Refine listing
Actions for selected content:
1418034 results in Open Access
SSH volume 48 issue 1 Cover and Back matter
-
- Journal:
- Social Science History / Volume 48 / Issue 1 / Spring 2024
- Published online by Cambridge University Press:
- 06 March 2024, pp. b1-b2
- Print publication:
- Spring 2024
-
- Article
-
- You have access
- Export citation
JFQ volume 59 issue 1 Cover and Front matter
-
- Journal:
- Journal of Financial and Quantitative Analysis / Volume 59 / Issue 1 / February 2024
- Published online by Cambridge University Press:
- 14 February 2024, pp. f1-f4
- Print publication:
- February 2024
-
- Article
-
- You have access
- Export citation
Orders and Disorders of Marriage, Church, and Empire in Mid-Nineteenth-Century Ottoman Armenia
-
- Journal:
- International Journal of Middle East Studies / Volume 56 / Issue 1 / February 2024
- Published online by Cambridge University Press:
- 14 March 2024, pp. 75-90
- Print publication:
- February 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
David Lehmann, After the Decolonial: Ethnicity, Gender and Social Justice in Latin America Polity, 2022, pp. xiv + 223
-
- Journal:
- Journal of Latin American Studies / Volume 56 / Issue 1 / February 2024
- Published online by Cambridge University Press:
- 12 March 2024, pp. 187-189
- Print publication:
- February 2024
-
- Article
- Export citation
Beckett’s Wasted Breath
-
- Journal:
- New Theatre Quarterly / Volume 40 / Issue 1 / February 2024
- Published online by Cambridge University Press:
- 13 February 2024, pp. 62-75
- Print publication:
- February 2024
-
- Article
-
- You have access
- Open access
- Export citation
SITI Training: Viewpoints and the Suzuki Method for Cross-Cultural Collaboration
-
- Journal:
- New Theatre Quarterly / Volume 40 / Issue 1 / February 2024
- Published online by Cambridge University Press:
- 13 February 2024, pp. 48-61
- Print publication:
- February 2024
-
- Article
- Export citation
POLICIES FOR INCLUSIVE GROWTH
-
- Journal:
- National Institute Economic Review / Volume 267 / Spring 2024
- Published online by Cambridge University Press:
- 29 April 2024, pp. 26-34
- Print publication:
- Spring 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
NMITE AND THE POLITICAL ECONOMY OF HIGHER EDUCATION: 2023 PARLIAMENTARY LECTURE
-
- Journal:
- National Institute Economic Review / Volume 267 / Spring 2024
- Published online by Cambridge University Press:
- 08 April 2025, pp. 66-73
- Print publication:
- Spring 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Effects of horizontal magnetic fields on turbulent Rayleigh–Bénard convection in a cuboid vessel with aspect ratio Γ = 5
-
- Journal:
- Journal of Fluid Mechanics / Volume 980 / 10 February 2024
- Published online by Cambridge University Press:
- 31 January 2024, A24
-
- Article
- Export citation
Mitigating Unemployment Stigma: Racialized Differences in Impression Management among Urban and Suburban Jobseekers
-
- Journal:
- Du Bois Review: Social Science Research on Race / Volume 21 / Issue 2 / Fall 2024
- Published online by Cambridge University Press:
- 31 January 2024, pp. 273-292
-
- Article
- Export citation
Effectiveness and predictors of group cognitive behaviour therapy outcome for generalised anxiety disorder in an out-patient hospital setting
-
- Journal:
- Behavioural and Cognitive Psychotherapy / Volume 52 / Issue 4 / July 2024
- Published online by Cambridge University Press:
- 31 January 2024, pp. 440-455
- Print publication:
- July 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
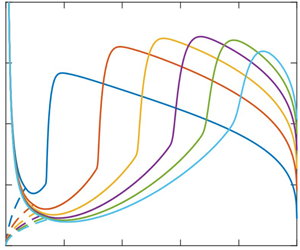
The characteristics of the circular hydraulic jump and vortex structure
-
- Journal:
- Journal of Fluid Mechanics / Volume 980 / 10 February 2024
- Published online by Cambridge University Press:
- 31 January 2024, A15
-
- Article
- Export citation
Travelling Barricades: Transnational Networks, Diffusion and the Dynamics of 1980s Squatter Conflicts in Western Europe – CORRIGENDUM
-
- Journal:
- Contemporary European History / Volume 33 / Issue 2 / May 2024
- Published online by Cambridge University Press:
- 31 January 2024, p. 809
- Print publication:
- May 2024
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Flows with free boundaries and hydrodynamic singularities
-
- Journal:
- Journal of Fluid Mechanics / Volume 980 / 10 February 2024
- Published online by Cambridge University Press:
- 31 January 2024, A23
-
- Article
- Export citation
Arazyme secreted by Serratia proteamaculans: current understanding in animal husbandry – CORRIGENDUM
-
- Journal:
- The Journal of Agricultural Science / Volume 161 / Issue 5 / October 2023
- Published online by Cambridge University Press:
- 31 January 2024, p. 703
-
- Article
-
- You have access
- HTML
- Export citation
Yielding to percolation: a universal scale
-
- Journal:
- Journal of Fluid Mechanics / Volume 980 / 10 February 2024
- Published online by Cambridge University Press:
- 31 January 2024, A14
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Path instability of deformable bubbles rising in Newtonian liquids: a linear study
-
- Journal:
- Journal of Fluid Mechanics / Volume 980 / 10 February 2024
- Published online by Cambridge University Press:
- 31 January 2024, A19
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Thanks to Reviewers
-
- Journal:
- The Cognitive Behaviour Therapist / Volume 17 / 2024
- Published online by Cambridge University Press:
- 31 January 2024, e2
-
- Article
-
- You have access
- HTML
- Export citation