Refine listing
Actions for selected content:
1418155 results in Open Access
The association between dietary patterns and disease severity in patients with ulcerative colitis
-
- Journal:
- British Journal of Nutrition / Volume 131 / Issue 10 / 28 May 2024
- Published online by Cambridge University Press:
- 02 February 2024, pp. 1803-1812
- Print publication:
- 28 May 2024
-
- Article
-
- You have access
- HTML
- Export citation
P201: Effect of Virtual Reality-based Biofeedback in Highly Stressed People
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 147
-
- Article
-
- You have access
- Export citation
P37: A systematic review on inequalities in accessing and using social care in dementia – from pre- and pandemic times to moving beyond
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 238-239
-
- Article
-
- You have access
- Export citation
Digital Phenotyping of Behavior and Clinical Decision Making in Psychogeriatrics: Towards Precision Care
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 36-37
-
- Article
-
- You have access
- Export citation
P208: The activities of Initial- phase Intensive Support Team for Dementia (IPIST) in Japan
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 148-149
-
- Article
-
- You have access
- Export citation
Mild behavioral impairment in prodromal Alzheimer´s disease and its association with APOE and BDNF risk genetic polymorphisms
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 26-27
-
- Article
-
- You have access
- Export citation
P110: Development and validation of the Relationship Quality Scales in Caregiving (RQSC): preliminary results.
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 128-129
-
- Article
-
- You have access
- Export citation
Determinants of Psychosocial Health Status in Pregnant and Postpartum Women Experiencing Earthquake in Turkey
-
- Journal:
- Disaster Medicine and Public Health Preparedness / Volume 18 / 2024
- Published online by Cambridge University Press:
- 02 February 2024, e16
-
- Article
- Export citation
P27: Pilot study of telephone peer support for inclusion of people living with cognitive decline in urban areas
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 197-198
-
- Article
-
- You have access
- Export citation
P41: Valladolid Multicenter Study: Factors related to time to referral and length of hospital stay in old psychiatry patients in seven general hospitals in Spain
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 201
-
- Article
-
- You have access
- Export citation
Optimal insurance with counterparty and additive background risk
-
- Journal:
- ASTIN Bulletin: The Journal of the IAA / Volume 54 / Issue 2 / May 2024
- Published online by Cambridge University Press:
- 02 February 2024, pp. 441-462
- Print publication:
- May 2024
-
- Article
- Export citation
FC15: The Baycrest Quick-Response Caregiver Tool TM for Behavioral and Psychological Symptoms of Dementia: Background and mixed methods studies
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 77-78
-
- Article
-
- You have access
- Export citation
Workshop 2: Humanitarian Crisis and Old Age Mental Health
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 1-2
-
- Article
-
- You have access
- Export citation
P12: Living Lab as academic practice partnership to improve care for people with dementia
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 234-235
-
- Article
-
- You have access
- Export citation
FC41: Music-assisted reminiscence therapy: Feasibility and use in practice
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 103-104
-
- Article
-
- You have access
- Export citation
P105: Measuring clinically relevant change in apathy symptoms in ADMET 2
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 126-127
-
- Article
-
- You have access
- Export citation
S20: Adapting and implementing WHO iSupport among dementia caregivers worldwide: users' perspectives and future development (Session II)
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 57-58
-
- Article
-
- You have access
- Export citation
P47: Impact of the FindMyApps intervention on Social health in community-dwelling people with dementia: results from a randomized controlled trial
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, pp. 113-114
-
- Article
-
- You have access
- Export citation
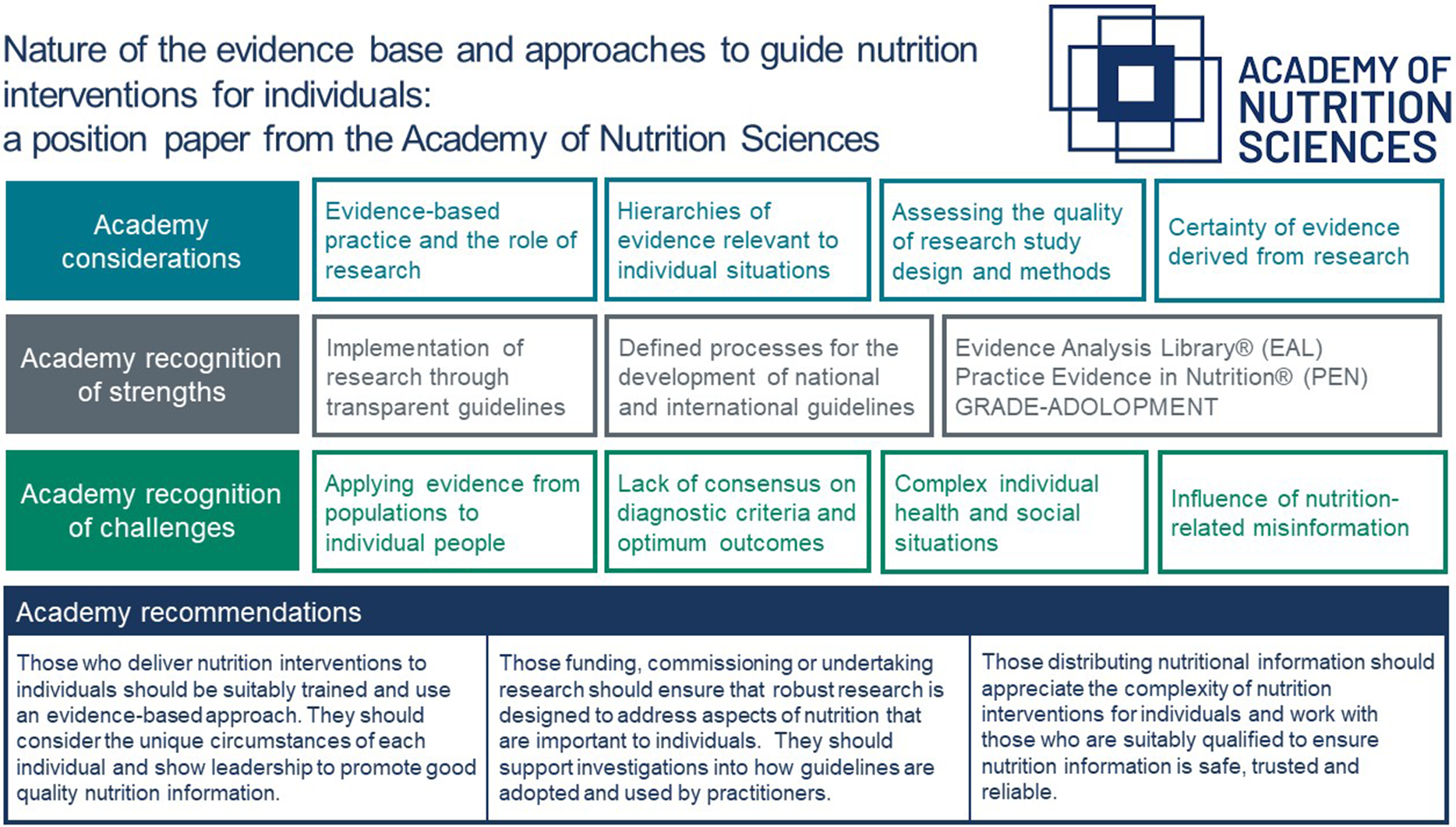
Nature of the evidence base and approaches to guide nutrition interventions for individuals: a position paper from the Academy of Nutrition Sciences
-
- Journal:
- British Journal of Nutrition / Volume 131 / Issue 10 / 28 May 2024
- Published online by Cambridge University Press:
- 02 February 2024, pp. 1754-1773
- Print publication:
- 28 May 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
P6: Brain alterations in patients with late-life major depressive disorder and amnestic type mild cognitive impairment during oddball performance: a longitudinal study
-
- Journal:
- International Psychogeriatrics / Volume 35 / Issue S1 / December 2023
- Published online by Cambridge University Press:
- 02 February 2024, p. 232
-
- Article
-
- You have access
- Export citation