reference Harris, Launer and Eiriksdottir 22 ).
Informed consent was obtained from all participants in the Reykjavik and AGES-Reykjavik studies. The AGES-Reykjavik study was approved by the Icelandic National Bioethics Committee (VSN: 00-063) and the MedStar Internal Review Board for the Intramural Research Program, Baltimore, Maryland. The Icelandic Heart Association has agreed to the use of the data for this research with written approval from the Icelandic National Bioethics Committee. The study was conducted according to the Declaration of Helsinki.
Data collection
Extensive data were collected at entry to the Ages-Reykjavik study in 2002–2006 through questionnaires and clinical examination in addition to three follow-up visits. Details regarding the methodology of the study have been described elsewhere( Reference Harris, Launer and Eiriksdottir 22 ). Information collected at study entry included information on general health including chronic diseases, supplement and medication use. Biomarkers of health, including serum lipids, were assessed from blood samples. Educational status, smoking status, alcohol consumption, current and past physical activity and other lifestyle characteristics were also recorded in detail. For the purpose of this paper, records on total mortality and CVD-related mortality among AGES-Reykjavik study participants from study entry until the end of December 2009 were extracted.
Assessment of supplement use
For the study-entry examination for the Ages-Reykjavik study, participants were asked to bring their medications and supplements for registration. Names of supplements and frequency of use per week were registered and each supplement was given a specific identification number( Reference Harris, Launer and Eiriksdottir 22 ). Quantitative data for vitamins and minerals in supplements listed on the Icelandic market until 2012 were obtained from The Icelandic Food and Veterinary Authority (MAST). For calculation of the amount of vitamins and minerals used by each participant, the frequency of use per week was taken into account. Total amounts consumed per day on average of vitamins and minerals from all supplements were calculated for each participant using the information from the MAST database. In a number of cases the name of the product did not clearly describe the content and thus the amount of micronutrients in some supplements had to be estimated.
Supplements for the purpose of this paper were defined as vitamins and minerals containing 15 % or more of the intake recommended by the Directorate of Health in Iceland.
Multivitamins were defined as supplements containing at least ten different vitamins or minerals in amounts close to the recommended intake. Most multivitamins included vitamin E, thiamine, riboflavin, niacin, vitamin B5, vitamin B6, biotin, vitamin B12, vitamin C, Zn, Mn, Se and Cr. Many contained vitamins A and D, Mg, Fe, Cu and I. Only a few had Ca, K and vitamin K. Upper intake level and recommended daily intake were defined according to the Directorate of Health in Iceland( 23 , 24 ).
Statistical analyses
To describe the difference between supplement users and non-users at baseline, the two-sample t test was used for normally distributed continuous variables and the Wilcoxon (Mann–Whitney) test was used for variables that were not normally distributed. The χ 2 test was used for categorical variables.
The Cox proportional hazards model was used to calculate hazard ratios (HR) and 95 % CI for the difference in risk for total mortality and CVD-related mortality between users and non-users. The proportional hazard assumption was assessed through visual inspection of the Kaplan–Meier curves. Follow-up time was from the date of study entry until death or the end of 2009 for CVD-related mortality and total mortality. Given the high frequency of multivitamin users among supplement users, this group was analysed separately in the mortality analyses. Although the emphasis in our primary analyses was on comparing supplement users and multivitamin users with non-users, we also grouped users according to the number of supplements used (1, 2, 3, 4+) as well as looked at those who were over the recommended intake level for some vitamins or minerals and compared them with non-users.
Multivariate models were used to adjust for covariates. Variables included as covariates in our proportional hazard models were: age (continuous), BMI (kg/m2) (<18·5, 18·5–25 and >25), education (primary, secondary or higher), physical activity (no activity/almost no activity or those having physical activity in the last 12 months or during midlife (ages 35–49 years)), smoking (current and former smoker) and diabetes mellitus (yes/no), hypertension (yes/no) and history of a CVD event (yes/no). Diabetes mellitus and hypertension were defined as either medication use for these diseases or as self-reported information from questionnaires.
We used two different approaches to impute values for missing covariates. In the case of education (7·5 % missing), missing values were assigned to a missing category and adjusted for by using dummy variables. For BMI (1·2 % missing) missing values were imputed using the mean value from the whole cohort. As for the use of medicines, participants who did not have confirmed use of medicines were classified as not taking them (0–9 % missing, depending on the medication). Lastly, missing values for smokers (3·4 % missing) or ever smokers (3·4 % missing) were changed to ‘not smoking’ values.
Results
The mean age at baseline of participants of the AGES-Reykjavik study was 77 years; 3326 (58 %) of the participants were female and 2438 were male. A total of 4449 (77 %) participants used one or more supplements. The most popular supplement was fish-liver oil, used by 55 % of participants, and the second most common supplement were multivitamins, used by 31 % of participants.
The number of participants in the AGES-Reykjavik study consuming any supplements containing different vitamins and minerals as well as the estimated median daily intake (10th and 90th percentile) can be seen in Table 1. Overall, the intake of vitamins and minerals from supplements was moderate and only few participants exceeded the upper intake levels for most vitamins and minerals. However, 22 % of participants who used vitamin B6 exceeded the upper limit of 25 mg/d for vitamin B6 intake and approximately 10 % of the participants consumed >50 mg vitamin B6 from supplements daily( 24 ). Furthermore 14 % of participants who used Zn exceeded the defined upper intake limits. Several participants were close to exceeding upper limits of vitamin A, vitamin E, Fe and Cu.
Table 1 The amount of vitamins and minerals consumed on average on a daily basis from all supplements by participants of the Age Gene/Environment Susceptibility-Reykjavik study (2002–2006) (Percentages and numbers)
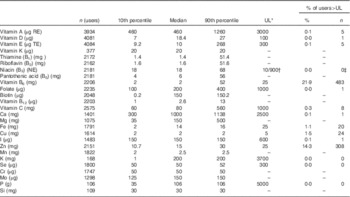
UL, upper intake level; RE, retinol equivalents – 1 RE=1 µg retinol=12 µg β-carotene; TE, α-tocopherol equivalents – 1 α-TE=1 mg α-tocopherol; NE, niacin equivalents – 1 NE=1 mg niacin=60 mg tryptophan.
* UL is the maximum of daily intake unlikely to cause harm.
† Nicotinic acid/nicotine amide.
‡ Most supplements contain nicotine amide and no one exceeded those limits.
In Table 2, descriptive information of all supplement users (4449) and multivitamin users (1788) are compared with non-users. Supplement users were in majority women (60 %), and at entry to the AGES-Reykjavik study (2002–2006) they were on average older (77·1 v. 76·7 years) and had lower BMI (26·8 v. 27·8 kg/m2) than non-users. Users were less likely to smoke (11 v. 15 %) or to have ever been smokers, they drank less alcohol and had higher educational levels than non-users. Users had lower prevalence of diabetes than non-users (12 v. 17 %), but no difference was seen in the prevalence of hypertension. The use of benzodiazepine derivatives, antidepressants, psycholeptics, glucocorticoids and osteoporosis medicines was found to be higher among supplement users compared with non-users, and the use of β-adrenergic blockers, hypoglycaemic medicine, nitrates and statins was higher among non-users. Similar results were seen for multivitamin users.
Table 2 Descriptive information on non-users, supplements users and users of multivitamins from the Age Gene/Environment Susceptibility (AGES)-Reykjavik study (2002–2006) (n 5764) (Mean values and standard deviations; medians and 10th, 90th percentiles)

P 1 and P 2, compared with non-users; Ref., referent values; CRP, C-reactive protein.
* 25-Hydroxyvitamin D (nmol/l).
From recruitment into the AGES-Reykjavik study in 2002–2006 and to the end of the follow-up period on 31 December 2009, there were a total of 1221 deaths and 525 CVD-related mortality cases. The median follow-up time was 5·33 years (30 118 total person-years). The association between the use of multivitamins and total mortality or CVD-related mortality is shown in Table 3. In sex- and age-adjusted models, a significant protective association (HR 0·83; 95 % CI 0·72, 0·96) was observed between multivitamin users and non-users and total mortality. This association disappeared after adjustment for covariates (HR 0·91; 95 % CI 0·77, 1·08). No association was also observed when examining the use of multivitamins in relation to CVD-related mortality (HR 0·91; 95 % CI 0·70, 1·18). The same was observed for any number of dietary supplements used or the use of vitamins or minerals over the upper limit of recommended intake. We investigated whether there was one particular confounding factor driving the non-association, but including the factors in the model one at a time did not reveal that any one of them, in particular, was the most important.
Table 3 The use of supplements and multivitamins and the risk total mortality and CVD-related mortality compared with non-users among Age Gene/Environment Susceptibility-Reykjavik study (2002–2006) participants (n 5764)Footnote * (Hazard ratios (HR) and 95 % confidence intervals)
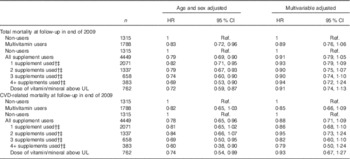
Ref., referent values; UL, upper intake level.
* Results from Cox proportional hazards model. Multivariable adjusted: age, BMI, sex, education, current and midlife physical activity, ever smoker, smoker, diabetes mellitus, hypertension and history of a CVD event.
† Percentage of participants taking multivitamins among those taking 1, 2, 3 or 4+ supplements was 21, 55, 61, 54 %, respectively.
‡ Percentage of participants taking fish-liver oil among those taking 1, 2, 3 or 4+ supplements was 65, 73, 80, 79 %, respectively.
Discussion
This study presents results from the AGES-Reykjavik study in Iceland on supplement use in the older population. The results indicate that a total of 77 % of participants in this study used at least one supplement. A relatively high percentage of participants exceeded upper limits for vitamin B6 and Zn but very few exceeded upper limits for other micronutrients. The results from this prospective cohort did not suggest any association between supplement use and total mortality or CVD-related mortality.
The proportion of supplement users in this study is similar to that in other reports. In the Iowa Women’s Health study, 75 % of women used supplements in 1986 and 85 % in 2004, and the most common supplements were Ca and multivitamins( Reference Mursu, Robien and Harnack 20 ). The most common supplement used by the AGES-Reykjavik study participants was fish-liver oil (55 %) and the second most common was multivitamins. A total of 31 % of participants used multivitamins, which is very similar to what has been reported elsewhere( Reference Rautiainen, Lee and Rist 9 ).
In our population, supplement use was relatively moderate and few participants exceeded the upper limit of recommended intake for most vitamins and minerals from supplements. However, it needs to be noted that contribution from diet was not taken into consideration. An exception was dietary supplement intake of vitamin B6 and Zn. Vitamin B6 is often present in large quantities in B-vitamin preparations and so is Zn in a number of dietary supplements, often in doses higher than the recommended daily intake. According to the Icelandic National Survey of 2010/2011, many participants exceeded daily recommendations for vitamin B6 (63 %) and Zn (80 %) but very few (<1 %) exceeded the upper limit from diet alone( Reference Thorgeirsdottir, Valgerisdottir and Gunnarsdottir 25 ). Our results could be of concern as total amounts obtained from supplements and diet are even higher, and adverse events have been reported for use of vitamin B6 in doses of 50 mg/d and higher for a prolonged period of time( 10 ). Reported adverse effects are neurological, and in extremely high doses vitamin B6 can even be a neurotoxin( 10 ). Others have reported excessive intake of vitamin B6 as well as of other nutrients( Reference Schwab, Heier and Schneider 26 ). A few studies have reported an excessive intake of Zn with the use of supplements( Reference Flynn, Hirvonen and Mensink 12 , Reference Wallace, McBurney and Fulgoni 27 – Reference Waskiewicz 29 ). The main concerns for excessive intake of Zn are effects on Cu metabolism. Lower activity of copper-containing enzymes has been reported when doses of Zn exceed 50 mg/d, and in doses higher than 150 mg/d changes in blood lipids and in immune defenses have been observed( 10 ). The consumption of the AGES-Reykjavik study participants was not so high as to exceed 150 mg.
Participants of the AGES-Reykjavik study were older at baseline than participants of many other similar studies. We however had information on various health factors for the participants during midlife, which were consistent with the information available for later in life and confirmed that users had, in some ways, a healthier lifestyle than non-users. Many others have reported supplement users to be healthier than non-users, which make it difficult to separate the impact of supplements from other health-related factors on chronic disease outcomes( Reference Mursu, Robien and Harnack 20 , Reference Bailey, Fakhouri and Park 30 – Reference Rock 34 ).
Our results do not suggest that multivitamin use increases the risk for total mortality as was reported by the Iowa Women’s Health study( Reference Mursu, Robien and Harnack 20 ). Other cohort studies have come to the same conclusion on no association of multivitamin use and total mortality( Reference Messerer, Hakansson and Wolk 14 – Reference Park, Murphy and Wilkens 19 ) or CVD-related mortality( Reference Rautiainen, Lee and Rist 9 , Reference Messerer, Hakansson and Wolk 14 , Reference Li, Kaaks and Linseisen 17 , Reference Neuhouser, Wassertheil-Smoller and Thomson 18 , Reference Mursu, Robien and Harnack 20 , Reference Muntwyler, Hennekens and Manson 35 ). The observational studies that have reported an association between multivitamin use and statistically significant lower risks for CVD-related mortality tend to include specialised groups with inadequate diets( Reference Messerer, Hakansson and Wolk 14 , Reference Dong, Iso and Kitamura 36 ) or long duration of use( Reference Pocobelli, Peters and Kristal 15 , Reference Bailey, Fakhouri and Park 30 , Reference Rautiainen, Akesson and Levitan 37 ).
There have been only a few randomised controlled trials investigating the effect of multivitamin supplementation on CVD events or CVD-related mortality. The Trial to Assess Chelation Therapy (TACT) trial, a randomised controlled trial, examined individuals with a history of myocardial infarction and administered high-dose multivitamins to the experimental group; however, no effect of the supplementation were observed on CVD-related death (HR 0·80; 95 % CI 0·54, 1·19)( Reference Lamas, Boineau and Goertz 38 ). The SUpplémentation en VItamines et Minéraux Anti-oXydants (SU.VI.MAX) study defined multivitamins in a unique way, the multivitamin used in that study contained five antioxidant vitamins and minerals and contained vitamin C (ascorbic acid), vitamin E, β-carotene, Se and Zn( Reference Hercberg, Kesse-Guyot and Druesne-Pecollo 39 ). The SU.VI.MAX study reported no effects during the supplementation period or in the postsupplement period on ischaemic CVD (risk ratio 0·95; 95 % CI 0·75, 1·20) or mortality (risk ratio 0·77; 95 % CI 0·57, 1·04)( Reference Hercberg, Kesse-Guyot and Druesne-Pecollo 39 ). The third randomised controlled trial included only male participants and reported no effects of multivitamin supplementation on total mortality (HR 0·94; 95 % CI 0·88, 1·02) or CVD-related mortality (HR 0·95; 95 % CI 0·83, 1·09)( Reference Sesso, Christen and Bubes 40 ). None of these studies reported statistically significant effects of multivitamins on total mortality, CVD events or on CVD-related mortality. All three randomised controlled trials however reported slightly lower insignificant risk for CVD incidence or mortality among multivitamin users( Reference Lamas, Boineau and Goertz 38 – Reference Sesso, Christen and Bubes 40 ).
This study has several strengths, one of which is its design; the study included a population-based prospective cohort and information on supplement use was collected during an interview, thus reducing recall bias. Another strength of the study is the number of covariates available, making adjustments for various aspects possible. The median follow-up time was 5·3 years, which may not be such a long time when chronic diseases and mortality rate are examined, but the participants were elderly and a considerable number of events occurred during that time.
Limitations should be pointed out as well. The participants brought the supplement products to the interview, and the name of the product was registered. However, in a number of cases the name of the product did not clearly describe the content and thus the amount of micronutrients in some supplements had to be estimated. This made the amount of vitamins and minerals from supplements an estimation of use. Results from this study include only information on the amount of micronutrients from supplements, thus making the number of participants who exceeded the upper limit likely an underestimation. The use of dietary supplements was only evaluated at baseline and therefore we were not able to estimate duration of use. When conducting a study on the association of supplements and health, it needs to be taken into consideration that users lead in many ways healthier lifestyles than non-users, which could have an effect on other risk factors and mortality. To account for this, multivariate models were used to adjust for confounding factors. Despite efforts to adjust for confounders, the use of supplements could be associated with other health behaviours.
Conclusions
This study provides insight into the use of supplements and consumption of micronutrients from supplements among older people in Iceland. The results from the survival analysis suggested that multivitamin supplements are neither beneficial nor harmful with respect to total mortality or CVD-related mortality. However, almost a quarter of the supplement users exceeded upper limits for recommended daily intake of vitamin B6 and Zn. This could be of concern as total amounts obtained from supplements and diet are even higher and adverse events have been reported for use of vitamin B6 in high doses for a prolonged period of time. Vitamin B6 is often present in large quantities in B-vitamin preparations and so is Zn in a number of dietary supplements, often in doses higher than the recommended daily intake, which is of great concern. Further research is needed to ascertain the full effect of vitamin B6 and Zn supplementation above the upper limit of recommended daily intake.
Acknowledgements
The authors thank the Icelandic Heart Association for the data used in this study.
B. Ó. was supported by the University of Iceland Research Fund (grant no. 1233-123101).
I. G. and T. B. H. formulated the research question. T. B. H. and K. E. designed the study. B. Ó. analysed the data and wrote the article. I. G., T. B. H. and K. E. helped interpret the data and revised the article. H. N., G. E., T. B. H., L. J. L. and V. G. revised the article critically for important intellectual content. All authors approved the final version of the article.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114517001313





