Introduction
The decline in infant mortality was a crucial element in the secular decline of mortality across the Western world during the late nineteenth and early twentieth centuries.Footnote 1 Prior to the first demographic transition, life expectancy at birth was low, largely due to high rates of infant and child mortality.Footnote 2 As the transition progressed and more children survived the first hazardous years, life expectancy at birth increased substantially. The causes of this secular decline in infant mortality have been extensively studied.Footnote 3 While factors such as breastfeeding, improved hygiene, and better infant care have been widely stressed as main drivers of the mortality decline, their relative importance varied by time and place.
Current research on historical infant mortality increasingly incorporates individual-level, cause-specific death data to gain a deeper understanding of this mortality decline. This approach enables an improved identification of the main factors responsible for the decline, as it allows for the connection of certain cause-of-death groups to specific factors, such as improved living conditions, environmental circumstances, or public health interventions.Footnote 4 The recent and ongoing digitisation of individual-level cause-of-death records maintained by civil, church, and hospital authorities has greatly benefited studies on mortality, enabling scholars to access a wealth of detailed information for their analyses.Footnote 5 However, studying causes of death in the past, particularly for infants, can be challenging due to the often vague descriptions of symptoms rather than actual diseases.Footnote 6 Infantile convulsions – in historical medical handbooks often addressed in Latin as eclampsia (infantum) with symptoms that resemble an epileptic attack – is a notable example of such a case.Footnote 7 As convulsions can occur as a symptom of various underlying diseases, the specific physiological meaning remains unclear, posing a complex challenge for scholars studying infant mortality. Given the large prevalence of convulsions-related mortality in historical populations, particularly among infants, it is crucial to understand convulsions as a meaningful cause-of-death category to avoid misclassifications and to ensure accurate interpretation of infant mortality differentials.
Moreover, the use of the term convulsions may have varied over time and across different localities. Since it describes a symptom rather than a clearly defined disease, physicians may have relied less on this terminology as registration practices of illnesses and causes of death became more professionalised. Gaining a deeper understanding of how the once-common term convulsions was used over time and place offers valuable insights into medical practices, the improvement in the accuracy of cause-of-death registration, and the broader process of medicalisation.
Despite the prevalence of convulsions as a cause of death in the past, research on its interpretations and patterns over time and place has received limited scholarly attention. The prevailing narrative, often based on the German usage of convulsions as a cause of death in the research conducted by Kintner, identifies convulsions as a probable substitute for water- and foodborne infectious diseases.Footnote 8 Other scholars are more hesitant about the actual meaning of convulsions and have labelled it as ill-defined or even excluded it from their analyses due to the lack of clarity surrounding the term.Footnote 9 While this increases the reliability of the remainder of the studied causes of death, much information is lost when resorting to this second solution, especially when the number of deaths due to convulsions was large indeed. Further research discussing factors that impacted the chance of being diagnosed with convulsions is still lacking. Therefore, a more nuanced and comprehensive approach is needed to improve our understanding of the meaning of convulsions as a cause of infant mortality in the past, as this may enhance our understanding of infant mortality itself and medical practices regarding infants across Europe.
The main purpose of the paper is to understand how the term was used over time and space in order to enhance the interpretation of large numbers of deaths from convulsions in historical infant mortality. We use a comparative and mixed-methods approach that combines qualitative analysis of historical medical interpretations of convulsions with quantitative analyses of infant deaths from convulsions. We adopt a comparative approach, shifting focus from the well-studied British Isles to explore potential local differences or similarities on the European continent. This allows us to gain a more comprehensive understanding of how the term convulsions was used as a cause of death across various regions of the continent. To achieve this, our study draws upon historical medical literature and individual-level cause-of-death data from four European cities: Amsterdam (the Netherlands), Hermoupolis (Greece), Maastricht (the Netherlands), and Rostock (Germany), covering the period from 1800 to 1955. This study is distinctive in its breadth and depth, offering valuable insights into how infantile convulsions were recorded as a cause of death across these four diverse historical populations, thereby contributing to the existing literature.
After reviewing the relevant literature, we discuss the combined study population and the distinct historical contexts. Cause-of-death reporting was influenced by various factors, including contemporary legislation and prevailing social and medical views, which we address next. We then explore what contemporary physicians understood about infantile convulsions, including the underlying illnesses and disorders, risks and predispositions based on contemporary medical literature from the Netherlands, Germany, and Greece. Finally, our study adopts a quantitative approach to analyse individual-level cause-of-death data, examining patterns and individual determinants of how convulsions were reported across various times and places.
Infantile convulsions in historical research
The frequent recording of infantile convulsions as a cause of death in historical data has triggered an ongoing debate about how to best interpret these cases. A central focus of this debate is the type of causes of death that convulsions may have substituted. Many scholars have argued that deaths attributed to convulsions in the nineteenth and early twentieth centuries should, to some extent, be reclassified under the broader category of water- and foodborne infectious diseases.Footnote 10 Kintner, for instance, suggested that convulsions in Germany were likely related to gastroenteritis and/or diarrhoea.Footnote 11 Other scholars treated convulsions as an ill-specified cause of death due to the large variety of possible interpretations of the term.Footnote 12 Reid, for instance, argued that evidence is lacking to suggest that convulsions in postneonatal infants served as an indicator of any particular alternative cause of death in Derbyshire (England).Footnote 13 Whereas Van Poppel suggested that convulsions in the Hague (the Netherlands) were related to both airborne infectious diseases and water- and foodborne infectious diseases, the evidence was inconclusive, as the disease patterns did not align.Footnote 14
To better understand convulsions as a cause of death, others have considered the age at death. Galley and Woods showed that in England and Wales, the term convulsions was used to describe infant deaths caused by exogenous factors linked to the postneonatal environment and by endogenous factors associated with congenital defects and birth trauma within the first few days of life.Footnote 15 They argued that while convulsions were more closely associated with exogenous causes, they were also significant as causes of death in the early neonatal period. Some deaths attributed to convulsions were likely linked to endogenous factors. Similarly, Jaadla and Puur classified convulsions under the category of water- and foodborne infectious diseases for deaths in Tartu (Estonia) on the premise that the death had occurred after the first two weeks of life.Footnote 16
Several studies have analysed seasonality patterns to compare convulsions-related mortality with other disease categories. For instance, summer mortality peaks are typically associated with water- and foodborne infectious diseases, while winter peaks are characteristic of airborne infectious diseases. However, in both Trondheim (Norway) and Sheffield (England), no clear summer peaks in convulsions-related mortality were observed.Footnote 17 More recently, Breathnach and Gurrin argued that convulsions were a catch-all term disproportionately applied when the precise illness was unknown, at least in Dublin (Ireland).Footnote 18 Their research has revealed that a variety of conditions, from brain congestion to whooping cough, were categorised as convulsions. Even acts of violence were sometimes sanitised under this category.Footnote 19
The different approaches to classifying convulsions as a cause of death can be valid, as interpretations and reporting practices likely varied depending on local and/or temporal circumstances. Historical cause-of-death reporting was highly dependent on regional contemporary institutional and legal frameworks, medical knowledge and practices, and prevailing social views.Footnote 20 As a result, comparisons of causes of death across different times and places are complicated by a shifting understanding of disease, changes in diagnostic nomenclatures, nosologies, and evolving recording practices.Footnote 21 Until national legislation standardised cause-of-death reporting, individual physicians may have used their own preferred terminologies to describe certain causes of death, influenced by their training, receptiveness to new ideas, and personal habits.Footnote 22 This implies that classification methods effective in certain historical settings may not be directly applicable in others. Consequently, Hardy argued that in using local registration figures, one must take the local context into account, with ‘due reference to local certification levels, problems of allocation, and indications of incidence’.Footnote 23
Research has shown that reported causes of death also reflected differences in medical provision.Footnote 24 Physicians often preferred to work in urban areas and/or serve wealthier patients, leaving rural areas, poorer regions, and less affluent individuals underserved.Footnote 25 Evidence has also revealed that access to medical care was unevenly distributed within families, with infants and the elderly frequently receiving less attention.Footnote 26 In some families, the belief prevailed that intervening to save ‘hardly viable infants’ would disrupt the natural order.Footnote 27 Consequently, many families chose not to risk the financial burden of consulting a physician for those who did not contribute to the livelihood of the family and were unlikely to recover.Footnote 28 The varying patterns of medical consumption among different groups of people and regions may have influenced the accuracy and reliability of post-mortem examinations, where and when they existed, as well as how causes of death were certified and reported. When the physician had not previously attended the deceased, they had to rely on accounts from non-medically trained eyewitnesses.Footnote 29 Convulsions were a visible, well-known, and alarming symptom that bystanders, often family members, were likely to observe and report to the physician as the apparent ‘illness’ rather than identifying the underlying, less visible cause.Footnote 30
Given the importance of historical context in the use of the term convulsions, a comparative analysis is essential for a deeper understanding of this cause of death. Such an analysis can help identify the factors that influenced how the term was used in different contexts.
Four different European cities and sources
The distinct characteristics of the four European cities make them well-suited for a comparative study (see Table 1). However, the selection was also driven by the availability of reliable data. The cities represent diverse geographic regions, with three northern European cities: Amsterdam, Maastricht, and Rostock, and one southern European city, Hermoupolis in Greece.
Table 1. Major characteristics of the cities of Amsterdam, Hermoupolis, Maastricht, and RostockFootnote 31
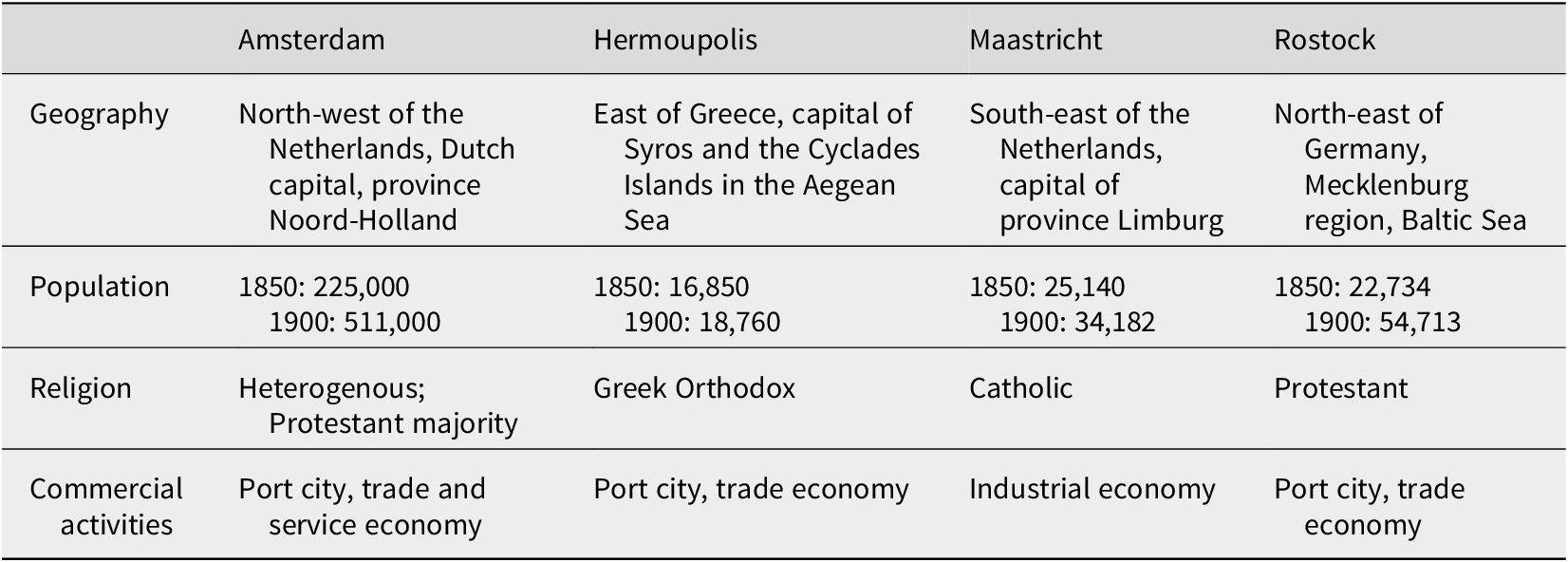
In terms of size, Amsterdam was already considered a relatively large city, while the other three cities were small to medium-sized. The smallest amongst the four, Hermoupolis, had a population of 17,000 inhabitants in 1850, whereas Amsterdam was significantly larger with 225,000 inhabitants.Footnote 32 Rostock and Maastricht were only slightly larger than Hermoupolis, with 23,000 and 25,000 inhabitants, respectively. By 1900, Rostock and Amsterdam had doubled in size, while Hermoupolis and Maastricht grew at a slower pace. Other distinct differences between the cities can be seen in their dominant religions. Maastricht was almost homogeneously Catholic, Rostock was predominantly Protestant, and Hermoupolis Greek Orthodox, while Amsterdam was relatively heterogeneous, with a slight Protestant majority. In terms of economic focus, Maastricht was an exception, as it was the only city of the four which did not function as an important port city. Instead, it thrived from its flourishing industry from the 1840s onwards. Contrarily, the other three cities relied more on trade through their functions as port cities. In the seventeenth century, Amsterdam was a large seaport and staple market and an important city in a global network of trade. At the beginning of the nineteenth century, however, its economic power had evaporated. Until the 1870s, the city went through a period of stagnation and decline, followed by a strong economic recovery that lasted well into the twentieth century. Rostock was an important port city on the Baltic coast and one of the earliest and most influential members of the Hanseatic League, shaped by trade, seafaring, and its university. Despite this, Rostock’s population had stagnated between 5,000 and 15,000 for centuries before the onset of the nineteenth century. However, from the 1850s onwards, moderate industrialisation and urbanisation sparked accelerated population growth. Hermoupolis, the capital of Syros and the Cycladic islands, was the second largest and wealthiest city in the new Greek kingdom and a key port in the Eastern Mediterranean. However, it faced a financial crisis in the following decades, leading to unemployment and outmigration. In the early twentieth century, investments in the textile industry stabilized the economy, and the population eventually stabilized around 18,000, briefly increasing due to Greek Orthodox refugees from Asia Minor.
The selection of these cities enables us to compare northern European cities with a Southern European city while also considering differences in size, religious composition, and economic characteristics and development. Moreover, including two cities from the same country allows us to examine the influence of the national context. Did the national context drive uniformity in cause-of-death registration practices, or was there significant local variation?
For the qualitative component of this study, we examined nineteenth- and early twentieth-century medical handbooks, clinical case reports, medical journals, and various other sources from Germany, Greece, and the Netherlands. A comprehensive list of these sources can be found in Appendix 1.
For the quantitative analyses, we use historical cause-of-death registration. Access to historical, individual-level, cause-specific mortality data remains limited despite the increasing number of such datasets being constructed for several European cities and localities. For our individual-level analysis, we utilised civil death registers from Hermoupolis and Amsterdam, cemetery registers from Maastricht, and church registers from Rostock.Footnote 33 The cause-of-death information from Rostock and Maastricht covers the longest periods, specifically 1800–1904 and 1864–1955, respectively. The period of the Amsterdam data is slightly shorter, however still remarkably long ranging from 1856 to 1926. Meanwhile, Hermoupolis provides cause-of-death information for intermittent years between 1876 and 1916, after which such information becomes systematically available up to 1940. The combined dataset contains 144,864 records of infant deaths.Footnote 34
Although civil registration has been available continuously for the entire population of Hermoupolis since 1859, causes of death have been recorded only since 1916, along with the name of the doctor who confirmed the death and specified the cause of death.Footnote 35 Prior to that, cause-of-death information is only available in so-called draft death registers for specific periods: 1876–1879, 1892–1898, 1902–1903, and 1912–1913. For this study, the draft death registers, which list all deaths that occurred in Hermoupolis during these years, were linked to civil death registration data to verify the accuracy of the information and completeness of the dataset.Footnote 36 For the period 1916–1940, infant deaths were obtained from the civil death registers, which have been transcribed into the Hermoupolis Mortality Database. The annual total numbers of births are used for calculating the infant mortality rates (IMRs) for the four cities. Information on the sex of the newborns is not available for Hermoupolis, as the birth registers have only been counted and not transcribed, resulting in the unavailability of sex-specific rates.
In the Netherlands, national cause-of-death registration was mandated by law starting in 1865.Footnote 37 This legislation specified that the cause of death should be reported by a physician rather than a mere witness to the death. However, Amsterdam was a forerunner, having begun cause-of-death registration as early as 1854. The municipality of Maastricht started its registration in 1864, probably incentivised by the expected new legislation.Footnote 38 As a result, both cities maintained detailed and reliable causes-of-death registers. The Amsterdam registers used in this study cover the period 1856–1926 with two missing years, 1892 and 1893, and data gaps in the years 1858, 1894, and 1899. The Maastricht Death and Disease Database provides causes-of-death information for all deaths that occurred in the city from 1864 to 1955. To enhance database comprehensiveness, all cause-of-death records were manually linked to information from death certificates.Footnote 39 Annual numbers of live births by sex are derived from the statistical yearbooks for the municipality of Amsterdam, considered highly accurate, as well as from civil birth registers and aggregate statistics for Maastricht.Footnote 40
In Rostock, civil cause-of-death registration had not yet been introduced at the time under study. Only after 1924, participation in ‘national’ cause-of-death statistics instituted in 1891 became truly nationwide.Footnote 41 The German sample, therefore, relies on the previously transcribed burial registers of Rostock’s St. Jakobi parish spanning the period from 1800 to 1904, which contain information on causes of death, supplemented by information from baptismal registers, which provided the annual numbers of live births by sex.Footnote 42 St. Jakobi constituted Rostock’s New Town in the western part of the city’s historic centre and was by far the largest of the four old Rostock parishes. Between 1827 and 1875, the share of Rostock’s live births occurring in St. Jakobi rose steadily from thirty-nine to sixty-one per cent. In addition, St. Jakobi was the most balanced parish in terms of social structure, while the other three parishes were either wealthy or poor. For these reasons, we consider St. Jakobi representative of the city. Although the cause-of-death annotations in the Rostock church registers were made by pastors instead of physicians, evidence from clerical statute books suggests that pastors in the Mecklenburg-Schwerin region possessed basic medical knowledge.Footnote 43
The lack of a uniform classification complicates the comparison of reported individual-level causes of death between different localities due to differences in nomenclature and registration practices.Footnote 44 Over time, these issues became less important as professionalisation of registration was on its way. By using causes of death that were already coded to ICD10h, version 2020, we overcame the issues of comparability. ICD10h is a historical coding system for causes of death that is applicable across countries and languages.Footnote 45
Medical knowledge of infantile convulsions
The root of medical knowledge in the Netherlands could be traced back to Germany, as most medical literature in the former two countries concerned translations from the German discipline in the nineteenth century. In Greece, reliance on French literature transitioned towards a focus on German medical literature in the early twentieth century. First, our objective was to explore the various synonyms and types of convulsions mentioned in this historical medical literature. In the historical literature from Germany, the Netherlands, and Greece, distinctions were drawn between the usage of Latin, vernacular, and regional terms for convulsions. Latin terms such as eclampsia and convulsiones were frequently employed, sometimes with adjectives specifying age groups: eclampsia/convulsiones neonatorum/infantum/puerilis/puerorum (neonatal/infantile convulsions). Vernacular synonyms including Eklampsie in Germany, eklampsia in Greece, and terms such as eklampsie, convulsiën ( convulsions ), hersenkoortsstuipen ( brain fever convulsions ) and (algemene) (kinder)stuipen ( children’s convulsions ) in the Netherlands, along with more general terms as Krämpfe (cramps, in Germany) and spasmoi (spasms, in Greece), were prevalent.Footnote 46 Regional synonyms or words in the local dialect referring to convulsions or cramps were also mentioned in the historical medical literature, as Gichter used in south-west Germany and Frais in the south-east.Footnote 47 In north-eastern Germany, other more general terms were used to describe infantile convulsions, such as Jammer (misery), Elend (woe) and Not (agony).Footnote 48 Further specificity was added through adjectives, detailing circumstances. For instance, the Dutch term stille stuipen (silent convulsions) indicated instances where parents sought medical assistance in the early morning due to infants passing away in silence during the night.Footnote 49 In Greece, the circular regarding the declaration of causes of death stated that if eclampsia occurred during childbirth, it was to be reported as epilocheios eclampsia (Latin, pre-eclampsia), referring to mothers rather than newborns.Footnote 50
In the German/Dutch literature, further specifications revolved around the categorisation of eclampsia into different types based on underlying illnesses. This included idiopathic (primary, direct, or ‘organic’) and deuteropathic (secondary, indirect, functional, or ‘reflective’) convulsions, distinguishing those originating in the brain/spinal cord and those elsewhere in the body, causing a reaction in the brain or nervous system.Footnote 51 Subdivisions further detailed eclampsia toxica, eclampsia gastrica, eclampsia dentitionis, and eclampsia febrilis, representing convulsions caused by intoxication, gastrointestinal problems, teething, and feverish diseases, respectively.Footnote 52 To differentiate between eclampsia and cramps or a milder form of convulsions, new synonyms emerged, such as convulsiones simplices (cramps in the spinal cord, face, or diaphragm), affectkrampen or woedekrampen (cramps caused by strong emotions), and inwendige stuipen or binnenstuipen (internal convulsions), representing a milder manifestation of eclampsia caused by gastrointestinal problems.Footnote 53 The historical literature also outlined spoken terminologies for a milder form: Terminen in north-eastern Germany, and torminen, termijntjes ( periodic cramps), groeiertjes/groeistuipen (growing pains) in the Netherlands.Footnote 54 In all three countries, the use of a diverse array of Latin, vernacular, and regional terms characterised the description of convulsions in medical literature. To identify effectively convulsions as the cause of infant death in historical cause-of-death reporting, an awareness of this broad spectrum of synonyms and types is crucial.
The next objective was to explore the diseases linked to infantile convulsions in medical literature over time. In nineteenth-century German/Dutch medical literature, it was explicitly stated that convulsions were symptomatic by nature and could be associated with various illnesses and disorders.Footnote 55 These illnesses could be broadly categorised into four types: congenital and birth disorders, various infectious diseases, non-infectious diseases, and disorders resulting from external causes such as hyperthermia and potentially harmful sleeping potions containing alcohol or poppies (sirupus papaveris).Footnote 56 In Greece, the recognition of convulsions as a symptom associated with other illnesses, such as childhood diseases and gastro-intestinal problems, emerged in the early twentieth century.Footnote 57 Changing medical insights evoked continuous changes to the list of underlying medical causes in German/Dutch literature over time. Newly discovered underlying illnesses and disorders were incorporated into the expanding list, while some causes, such as teething and strong emotions of a hypersensitive breastfeeding mother or wet nurse, were dismissed.Footnote 58 The German professor Carl Friedrich Canstatt (1807-1850) challenged the prevailing belief in England and North America that teething was the primary cause of convulsions.Footnote 59 Hence, medical literature not only reflected a changing variety of underlying causes over time but also regional differences of opinion on the primary causes of convulsions.
Finally, we investigated the medical and non-medical factors considered by nineteenth- and early twentieth-century physicians when identifying children with a predisposition or higher risk of convulsions. In particular, potentially fatal combinations of convulsions with specific illnesses could provide insights into historical causes of death masked by convulsions. Although the terminology evolved, nineteenth-century German/Dutch medical authors noted similar predispositions to convulsions: anaemia, a tendency to rickets and tetany, as well as hereditary syphilis.Footnote 60 The presumed association of convulsions with hereditary syphilis was also reported in the Greek medical journal Iatrike Proodos in the early twentieth century, establishing this relationship widely in Greece.Footnote 61 However, in 1920, Dutch paediatrician Evert Gorter concluded that, besides neuropathic disorders, tetany was the only predisposition to convulsions in children.Footnote 62
German/Dutch and Greek literature also identified specific non-medical risk factors that increased the likelihood of children, especially infants, experiencing convulsions. The primary risk factors were poverty, poor living conditions, and artificial feeding.Footnote 63 These observations suggest a potential relationship between convulsions and water- and foodborne infectious diseases, given that the absence of breastfeeding was a substantial risk factor for infants to contract gastrointestinal infections that could spread through contaminated water and/or nourishment. Additional risks stemmed from small, poorly ventilated, and overcrowded houses which lacked fresh air, according to the medical literature. This points to a possible connection of convulsions with airborne infectious diseases, which tend to spread easily in such overcrowded and poorly ventilated dwellings. According to others, infants’ clothing was often inadequate for maintaining an appropriate temperature in a single-room house where washing and cooking also took place.Footnote 64 This environment rendered young children susceptible to hyperthermia, potentially resulting in coma and fatal convulsions. Additionally, the literature highlighted the widespread practice of having infants sleep in the parental bed, which was usually a cramped and poorly ventilated cupboard bed or alcove. Despite nationwide warnings, this habit persisted in the Netherlands, leading to cases of infants who had died in bed during the night. While parents often attributed these deaths to convulsions, attending physicians indicated that the true causes were hyperthermia and suffocation.Footnote 65 All these observations seem to link an increased risk of convulsions to poverty and poor infant care, but caution is needed to avoid blaming the poor for adhering to ingrained traditions presumed to harm infants as better-off contemporaries often did.
The historical literature provided limited information regarding the prognosis and fatality of specific combinations of convulsions and underlying illnesses. Available information mostly referred to dangerous and less dangerous combinations. German/Dutch authors considered convulsions caused by disorders and illnesses in the brain or spinal cord, such as meningitis, hydrocephalus, brain oedema, encephalitis, brain tumours, or intracranial haemorrhages, as dangerous. They also regarded convulsions resulting from tetany or spasmophilia, hyperthermia, and whooping cough as risky.Footnote 66 In her inaugural lecture of 1927, Professor Cornelia de Lange highlighted the risk associated with convulsions caused by kindertetanie (tetany in children) or spasmophilie (spasmophilia), noting that ‘many children died from it in the past’.Footnote 67 Contemporary physicians reported that tetany, like rickets, was more prevalent in spring, at least in the Netherlands.Footnote 68 Towards the end of the 1930s, tetany was diagnosed much less, and their outbreak in late winter and spring was slowly disappearing, according to De Lange.Footnote 69 Reid and Garrett, on the other hand, recently argued that tetany, believed to be caused by calcium deficiency and underlying vitamin D deficiency, and the bacterium-based neonatal tetanus exhibited similar symptoms.Footnote 70
Convulsions resulting from diseases that induced fever were generally considered less dangerous, especially when related to skin rash diseases.Footnote 71 Moreover, there were conflicting views among German/Dutch authors regarding the risks of convulsions caused by gastro-intestinal problems in infants, with some physicians arguing for a better prognosis and resolution with vomiting stimulated by a feather and/or an intrarectal enema.Footnote 72
To summarise, while the Latin term eclampsia (infantum) was widely used in historical medical literature from Germany, the Netherlands, and Greece, understanding the full range of synonyms and types is crucial when studying individual-level cause-of-death reporting, especially when uniform cause-of-death registration had not yet been introduced at the time under study. The medical literature reflected a changing variety of underlying causes over time with newly discovered illnesses being incorporated into an expanding list while others were removed, and variations in interpretations among individual authors, even within the same linguistic tradition. German and Dutch authors presented new medical insights regarding underlying illnesses much earlier than their Greek counterparts. Additionally, information on the prognosis and fatality of specific combinations of convulsions and underlying illnesses was scarce and inconsistent, with significant differences in interpretation even among authors from the same country.
Convulsions in cause-of-death registers
For the investigation of convulsions mortality patterns, we used causes of death coded according to the newly established ICD10h. These were then categorised into the infant categorisation (namely ‘infancat’), which consists of eleven disease categories based on aetiology.Footnote 73 This categorisation allowed for the consistent classification of all convulsions-related mortality to a specific convulsions category. We distinguished infant deaths between two age groups: neonatal deaths, occurring up to and including twenty-eight days of age, and postneonatal deaths for the remainder of the first year of life (>twenty-eight and <365 days).Footnote 74 Stillbirths were excluded from the analyses.Footnote 75 We subsequently calculated infant mortality rates (IMRs) by cause-of-death category, age group and sex.
The first objective of the analysis was to investigate the share of infant deaths attributed to convulsions relative to total infant mortality and how this changed over time. We expected that the proportion of infant deaths due to convulsions steadily declined as medical knowledge advanced and the registration of causes of death professionalised. Figure 1a shows that all four cities experienced high IMRs in the nineteenth century. The data for Rostock, which date back to the start of the century, reveal a marked increase in infant mortality starting in the 1840s. By the second half of the nineteenth century, IMRs of all four cities were relatively similar, roughly around 200 deaths per 1000 live births. However, the decline in infant mortality started at different periods. While we do not observe a decline in infant mortality in Rostock during this period, IMRs in Amsterdam had improved already as early as the 1880s. Maastricht’s infant mortality decline lagged by four decades, despite being in the same country. Hermoupolis followed a pattern more similar to Maastricht, although its decline took a few additional years to take hold.
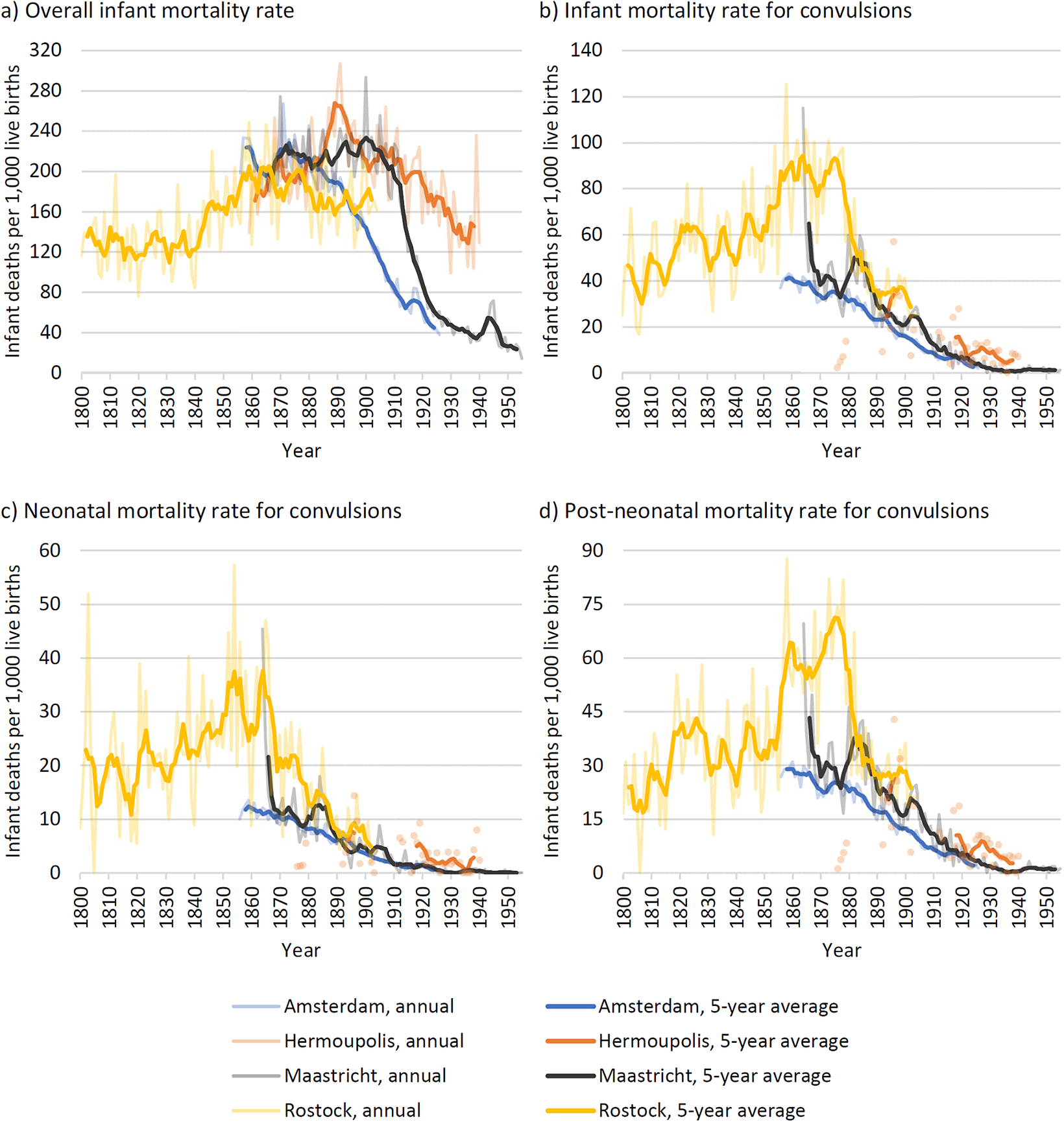
Figure 1. Infant mortality rates in Amsterdam, Hermoupolis, Maastricht, and Rostock.Footnote 76
The patterns of convulsions-related infant mortality were quite distinct, as is displayed in Figure 1b–d. In all four populations, convulsions were more frequently associated with post-neonatal mortality than neonatal mortality. However, the use of the term varied significantly between the cities. The patterns for postneonatal mortality were particularly intriguing. In Rostock, which experienced the highest convulsions mortality, there was a distinct period from 1850 to 1880 when the term was most prevalent. Rostock expanded beyond its city walls in these years, so the composition of our study population, the St. Jakobi parish, might have changed. It is also plausible that infant deaths from the cholera epidemic in 1859 contributed to the peaks of convulsions mortality at the end of the 1850s and early 1860s. Interestingly, the decline in convulsions mortality did not align with a reduction in infant mortality in Rostock. On the contrary, it dropped remarkably in the 1880s, when overall infant mortality stagnated. So, the decline in convulsions occurred even before the unification of the state classifications in 1891.Footnote 77 In a similar vein, convulsions mortality dropped massively just after the introduction of cause-of-death registration in Maastricht. As such, the decline in convulsive mortality coincided with the professionalisation of registration practices but not with a decline in total infant mortality. The peak observed in Maastricht in the mid-1860s could potentially be attributed to infant deaths resulting from a scarlet fever outbreak in 1864 and a cholera outbreak in 1866. In Amsterdam, convulsions mortality was already much lower compared with Rostock and Maastricht, yet the decline in its use occurred before the decline in infant mortality started. The convulsions patterns in Hermoupolis presented a more ambiguous picture, with rates ranging from extremely low (1876–1879) to occasionally high compared to the other cities, particularly in the 1890s. Although a clear explanation for this extraordinary peak cannot be provided, it may be associated with the smallpox and whooping cough epidemics that occurred in the city during the 1890s.Footnote 78 Although causes of death for Hermoupolis were only available for a sporadic span of years, it seemed that the cause of death convulsions was less used when Greece formally adopted the ICD-3 in 1921.
To better understand these intriguing convulsions mortality patterns, it was helpful to scrutinize trends in the broader causal mortality categories into which all infant deaths were classified. Specifically, categories that exhibited rising neonatal and postneonatal mortality rates while the respective rates of convulsions were declining might offer further clues. Given that the total infant mortality did not decline during the same period, it is unlikely that the reduction in convulsions-related mortality reflects a genuine epidemiological shift. Instead, these deaths were probably being recorded under different terms. Advances in medical practices and registration likely led to more accurate cause-of-death reporting, reducing vague categories like convulsions.
Figures 2 and 3 display the infant mortality rates divided into distinct categories of causes of death for neonatal and postneonatal mortality, respectively. Among neonatal mortality (Figure 2), different trends emerged across the different localities. In the two cities where convulsions were most prominent, Rostock and Maastricht, differences in mortality appeared between mortality due to weakness and convulsions. As convulsions declined, there was a slight increase in deaths attributed to weakness. Moreover, in Maastricht and Amsterdam, an increase in congenital and birth disorders coincided with the decline in convulsions mortality. However, in Amsterdam, it was uncertain whether the rise in congenital and birth disorders was directly related to the decline in convulsions or more correlated with the simultaneous decrease in the weakness category. The patterns in Hermoupolis were more difficult to interpret. While convulsions-related mortality was present throughout the study period, it became more noticeable in the 1890s and 1910s, albeit at a much lower level than in the other three cities.

Figure 2. Cause-specific neonatal mortality rates in Amsterdam, Hermoupolis, Maastricht and Rostock.Footnote 79
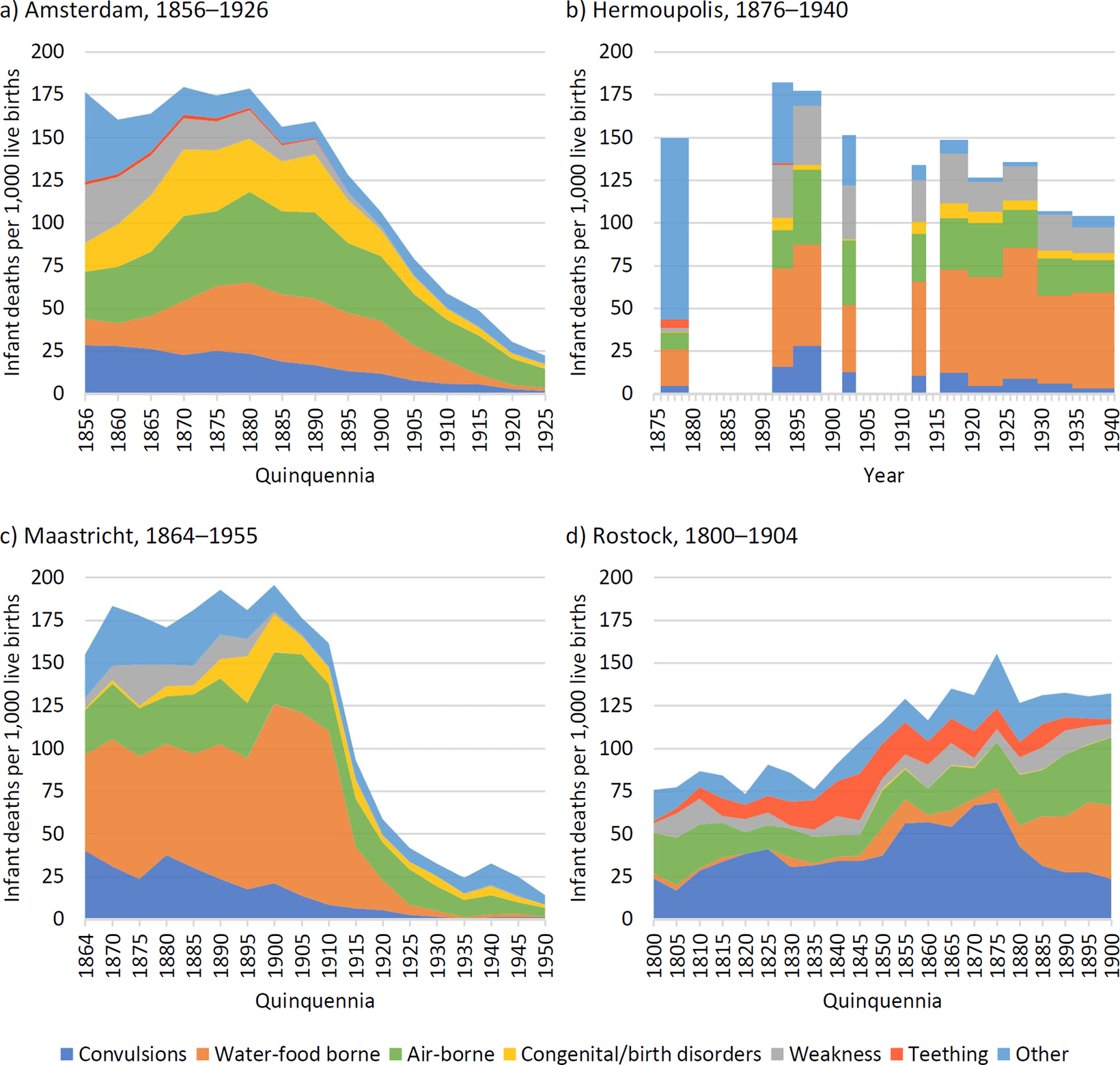
Figure 3. Cause-specific postneonatal mortality rates in Amsterdam, Hermoupolis, Maastricht, and Rostock.Footnote 80
The cause-specific mortality patterns among postneonatal deaths varied across the cities (Figure 3a–d). In Maastricht and Rostock, the trends seemed to support the idea voiced by Kintner that convulsions were used to describe water- and foodborne infectious diseases. In both cities, as mortality rose, mortality due to convulsions declined. Amsterdam also experienced a slight increase in water- and foodborne infectious diseases, but unlike the other two cities, this was not immediately followed by a decline in convulsions, which occurred only later. In Hermoupolis, the relationship between the ‘other’ category and convulsions appeared stronger than with other categories.
Further insights about how the term convulsions may have been used can be obtained from a seasonality analysis. Whereas a summer mortality peak may be associated with higher incidence of water- and foodborne diseases, a winter peak would suggest increased mortality from airborne infectious diseases. We first investigated seasonal patterns by age group, presenting infant mortality from convulsions broken down by calendar month for the entire period per city. Given that the meaning of convulsions likely changed over time, we also analysed seasonal patterns of postneonatal convulsions mortality in Amsterdam, Maastricht, and Rostock broken down in shorter periods. For Hermoupolis, these patterns were calculated around the available periods.
As expected, the seasonal patterns of convulsions in the neonatal group were not in line with the infectious diseases’ patterns. Apparently, exogenous factors did not play a dominant role in neonatal convulsions mortality. Therefore, we focussed on the seasonal patterns in the postneonatal group (Figure 4), also because the numbers of deaths per month in the neonatal group from Rostock, Maastricht, and Hermoupolis were small. The patterns of the neonatal group are shown in a supplement (Figure 7).
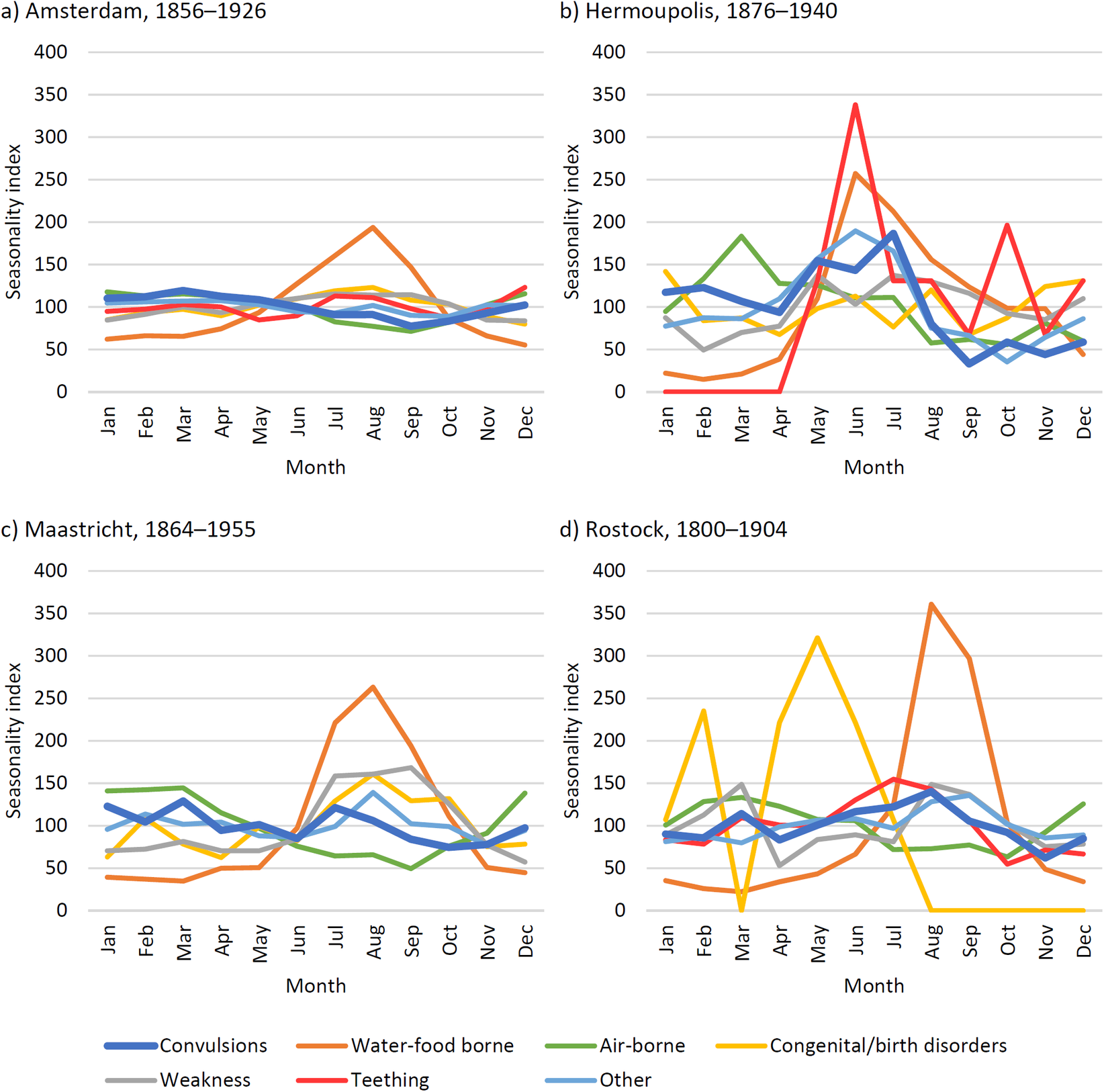
Figure 4. Cause-specific seasonality ratios for postneonatal deaths in Amsterdam, Hermoupolis, Maastricht, and Rostock.Footnote 81
Throughout the entire study period, the seasonality patterns of convulsions for postneonates followed a similar trend to that of infectious diseases only in Amsterdam (Figure 4). Yet, this alignment was with airborne infectious diseases, not with what would be expected if convulsions resembled water- and foodborne diseases. While in Maastricht and Rostock, there appeared to be a trade-off between convulsions and water- and foodborne infectious diseases (see Figure 3); the seasonality analysis over the entire period did not support this, as shown in Figure 4. On the other hand, in Hermoupolis (Figure 4), convulsions exhibited a clear summer peak, similar to that of water- and foodborne diseases.
However, since the potential trade-offs in convulsions and water- and foodborne infectious diseases were time-specific, seasonality patterns over shorter periods may show more similarities. Indeed, the seasonal patterns changed over time. Figure 5 divides the total observation period into five subperiods that can be distinguished by seasonal patterns and have a sufficient number of convulsions-related deaths, with orange lines referring to the early nineteenth century, blue lines for the rest of the century, and green lines for the twentieth century. For Hermoupolis, we used only two study periods due to the low number of deaths caused by convulsions. Figure 5 reveals that in all four cities, the trend of convulsions-related mortality was observed to become less significant in the summer months and more significant in the winter months over the course of the study period, albeit at different levels. While Maastricht showed a summer peak in the nineteenth century, particularly between 1864 and 1879, convulsions-related mortality became more and more concentrated in the winter during the first half of the twentieth century. Rostock showed summer peaks throughout the nineteenth century, albeit to a decreasing extent as well. In Hermoupolis, convulsions-related mortality was highest between May and July, whereas in Amsterdam, it showed no summer peak at all for any of the observation periods but became more and more concentrated in the winter. The results of the seasonal patterns broken down in periods suggested that the convulsions-related mortality might have represented deaths from water- and foodborne infectious diseases in some specific localities and periods. As registration practices of illnesses and causes of death became more professionalised, the use of convulsions as the cause of death diminished.
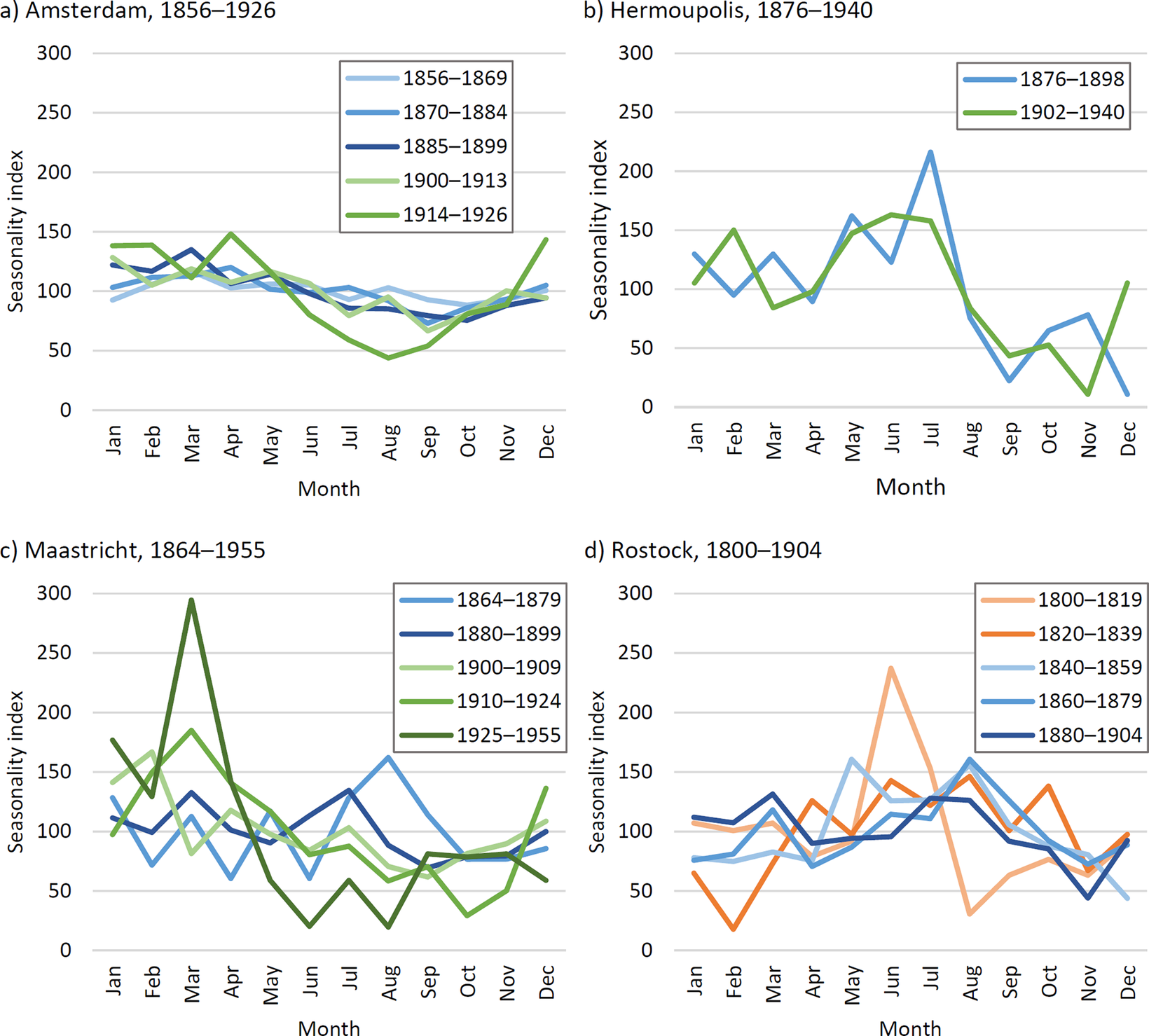
Figure 5. Seasonality ratios for postneonatal convulsions mortality by period in Amsterdam, Hermoupolis, Maastricht, and Rostock.Footnote 82
Furthermore, we explored the relationship between sex and infant deaths from convulsions to determine if any sex differences in the prevalence of convulsions mortality might offer clues to sex-specific under-registration or underlying illnesses. Since the sex pattern of convulsions-related mortality during infancy closely resembled that of all-cause mortality, we presented these results as a supplement (Figure 6). As is shown in Figure 6, boys exhibited slightly higher rates than girls. However, these patterns did not provide additional insights that may help us to understand convulsions-related mortality, as it is well established that boys, in general, have higher mortality rates during infancy.Footnote 83
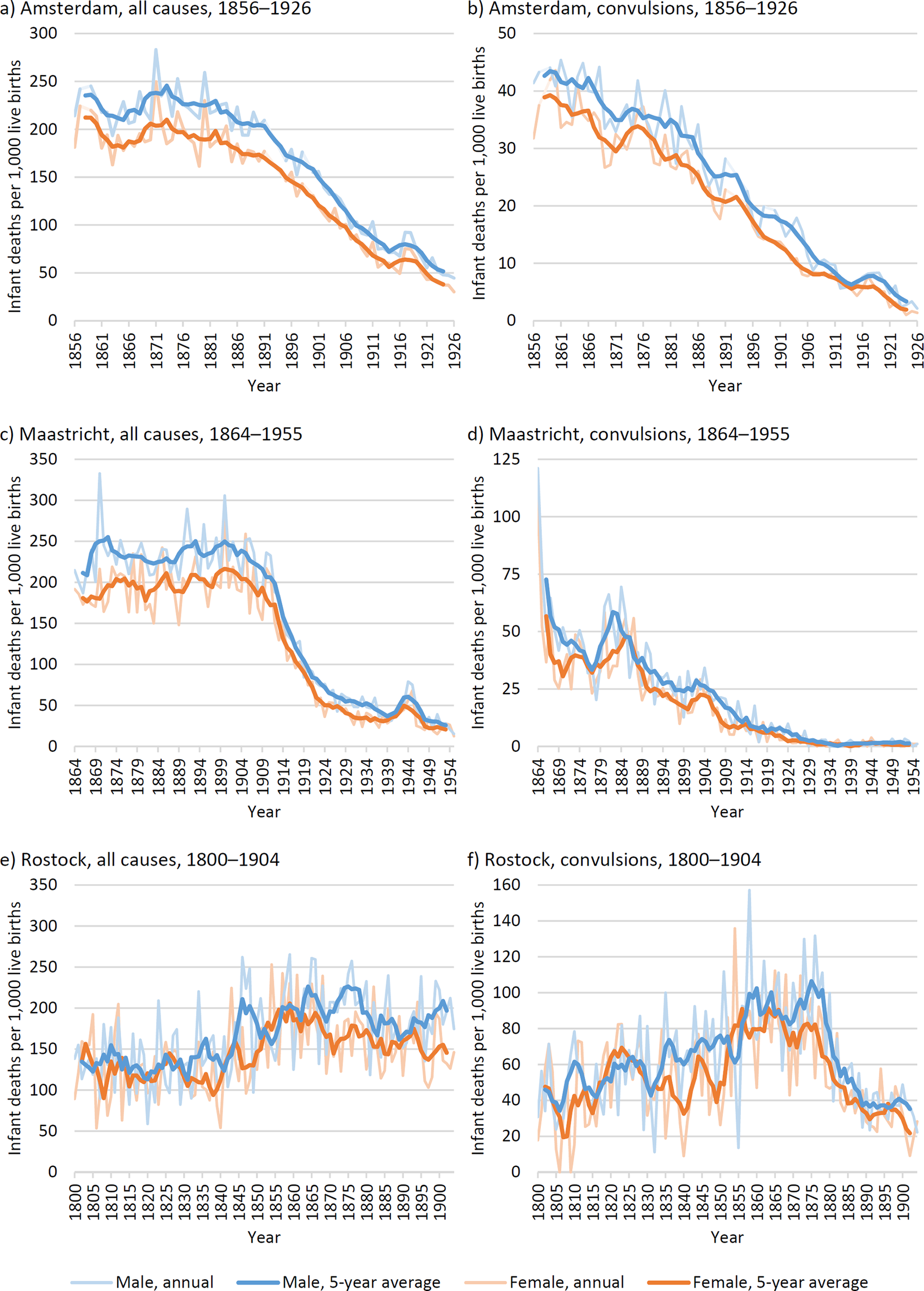
Figure 6. Infant mortality rates by sex for all causes combined (left panel graphs a, c, e) and convulsions (right panel graphs b, d, f) in Amsterdam, Maastricht and, Rostock.
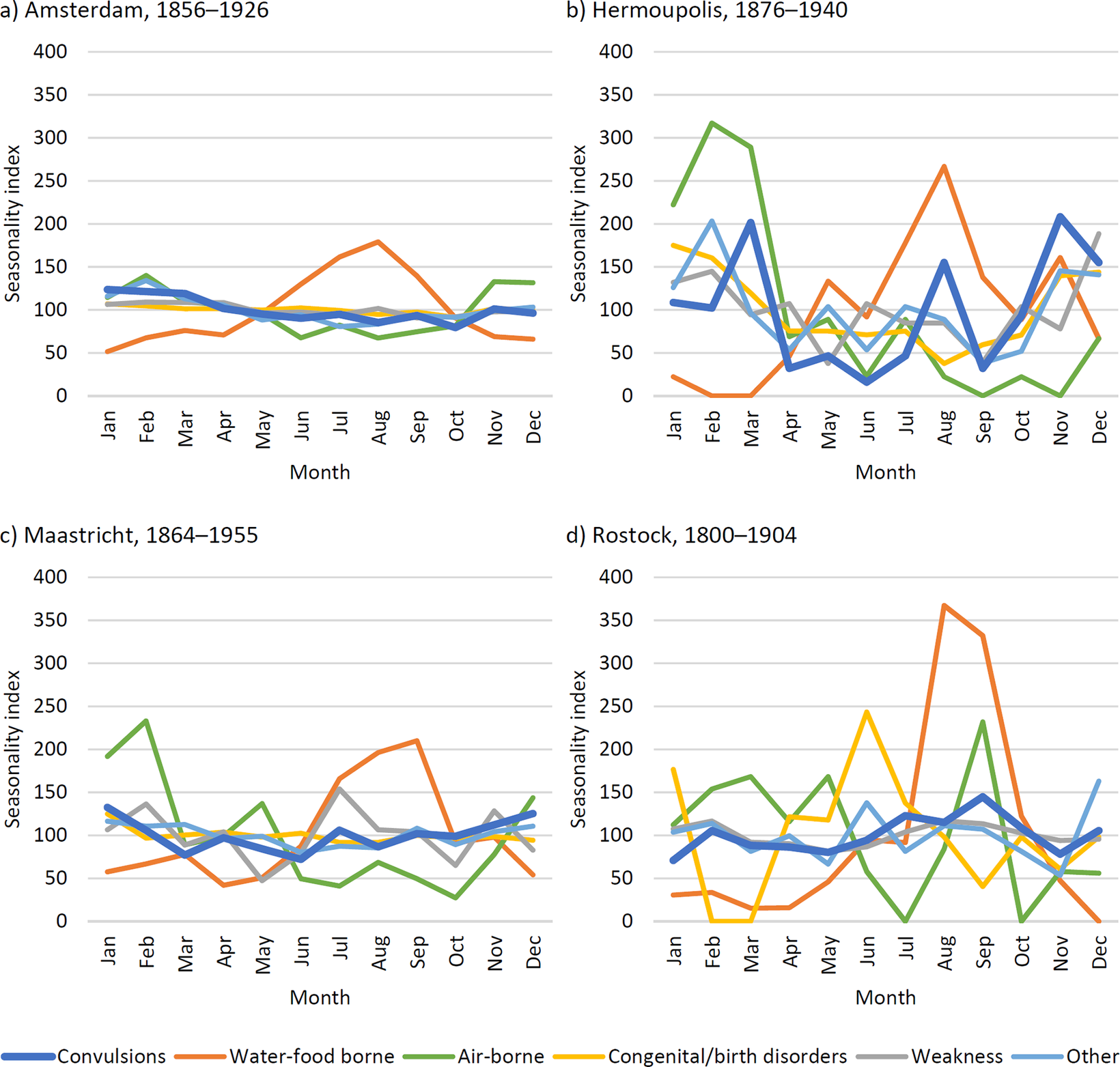
Figure 7. Cause-specific seasonality ratios for neonatal deaths in Amsterdam, Hermoupolis, Maastricht, and Rostock.
Conclusions
The complexity of the term convulsions as a cause of death is widely acknowledged among historians and historical demographers, though the ways in which it is addressed vary significantly. For many scholars, the term convulsions is seen as little more than a nuisance – a vague nineteenth-century term that resists modern classification into a precise cause-of-death category. In the field of historical demography, convulsions are frequently reclassified into the most likely disease category, water- and foodborne infectious diseases, or simply relegated to an ill-defined group and largely ignored. In this study, we argue that both approaches are overly simplistic and risk introducing biases into the datasets used. Moreover, the term itself can offer much more than just a source of frustration. From a qualitative, medical-historical perspective, the term offers valuable insights into historical medical practices and the evolution of diagnostic methods, especially as these practices shifted over time. In this study, we examine convulsions as a cause of death both quantitatively across four European cities (Amsterdam, Hermoupolis, Maastricht, and Rostock) and qualitatively using historical medical literature from Germany, Greece, and the Netherlands. Our goal is to enhance the understanding of this ambiguous cause of death, which can not only reduce biases in quantitative studies but also deepen our knowledge of historical medical diagnostic practices.
The main findings of this study highlight the complex and multifaceted nature of convulsions as a cause of infant death, as revealed through both qualitative and quantitative analyses. Infant deaths attributed to convulsions cannot be adequately classified under a single cause-of-death category; instead, they reflect a range of underlying conditions that vary across the four urban populations. Both historical medical literature and cause-of-death analysis point to a relationship between infantile convulsions and both infectious and non-infectious diseases, particularly airborne as well as water- and foodborne infectious diseases. However, the medical literature indicates that a wide array of diseases could manifest as convulsions that did not always lead to death. Contemporary physicians considered convulsions as a result of disorders and illnesses in the brain or spinal cord, such as encephalitis and meningitis, the most dangerous. Also, convulsions resulting from tetany or spasmophilia, hyperthermia, whooping cough, and hereditary syphilis were viewed as hazardous. It is perhaps unsurprising that, before more standardized diagnostic and/or registration instructions were introduced, convulsions was a commonly used term. Our analysis further supports the idea that convulsions were not solely or even predominantly a stand-in for water- and foodborne infectious diseases, as some historians and historical demographers have claimed. While certain cases of convulsions were likely linked to water- and foodborne infectious diseases, as suggested by both time series analyses of cause-specific mortality and seasonal patterns, other causes of death – such as airborne infectious diseases, and congenital- and birth disorders – may also have been hidden behind the label of convulsions.
The diagnostic practices surrounding convulsions varied significantly by population, across time, and age group within the first year of life. We support the strand of literature that distinguishes convulsions in the first month of life from those in the remaining months of the first year. Convulsions in the first month most likely served as a substitute for congenital and birth-related disorders (Amsterdam, Maastricht, and Rostock), much like weakness.Footnote 84 Over time, diagnostic practices underwent substantial changes, as medical literature reveals. Earlier associations with convulsions were discarded while new ones emerged. Although no clear trend can be pinpointed regarding which causes were linked to convulsions by physicians over time, the medical understanding certainly changed over several decades.
Seasonality analysis offers further insights, showing that, in at least two locations, Rostock and Maastricht, convulsions were associated with a summer peak in mortality during certain periods, especially between 1860 and 1879 in Maastricht and in the period 1800 – 1879 in Rostock. This suggests that a larger proportion of convulsion-related deaths were linked to water- and foodborne infections in these periods, which were exacerbated by high temperatures. However, these seasonal patterns diminished over time. This coincided with improved registration practices, particularly in Maastricht, when stricter legal requirements were introduced in the Netherlands. In the other periods and in Amsterdam and Hermoupolis as a whole, seasonality analysis indicated that convulsions may have been perceived differently, especially where a more pronounced winter peak was observed. For instance, convulsions in Amsterdam exhibited seasonality similar to that of airborne infectious diseases from the 1870s onward, while in Hermoupolis, no clear seasonal pattern was found.
The comparative and longitudinal approach of this study emphasizes the significant diversity in the diagnosis and understanding of infantile convulsions. While the medical handbooks and literature across the three countries were largely rooted in the same medical tradition, local practices varied considerably. In this context, regional medical culture may have proven more important in shaping the use of the term convulsions than formal medical training alone. These regional differences were not limited by national borders but could also be observed within the same country, as demonstrated by the variation between the Dutch cities Amsterdam and Maastricht. Therefore, it is crucial to consider local medical practices when examining historical medical diagnoses.
The importance of these findings lies in the high incidence of mortality attributed to infantile convulsions. This is particularly critical in cities where this term was used extensively to describe a cause of death, as shown in the case of Rostock, where almost half of infant deaths were attributed to convulsions for most of the study period. Our analysis shows that a decline in infantile convulsions-related mortality did not coincide with a reduction in overall infant mortality, indicating that the reasons for a decline in convulsions mortality were different from the reasons for the actual decline in infant mortality. Consequently, high levels of convulsions-related mortality lead to an underestimation of deaths due to other causes of death since some of these deaths may have ended up being registered as only convulsions. Simply categorizing convulsions-related deaths into an ill-defined category is inadequate, as it can distort the classification of an entire dataset by over- or under-estimating mortality due to other disease categories. Moreover, the causes of death hidden by the term convulsions can differ over time in relation to changing registration practices. For this reason, historians studying cause-specific infant mortality should not rely solely on quantitative evidence but must also consider how registration practices may have evolved. Incorporating this contextual knowledge into their analysis is essential for accurately interpreting mortality trends.
The high incidence of infant deaths attributed to convulsions serves as a valuable indicator for assessing the accuracy of cause-of-death registration, similar to other ill-defined causes of death, such as weakness. The reduction or eventual disappearance of infant deaths classified under convulsions or other unspecified causes over time likely reflects improvements in both registration practices and medical understanding. Finally, we suggest that further research into patterns of infant mortality from convulsions in rural areas is necessary. While the cities in our study are quite diverse, they were relatively large cities by the standards of each country at the time, implying that our findings primarily reflect urban patterns. These urban patterns may have differed significantly from those in rural areas, where medical resources and practices were likely more limited.
Supplementary material
The supplementary material for this article can be found at http://doi.org/10.1017/mdh.2025.7.
Competing interests
The authors declare none.










