Refine listing
Actions for selected content:
FirstView articles
Contents
Review Article
A call for phylogenetic context to understand geographic variation and host specificity in the parasitic copepod genus Salmincola
-
- Published online by Cambridge University Press:
- 06 October 2025, pp. 1-13
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Research Article
A combined morphological and genetic survey of helminths in the European green toad Bufotes viridis (Laurenti, 1768) from eastern Slovakia
-
- Published online by Cambridge University Press:
- 06 October 2025, pp. 1-17
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Descriptions of intestinal worms in European medieval medical texts
-
- Published online by Cambridge University Press:
- 26 September 2025, pp. 1-4
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Review Article
Mainstreaming female genital schistosomiasis to ensure it is not neglected among the neglected tropical diseases
-
- Published online by Cambridge University Press:
- 25 September 2025, pp. 1-9
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Research Article
Uncinaria stenocephala (northern hookworm) is the major endoparasite in dogs from private dog shelters in the Balkans: presence of benzimidazole susceptible isotype-1 β-tubulin alleles
-
- Published online by Cambridge University Press:
- 22 September 2025, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Review Article
Visual diagnostics for female genital schistosomiasis and the opportunity for improvement using computer vision
-
- Published online by Cambridge University Press:
- 12 September 2025, pp. 1-12
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Research Article
An investigation of female genital schistosomiasis and associated genital infections in Southern Malawi
-
- Published online by Cambridge University Press:
- 01 September 2025, pp. 1-12
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Molecular characterization of two Myxidium species (Cnidaria: Bivalvulida: Myxidiidae) infecting barbs in the Sea of Galilee, Israel
-
- Published online by Cambridge University Press:
- 28 August 2025, pp. 1-16
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Proof-of-concept trial in mature bulls prophylactically and therapeutically vaccinated with an experimental whole-cell killed Tritrichomonas foetus vaccine
-
- Published online by Cambridge University Press:
- 22 August 2025, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Review Article
Genital schistosomiasis in non-endemic settings: a clinical perspective
-
- Published online by Cambridge University Press:
- 20 August 2025, pp. 1-6
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Incorporating the gender dimension into infectious disease research: how is Parasitology progressing?
-
- Published online by Cambridge University Press:
- 13 August 2025, pp. 1-7
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Research Article
From clinical research to public health action: addressing chronic female genital schistosomiasis in non-endemic countries
-
- Published online by Cambridge University Press:
- 06 August 2025, pp. 1-9
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Microscopic detection and genetic characterization of schistosome eggs within cervicovaginal lavage sediments from cases of female genital schistosomiasis
-
- Published online by Cambridge University Press:
- 06 August 2025, pp. 1-8
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Book Review
New book on the links between ecology and aquatic parasites - Nico Smit and Bernd Sures (editors): Aquatic Parasitology: Ecological and Environmental Concepts and Implications of Marine and Freshwater (2025) Parasites. Springer Nature, Switzerland. Pp. XI+662. Hardcover ISBN 978-3-031-83902-3; Softcover ISBN 978-3-031-83905-4; eBook ISBN 978-3-031-83903-0 (DOI: https://doi.org/10.1007/978-3-031-83903-0)
-
- Published online by Cambridge University Press:
- 14 July 2025, pp. 1-2
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Review Article
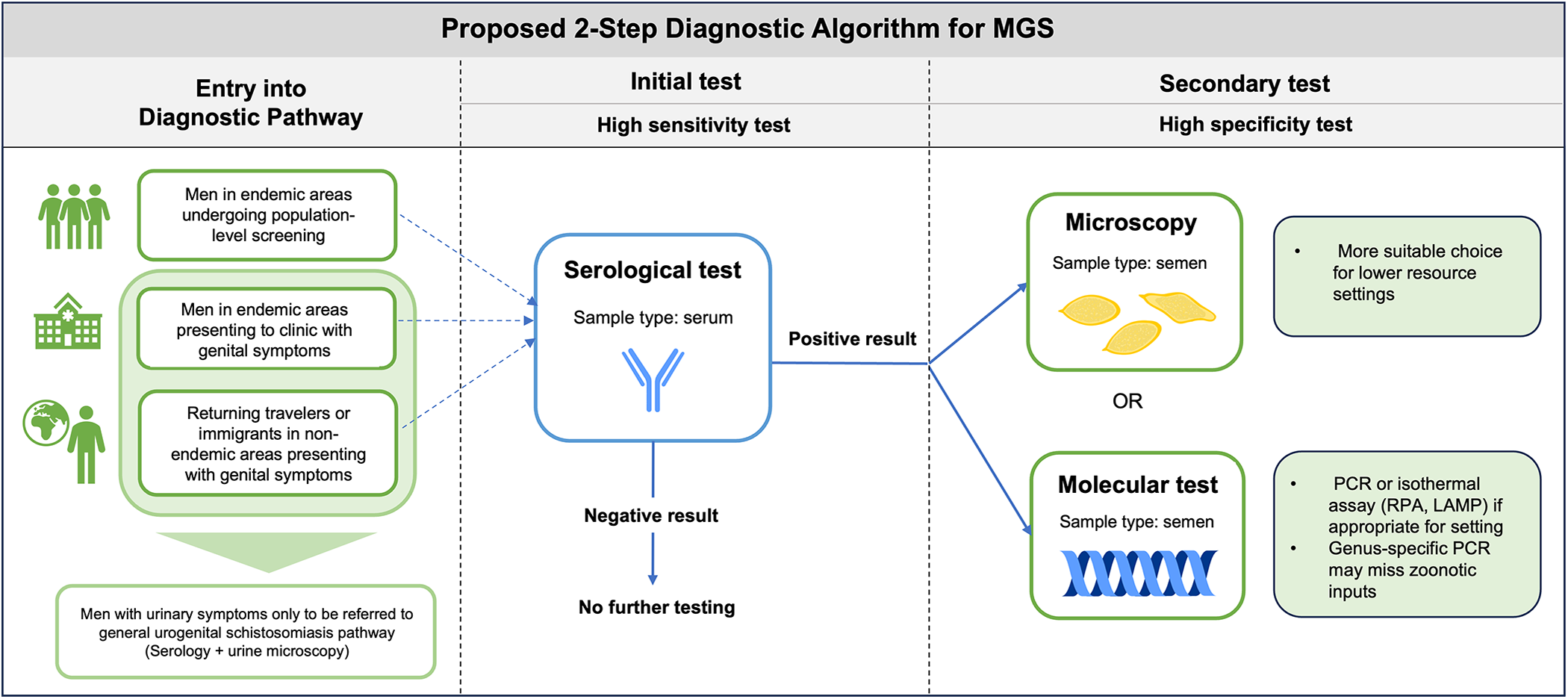
Closing the diagnostic gap in male genital schistosomiasis (MGS): current detection tools and novel strategies
-
- Published online by Cambridge University Press:
- 24 June 2025, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Research Article
‘Female Genital Schistosomiasis: Translational Challenges and Opportunities’ – outputs and actions from a consultative, collaborative and translational workshop
-
- Published online by Cambridge University Press:
- 23 June 2025, pp. 1-11
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Cross-sectional assessment of feasibility and acceptability in screening for female genital schistosomiasis (FGS) in two clinical settings in East Province, Cameroon
-
- Published online by Cambridge University Press:
- 16 June 2025, pp. 1-7
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Review Article
Description of four cases of male genital schistosomiasis (MGS) in children and adolescents, with a scoping review
-
- Published online by Cambridge University Press:
- 24 February 2025, pp. 1-10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation