Refine listing
Actions for selected content:
1418337 results in Open Access
P16: Report on a Dementia Prevention Workshop Organized through Multidiscipline Intervention: An Examination of Intervention Approach through the Evaluation of Group Reminiscence Method and Mental Aspect
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 194
-
- Article
-
- You have access
- Export citation
Indigenous Knowledge and Ontological Difference? Ontological Pluralism, Secular Public Reason, and Knowledge between Indigenous Amazonia and the West
-
- Journal:
- Comparative Studies in Society and History / Volume 66 / Issue 2 / April 2024
- Published online by Cambridge University Press:
- 02 February 2024, pp. 267-293
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
P104: Heterogeneity of Response to methylphenidate in apathetic patients in the ADMET 2 Trial
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 125-126
-
- Article
-
- You have access
- Export citation
P116: Cessation of caregiving due to institutionalization: Dementia family caregivers’ profile. A 3 year longitudinal study
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 131-132
-
- Article
-
- You have access
- Export citation
P194: A comparison study between AD8 and modified AD8 for dementia screening
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 264-265
-
- Article
-
- You have access
- Export citation
P29: Prolonged Intermittent Theta-Burst Stimulation of the Left Dorsolateral Prefrontal Cortex for Older Adults with Treatment-Resistant Depression: Effectiveness and Safety
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 111-112
-
- Article
-
- You have access
- Export citation
P1: Dosing and treatment outcomes of rTMS for treatment-resistant depressed older adults in a naturalistic outpatient clinic population.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 191-192
-
- Article
-
- You have access
- Export citation
P207: Pilot testing of the Health and Social Care Professionals’ Knowledge & Attitudes towards Later Life Sexuality (HSCP-KALLS) instrument
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 148
-
- Article
-
- You have access
- Export citation
P24: DemenTitude® - Applying the Model of “LAN” to Understand the Experience of People with Dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 151
-
- Article
-
- You have access
- Export citation
Insight into impaired social functioning in dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 19-20
-
- Article
-
- You have access
- Export citation
Rooted in turbulence: arguing ethnicity in folk narratives about violence
-
- Journal:
- International Journal of Asian Studies , First View
- Published online by Cambridge University Press:
- 02 February 2024, pp. 1-13
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
P5: Anesthesia Nurses’ Self-Perceived Roles and Competences and Their Recognition of Anesthesia Specialist Nurses' Roles and Competencies
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 232
-
- Article
-
- You have access
- Export citation
FC32: Neuropsychiatric symptoms: Disentangling the role of unmet needs using the Camberwell Assessment of Need for the Elderly (CANE) interview
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 95
-
- Article
-
- You have access
- Export citation
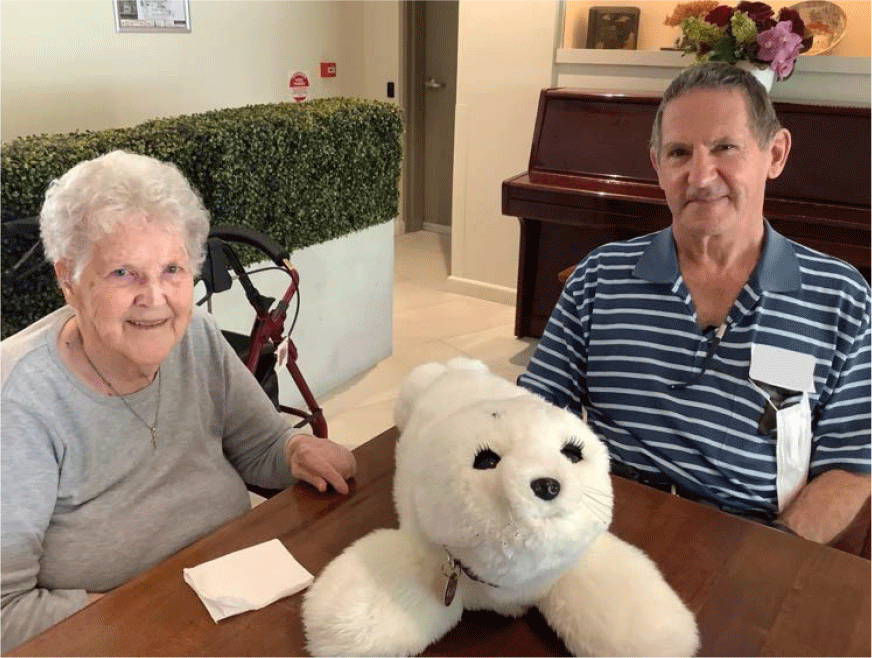
P114: Experiences of nursing home residents with dementia and chronic pain using an interactive social robot: A qualitative study of multiple stakeholders
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 171-172
-
- Article
-
- You have access
- Export citation
P142: Dementia diagnosis: the potential onset of suicidal risk
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 179
-
- Article
-
- You have access
- Export citation
Plenary Session 5: The role of social connectedness in the multifactorial demential syndrome. Does social life matter? - IPA/INTERDEM live webinar
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 14
-
- Article
-
- You have access
- Export citation
P101: Factors Assoicated with Psychotropic Use in People with Dementia Living in Their Own Homes in the Community: A Systimatic Review and Meta-Analysis
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 250
-
- Article
-
- You have access
- Export citation
P172: A preliminary study for potential protective role of anti-oxidative stress markers for cognitive impairment: glutathione and glutathione reductase.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 184
-
- Article
-
- You have access
- Export citation
Using the axonal protein neurofilament light to distinguish psychiatric and neurodegenerative disorders across a program of clinical research studies
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 7-8
-
- Article
-
- You have access
- Export citation
P36: Intimacy and Sexuality Expression Preference (ISEP) Tool: Usage experience and creation of a practical user guide
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 200
-
- Article
-
- You have access
- Export citation