Refine listing
Actions for selected content:
1416829 results in Open Access
P169: IMPROVING THE MENTAL HEALTH CARE NEEDS OF OLDER ADULTS IN NEPAL.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 142
-
- Article
-
- You have access
- Export citation
Cross-sector learning collaboratives can improve post-diagnosis care integration for people with young onset dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 8-9
-
- Article
-
- You have access
- Export citation
P57: The ENGAGED study: dementia prevention co-design for people living with depression
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 116-117
-
- Article
-
- You have access
- Export citation
P170: Safety and Tolerability of Brexpiprazole for the Treatment of Agitation in Alzheimer’s Dementia: Pooled Results From Three Phase III Trials
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 259-260
-
- Article
-
- You have access
- Export citation
FC16: Memory Services National Accreditation Programme (MSNAP), United Kingdom The Royal College of Psychiatrists, UK
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 78-79
-
- Article
-
- You have access
- Export citation
P103: Middle Cerebral Artery Stenosis is Associated with Severity of Depression in Elderly Patients: Magnetic Resonance Angiography (MRA) Findings
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 168-169
-
- Article
-
- You have access
- Export citation
FC23: Dementia and Triadic (Doctor-Patient-Carer) Interactions in Primary Care
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 84-85
-
- Article
-
- You have access
- Export citation
FC18: Can rehabilitation improve functional independence of older people with dementia? A pragmatic randomized controlled trial (RCT) of the Interdisciplinary Home-bAsed Reablement Program (I-HARP)
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 80-81
-
- Article
-
- You have access
- Export citation
Blended web-based Acceptance and Commitment Therapy for Informal Caregivers of people with dementia (ACT-IC study): Result of social health aspects
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 4
-
- Article
-
- You have access
- Export citation
Social connections and risk of incident mild cognitive impairment, dementia, and mortality in 13 longitudinal cohort studies of ageing
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 16-17
-
- Article
-
- You have access
- Export citation
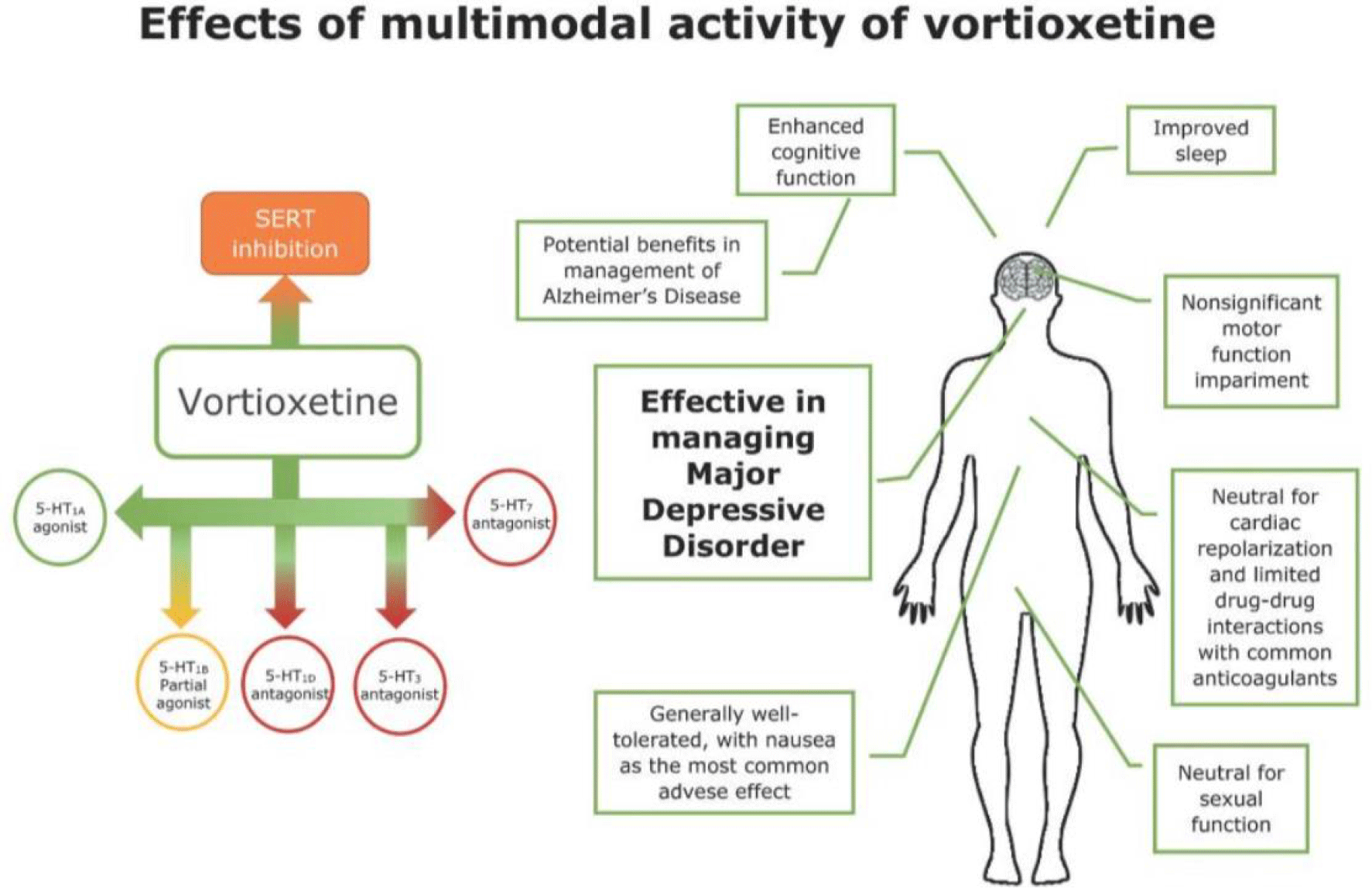
P149: Chronic fatigue syndrome and its response to the use of a multimodal antidepressant
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 216-217
-
- Article
-
- You have access
- Export citation
Descriptive anatomy and three-dimensional reconstruction of the skull of the tetrapod Eoherpeton watsoni Panchen, 1975 from the Carboniferous of Scotland
-
- Journal:
- Earth and Environmental Science Transactions of The Royal Society of Edinburgh , First View
- Published online by Cambridge University Press:
- 02 February 2024, pp. 1-21
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Virtual reality to provide caregiver skill development and problem solving
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 42-43
-
- Article
-
- You have access
- Export citation
Cost-effectiveness of a tablet-based intervention to support social health in dementia: results from the FindMyApps randomized controlled trial
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 3
-
- Article
-
- You have access
- Export citation
FC37: Prevalence of depressive symptoms and its association with probable sarcopenia, disability, frailty and comorbidities among older adults.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 100
-
- Article
-
- You have access
- Export citation
P92: Risk Assessment in People living with Dementia: A Systematic Review
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 208
-
- Article
-
- You have access
- Export citation
Collective learning as means to improve quality of long-term care
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 55-56
-
- Article
-
- You have access
- Export citation
P153: The CIMA-Q and CompAS cohort studies on factors associated with Alzheimer's disease (AD): Exploring sociodemographic, health and neuropsychological profile of Subjective Cognitive Decline (SCD) participants from two culturally differentiated samples.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 269-272
-
- Article
-
- You have access
- Export citation
P13: Supporting physical health for mental health consumers, in a community setting
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 193-194
-
- Article
-
- You have access
- Export citation
Digital technologies in ISupport implementation in Russia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 59-60
-
- Article
-
- You have access
- Export citation