Refine listing
Actions for selected content:
1416829 results in Open Access
Insight into impaired social functioning in dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 19-20
-
- Article
-
- You have access
- Export citation
Rooted in turbulence: arguing ethnicity in folk narratives about violence
-
- Journal:
- International Journal of Asian Studies , First View
- Published online by Cambridge University Press:
- 02 February 2024, pp. 1-13
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
P5: Anesthesia Nurses’ Self-Perceived Roles and Competences and Their Recognition of Anesthesia Specialist Nurses' Roles and Competencies
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 232
-
- Article
-
- You have access
- Export citation
FC32: Neuropsychiatric symptoms: Disentangling the role of unmet needs using the Camberwell Assessment of Need for the Elderly (CANE) interview
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 95
-
- Article
-
- You have access
- Export citation
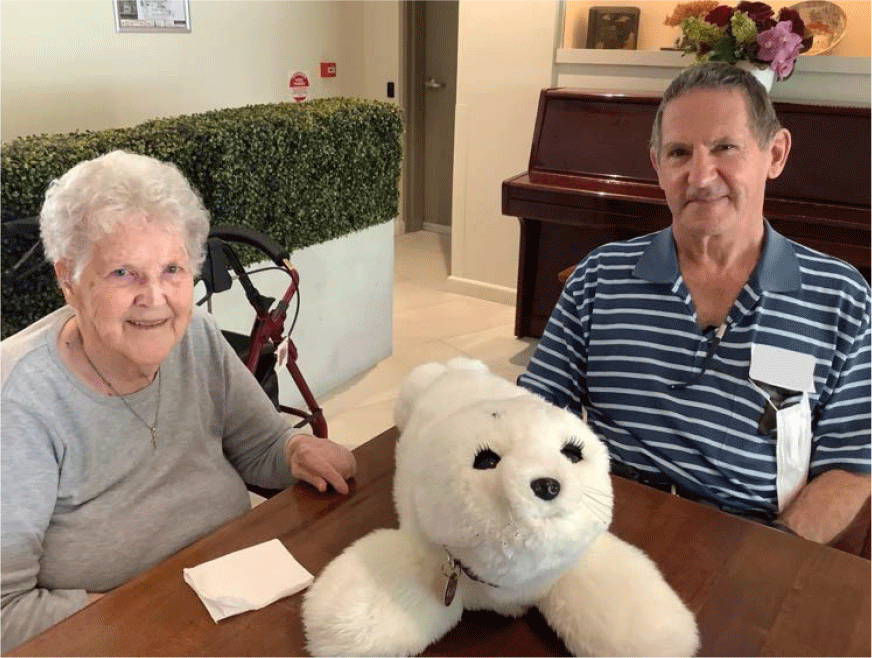
P114: Experiences of nursing home residents with dementia and chronic pain using an interactive social robot: A qualitative study of multiple stakeholders
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 171-172
-
- Article
-
- You have access
- Export citation
P142: Dementia diagnosis: the potential onset of suicidal risk
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 179
-
- Article
-
- You have access
- Export citation
Plenary Session 5: The role of social connectedness in the multifactorial demential syndrome. Does social life matter? - IPA/INTERDEM live webinar
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 14
-
- Article
-
- You have access
- Export citation
P101: Factors Assoicated with Psychotropic Use in People with Dementia Living in Their Own Homes in the Community: A Systimatic Review and Meta-Analysis
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 250
-
- Article
-
- You have access
- Export citation
P172: A preliminary study for potential protective role of anti-oxidative stress markers for cognitive impairment: glutathione and glutathione reductase.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 184
-
- Article
-
- You have access
- Export citation
Using the axonal protein neurofilament light to distinguish psychiatric and neurodegenerative disorders across a program of clinical research studies
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 7-8
-
- Article
-
- You have access
- Export citation
P36: Intimacy and Sexuality Expression Preference (ISEP) Tool: Usage experience and creation of a practical user guide
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 200
-
- Article
-
- You have access
- Export citation
Pattern of anuran infection by acanthocephalans from the Cerrado, Northeastern Brazil with a summary for South America
-
- Journal:
- Journal of Helminthology / Volume 98 / 2024
- Published online by Cambridge University Press:
- 02 February 2024, e15
-
- Article
- Export citation
FC42: Evaluation of patients with cognitive impairment due to suspected idiopathic normal-pressure hydrocephalus at medical centers for dementia: a nationwide hospital-based survey in Japan
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 104
-
- Article
-
- You have access
- Export citation
The implementation of euthanasia in Spain: a one-year balance and current challenges
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 54
-
- Article
-
- You have access
- Export citation
P164: Reminiscence therapy to reduce falls and weight loss: The protocol and outcomes of a pilot trial in residential aged care.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 183
-
- Article
-
- You have access
- Export citation
FC33: Hilarious Gas for treatment resistant depression in older adults: is it really serious?
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 96-97
-
- Article
-
- You have access
- Export citation
Protective and Vulnerability Factors of Posttraumatic Growth in Older Adults during the COVID-19 Pandemic
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 23
-
- Article
-
- You have access
- Export citation
S22: Social Connectedness, Ageing and Mental Health in Doctors
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 64
-
- Article
-
- You have access
- Export citation
S1: Social health in the context of dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 14-15
-
- Article
-
- You have access
- Export citation
P93: Characteristics of complex, non-pharmacological cognitive stimulation interventions for people with dementia in nursing homes: systematic review
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 124
-
- Article
-
- You have access
- Export citation