Refine listing
Actions for selected content:
1416829 results in Open Access
Visualization of Pain and Agitation by System Analysis Algorithms
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 38-39
-
- Article
-
- You have access
- Export citation
P107: Paranoid Ideation Without Psychosis Is Associated With Depression, Anxiety, and Suicide Attempts in General Population
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 169
-
- Article
-
- You have access
- Export citation
FC3: “Empowering Health & Social Service Providers in Addressing Social Isolation & Loneliness in Older Adults”
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 66
-
- Article
-
- You have access
- Export citation
P19: Effects of a Post-diagnostic Support Programme on self-efficacy among persons with dementia and family members
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 194-195
-
- Article
-
- You have access
- Export citation
P195: The evolution of a community mental health team in Singapore: Community Psychogeriatric Programme
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 228
-
- Article
-
- You have access
- Export citation
P72: Diagnostic pathways for people living with rare types of dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 245
-
- Article
-
- You have access
- Export citation
P100: Education level is associated with neuropsychiatric symptoms in patients with amnestic-mild cognitive impairment
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 211
-
- Article
-
- You have access
- Export citation
P94: Co-design of a theory-based implementation plan for a digital holistic assessment and decision support framework for people with dementia in care homes
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 167
-
- Article
-
- You have access
- Export citation
P59: Associations Between Smoking, Alcohol Consumption, Physical Activity and Depression in Middle-Aged Premenopausal and Postmenopausal Women
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 156-157
-
- Article
-
- You have access
- Export citation
Evaluation of the Situations of Coping With Mental Trauma and Trauma in Emergency Service Personnel Who Medically Intervened to Earthquake Affected People in the 2020 Izmir Earthquake
-
- Journal:
- Disaster Medicine and Public Health Preparedness / Volume 18 / 2024
- Published online by Cambridge University Press:
- 02 February 2024, e17
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
FC10: Telehealth for Older Adults: Developing telehealth competencies to ensure access, quality and equity across the lifespan
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 72-73
-
- Article
-
- You have access
- Export citation
Transnational Echoes of Spenceanism: A Text-Mining Exploration in English-Language Newspapers (1790–1850)
-
- Journal:
- International Review of Social History / Volume 69 / Issue 1 / April 2024
- Published online by Cambridge University Press:
- 02 February 2024, pp. 67-97
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
P118: The Geriatric Psychiatry Fellowship Program in Mexico
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 172
-
- Article
-
- You have access
- Export citation
FC39: The influence of social constructivism on children and young adults perspectives of parental young onset dementia: A thematic analysis of the narratives
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 101-102
-
- Article
-
- You have access
- Export citation
P160: Electroconvulsive therapy for neuropsychiatric symptoms in dementia: survey among Dutch physicians
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 257-258
-
- Article
-
- You have access
- Export citation
FC22: Changes in inhibitory control in older adults: Diminished inhibitory efficiency or slowing of general processing speed?
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 83-84
-
- Article
-
- You have access
- Export citation
FC26: What have staff got to do with it? Untangling complex relationships between residential aged care staff, the quality of care they provide, and the quality of life of people with dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 87-88
-
- Article
-
- You have access
- Export citation
Plenary Session 1 : Healthy Ageing and the role of physical and social environments
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 13
-
- Article
-
- You have access
- Export citation
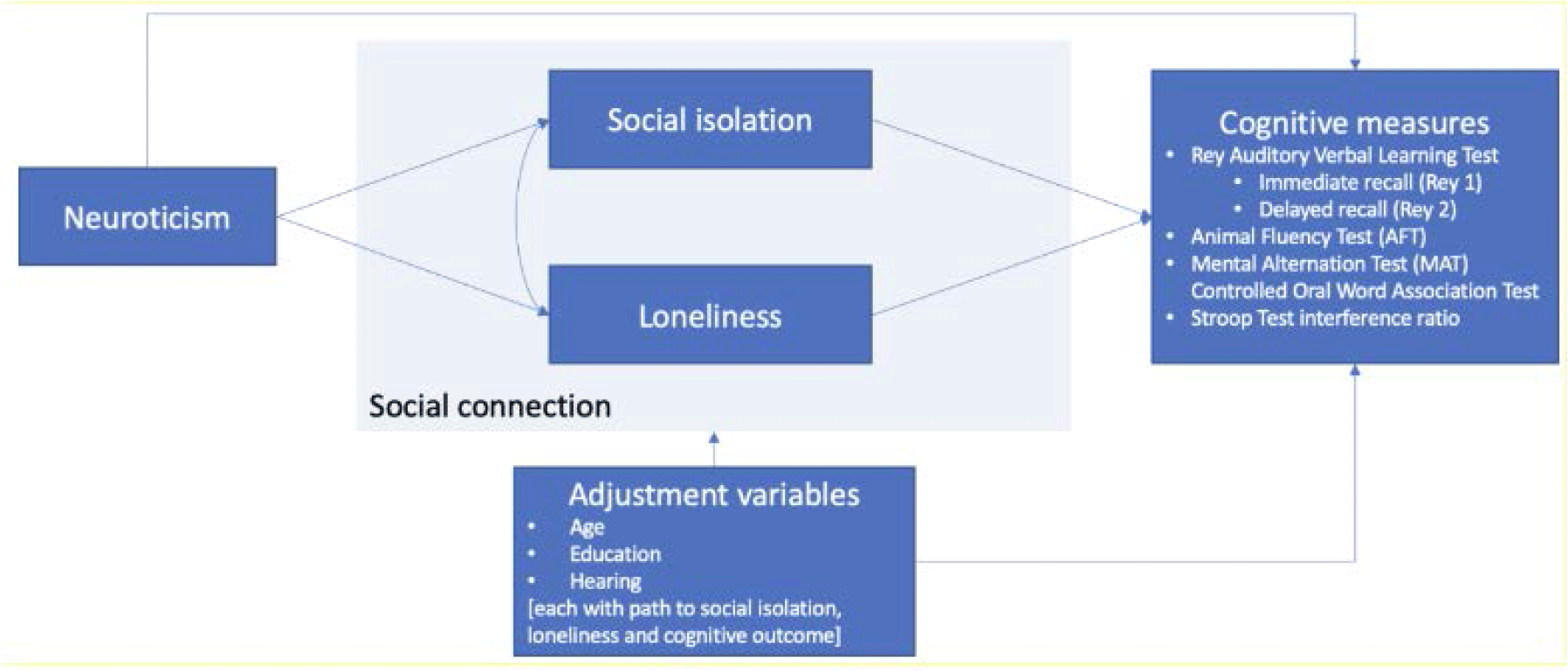
FC30: The relationships between neuroticism, social connection and cognition
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 92-94
-
- Article
-
- You have access
- Export citation
iSupport: the online support program for caregivers of people with dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 32
-
- Article
-
- You have access
- Export citation